Volume 1, Issue 2
May 2021
Management of Mangled Extremities: Upper vs Lower Limb Differences
Syed Asif, Mohammed Al Thaiban, Abdulrahman Alghamdi, Mazen Alqahtani, Ali Al Suliman, Wael Alanazi, Yousef Alharthi, Salah Almatrafi, Sultan Alshammari, Fares Alghamdi, Salem Alsharyah
DOI: http://dx.doi.org/10.52533/JOHS.2021.1104
Keywords: orthaopedics, mangled, extremity, management, lower limb, upper limb
A mangled extremity usually refers to the development of a severe injury to the affected extremity that usually involves the soft tissue, skin, bones, and muscles. As most mangled injuries usually result from severe trauma, they can be associated with life-threatening complications if they are not adequately treated, requiring the integration of clinical decisions that can be lifesaving and may require amputation of the injured limb. In the present literature review, we aim to discuss management approaches to mangled extremities, in addition to the differences between the management of upper and lower limbs. The main steps for managing mangled extremities encompass damage control and fracture management by skeletal stabilization, debridement, and fracture fixation followed by revascularization and fasciotomy of extremity, in addition to nerve repair and debridement of soft tissues. It is important to care for any potential complications as infections may worsen the prognosis of the case. Bone shortening and critical time for reperfusion are two important factors that surgeons should consider when considering upper versus lower mangled extremities.
Introduction
The term ‘mangled’ can be used to describe many events that may eventually result in serious damage to the affected regions. It can be used to describe tearing, cutting and crushing, or a severe injury that will cumulatively result in unrecognizable extremities. A mangled extremity generally refers to the development of a severe injury to the affected extremity that usually involves the soft tissue, skin, bones, and muscles (1). However, according to current literature, many authors also use ‘mangled’ more broadly, including events ushc as open fractures, mutilating or blast injuries, and even amputations.
As most mangled injuries usually result from severe trauma, they can be associated with life-threatening complications if they are not adequately treated. They require the integration of life-saving clinical decisions and may also require amputation of the injured nerve to prevent life-threatening complications (2). Although many advances are now evident in the field of microsurgery, management of mangled extremities remains a great challenge for surgeons, who require sufficient experience to meet success (3). Limb salvage is hard to achieve, and obtaining the past function of the limb is even harder (4). However, it is considered much better than amputations, which are associated with persistence of pain in around 30-79% of the affected patients (5).
Complications for mangled extremities constitute a considerable concern as they can worsen the prognosis and increase the period of treatment. Many complications have been previously reported as infections, which further complicates the injured extremities. Early debridement at the injured site can reduce the incidence of infections. Pulmonary embolism and deep venous thrombosis have also been reported in 2-58% of patients, and therefore, adequate prophylaxis by antibiotics may be required (6-9). Myoglobinuria and rhabdomyolysis can also occur secondary to severe injury, and can be further complicated by renal failure. This litany of complications indicates the urgent need to establish clear management procedures to enhance the prognosis of mangled patients and improve their quality of care and life. Accordingly, in the present literature review, we aim to discuss management approaches for mangled extremities, in addition to the differences between the management for upper and lower limbs.
Management approaches of mangled extremities
The first step of the management process is to assess the severity of the mangled extremity. Many assessment tools and classification systems have been previously proposed. These include the Predictive Salvage Index System (10), the Limb Salvage Index (11), the Mangled Extremity Syndrome Index (1), the Gustilo-Anderson Classification System (12, 13), the Nerve Injury, Ischemia, Soft Tissue Injury, Skeletal Injury, Shock, and Age of the patient (NISSA) Scoring system (14), and the Mangled Extremity Severe Score (MESS) (15). Among these various scoring systems, the Gustilo-Anderson Classification System, and the MESS have been previously studied and well-validated for properly evaluating the severity of mangled cases (Table 1,2). Based on these scores, it has been previously recommended that amputation should be conducted when the score is equal to or exceeds 7 (16-19).
Table 1: Scoring system for the Gustilo-Anderson Classification (12,13)
|
Gustilo-Anderson Classification |
|
|
Type |
Description |
|
Type I |
- Open fracture is transverse or short oblique fracture with minimal communication. - Wound is less than 1 cm with minimal soft tissue injury. |
|
Type II |
- Open fracture is simple transverse or short oblique fracture with minimal communication. - Wound is greater than 1 cm with moderate soft tissue injury. |
|
Type IIIA |
- Adequate soft tissue coverage of a fractured bone despite extensive soft tissue laceration or flaps, or high-energy trauma irrespective of wound size. |
|
Type IIIB |
- Extensive soft tissue injury loss with periosteal stripping and bone exposure. - Usually associated with massive contamination. - Wound requires local or free flap coverage. |
|
Type IIIC |
- Open fracture associated with arterial injury requiring repair, regardless of soft tissue injury. |
Table 2: Scoring system for the Mangled Extremity Severity Score (MESS) (15)
|
Scoring system for the Mangled Extremity Severity Score (MESS) |
Points |
|
Skeletal / Soft-Tissue Injury Low energy (stab; simple fracture; civilian gunshot wound) Medium energy (open or multiple fractures, dislocations) High energy (close range gunshot or military gunshot wound, crush injury) Very high energy (above + gross contamination, soft tissue avulsion) |
1 2 3 4 |
|
Limb Ischemia Pulse reduced or absent but perfusion normal, less than 6 hours Pulse reduced or absent but perfusion normal, more than 6 hours Pulseless; paresthesias, diminished capillary refill for less than 6 hours Pulseless; paresthesias, diminished capillary refill for more than 6 hours Cool; paralyzed; insensate; numb extremity for less than 6 hours Cool; paralyzed; insensate; numb extremity for more than 6 hours |
1 2 3 4 5 6 |
|
Shock Systolic blood pressure always > 90 mmHg Hypotensive transiently Persistent hypotension |
0 1 2 |
|
Age Less than 30 30 – 50 More than 50 |
0 1 2 |
All management steps should be performed in conjunction with obtaining stable hemodynamics and controlled bleeding to prevent any potential complications. When complications are inevitable and bleeding cannot be controlled, amputation is recommended. In the following section, we will discuss the different procedures that are used to manage a mangled extremity.
Damage control and fracture management
Compression is utilized to stop bleeding if it persists following the injury. Tourniquet installation, blood vessel repair, and ligation is also considered when compression fails to stop bleeding. It should be noted that ligation of the blood vessels should not exceed six hours, and revascularization, by constructing a shunt which may be for a damaged artery or both the artery and vein, should be considered after.
Skeletal stabilization and debridement
After assessment of the damage, debridement is performed at the beginning of the surgery for reconstruction of damaged tissue and removal of the foreign bodies and torn pieces. It is undertaken using a low-pressure lavage system, and it is recommended that it is conducted as early as possible to prevent complications, especially infections and amputations (20-22). Following this step, a thorough evaluation of the remaining soft tissue and underlying structures is performed using the Gustilo-Anderson Classification System to assess the severity. However, it is usually hard to assess and grade the severity of the impacted soft tissue structures due to the potential presence of complications, including infection. Accordingly, second and third-look debridement approaches are encouraged. In the same context, skeletal stabilization may be required as the initial management technique for some severe injuries, including those with significant fractures. In these cases, revascularization is also required when a prominent injury to the underlying vessels is observed, and should be done as early as possible to prevent ischemia. Further evaluation is then performed three days after stabilization to decide whether additional debridement and stabilization processes are needed.
Definitive fracture fixation
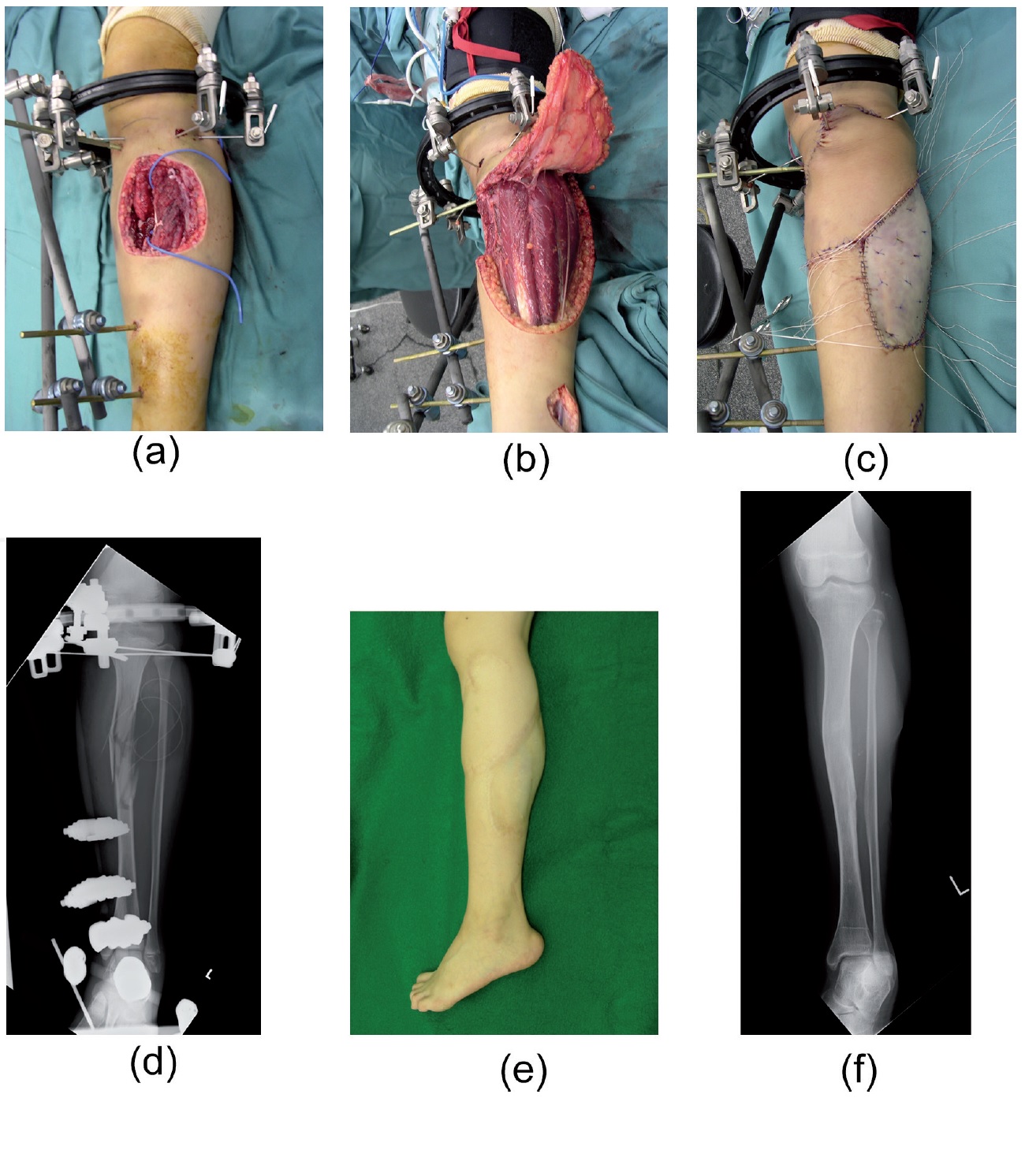
This step should be performed when the patient stabilizes, even if other concomitant injuries are observed. When managing open fractures, external followed by internal fixations and adequate coverage of the soft tissue defects is encouraged. Moreover, in children with mangled extremities, external fixation has been recommended as an efficacious and safe modality for stabilization (Figure 1) (23, 24). Evidence also indicates that intramedullary nailing is recommended, together with fixation of long bones with low-grade fractures. However, it has been observed among studies in the literature that the significance of this technique is still controversial because of the unapparent differences between benefits from the unreamed and reamed nailing modalities (25-27).

Figure 1. External fixation of a mangled lower extremity of a child. A) Shows an open fracture of the left lower extremity with soft tissue defects on the anterior surface, B) A lateral fasciocutaneous flap elevation was conducted, C) Covered soft-tissue defects by a fasciocutaneous flap, with skin grafting done at the donor site, D) Intra-operative x-ray findings, E) An 84-month postoperative real view, F) An 84-month postoperative view (24).
Revascularization and fasciotomy of extremity
Revascularization should be performed less than six hours after ligation to prevent permanent ischemia. However, many factors can result in inadequate management and poor revascularization. These include the period taken to perform revascularization from the time the injury occurred, the length of ischemia, the type of injury, and the affected vessels. Vein grafting, vascular repair, and inserting bypass, shunts, and stents are relevant techniques that are usually performed within the operating room by experienced surgeons. Whenever multiple vascular injuries are observed, their management should be inaugurated from the proximal end to the affected vessel until all injuries are ligated and revascularization is achieved. Considering the formation of shunts should reduce the rate of amputations, whenever revascularization is delayed (28). It has also been previously recommended that surgeons begin vein grafting before revascularization wherever there is a strong tension or significant vessel defect at the site of injury. Venous revascularization should also be indicated in cases of potential problems with venous return.
Ischemia due to swelling of the muscles and fascia can occur secondary to the injury, and causes what is known as compartment syndrome, in which there are potential nerve and muscular injuries. A thorough examination using the present and past histories of the affected patient should adequately assess and diagnose ischemia. Severe pain that does not respond to analgesics and increases with stretch is a significant characteristic. However, peripheral pulsations should still be assessed. Continuous checking of vital signs is recommended within the first two days to assess for complications and life-threatening adverse events. However, if compartment syndrome is suspected, inner pressure measurement should be approached. Fasciotomy is preferred when the measured inner pressure exceeds 35-40 mmHg. Skin grafting and delayed closure are required for the proper management of the fasciotomy.
Nerve repair and debridement of soft tissues
Simple fixation and repositioning of injured nerves is undertaken in cases of mangled extremity injuries. However, this microsurgery should be carefully approached with adequate experience and the equipment necessary to avoid any potential complications. Many factors have been associated with the recovery of the injured nerve, including the age of the affected patient and the severity of the nerve injury. Evidence also indicates that delayed nerve repair can be performed up to two weeks following the injury in cases where severe surgical operation priorities require a delay. In these cases, marking the nerve fibers, which can be done using nylon sutures, is advised. For severely damaged nerve fibers, all damaged fibers should be reunited and innervated. Nerve gaps can also make it hard to complete the process of nerve repair when there is significant tension at the site of the injury, and therefore, artificial nerve conduit or autologous nerve grafting is recommended to complete the management procedure (29, 30).
The severity of soft tissue injury has been previously correlated with the degree of success of management procedures and the prognosis of mangled extremities (31). Previous reports have demonstrated that infections can complicate both immediate and primary wound closure, and therefore, concurrent interventional approaches during the procedure should be considered. However, this can be difficult due to limitations in assessing the severity of the injury and the presence of infections. Negative pressure wound therapy has been recommended for open fracture surgical procedures until coverage occurs and debridement is completed (32). However, the efficacy of this modality and its superiority over conventional moist dressing has not yet been adequately validated (33, 34). Moreover, closing the wound as early as possible after the operation is conducted is preferable as it decreases the chances of catching an infection, on the condition that the patient stabilizes with normal hemodynamics (35, 36). Soft tissue defects are further covered using a flap, which has been previously reported to enhance the prognosis if it has been utilized within three days of the procedure and after debridement (35-38). However, free flap transfer techniques have been previously reported to be efficacious with severe soft tissue injuries, enabling the easy anastomosis of the underlying vessels and other structures due to the wide variability of options available when using the free-flap technique (Figure 2) (24, 39).

Figure 2. Free flap transfer procedure for an extensive soft tissue injury. A) Left lower limb showing an open fracture within the distal compartment, with extensive soft tissue damage, B) X-ray findings intraoperatively after fixation using intramedullary nailing, C) A fasciocutaneous flap was obtained from the anterolateral part of the right thigh, D) The flap was used to cover the soft tissue defects, and bone grafting was done six months after fixation, E) A 12-month postoperative real image, F) A 12-month postoperative X-ray image showing reunion (24).
Differences between the management of upper and lower mangled extremities
Previous studies in the literature have demonstrated differences that should be considered by attending clinicians and surgeons for the proper management of mangled upper and lower extremities. The investigation by Togawa et al. (40) reported that mangled upper extremities need longer critical time for reperfusion than lower extremities (8-10 versus 6 hours). Another potential difference that should be considered is bone shortening, as it has been previously indicated that lower extremity bone shortening, used to decrease defective soft tissue, is not tolerated for more than 2 cm, while shortening of the humerus can be undertaken for up to 5 cm. Reconstruction of the injured nerves within the upper limbs has been reported with favorable success rates, while many clinicians seriously consider amputations of the mangled lower extremity when a significant injury affects the nerve. Gupta et al. (41) also indicates that rehabilitation for upper mangled limbs is more important and crucial than lower extremities. Assessment by the MESS score has also been reported to have successfully predicted amputations in injured upper extremities (42).
Limb salvage versus amputation
Evidence from the current literature indicates that the superiority of limb salvage over amputation is controversial (43-46). Although some investigations reported that the scoring systems may be efficacious when taking the clinical decision (47), others did not support the suggestion (48). If the scoring systems are to be used anyway, they should be carefully interpreted before indicating amputation, and other factors should be considered including the patient’s age, underlying medical conditions, and occupation (49). However, some general indications for amputation have been found in the literature. These include: 1) the open injuries may cause a life-threatening complication, 2) extensive bleeding that cannot be dealt with using ligations and other approaches, 3) there has been a clinical decision by the attending surgeons that salvage cannot be undertaken due to severe underlying injuries. Finally, it should be noted that obtaining consent from the patients and their families is necessary before initiating the amputation procedure, which can be postponed for up to three days following the injury.
Conclusion
In the present literature review, we have discussed the current management approaches and considerations that should be undertaken for mangled upper and lower extremities. It is important to care for potential complications, including infections, that may worsen the prognosis of the case. Bone shortening and critical time for reperfusion are two important factors that surgeons should consider when presented with upper versus lower mangled extremities.