Volume 3, Issue 10
October 2023
Surgical Treatment of Acute and Chronic Facial Paralysis
Hussam Shawly, Faisal Alotaibi, Rawan Alamri, Haitham Sharrahi, Sadeem Zaylai, Salma Khawaji, May Hakami, Weaam Naseeb, Areej Alameer, Abdulelah Alhazmi, Amani Basheri
DOI: http://dx.doi.org/10.52533/JOHS.2023.31007
Keywords: Facial palsy, treatment strategies, multi-disciplinary approach
The assessment and management of facial palsy depend on a comprehensive understanding of three key factors: the duration of the palsy, its anatomical location, and the underlying cause or mechanism. Clinical history and physical examination are the cornerstones for diagnosis, though diagnostic tools like CT scans, MRIs, and electromyography also offer valuable insights. These tools, however, have limitations, particularly in the initial and late stages post-injury. Facial palsy is categorized into acute (0–72 hours), subacute (72 hours up to 12–18 months), and chronic (beyond 12–18 months) phases. Treatment strategies are primarily guided by the mechanism and location of the injury rather than the stage of palsy. Acute injuries may be intratemporal or extracranial, each requiring different approaches. In the subacute phase, surgical interventions like nerve transfers become important. For longstanding facial paralysis, a new neuromuscular unit is often required, with multiple treatment options available. Static procedures offer valuable adjunctive treatments for aesthetic and functional outcomes. Various muscle transplant methods, graft choices, and ancillary procedures are under exploration and offer promise for better outcomes. Overall, the focus remains on a tailored, multi-disciplinary approach for effective management of facial palsy.
Introduction
The face is an essential aspect of an individual's identity and uniqueness. The role of facial expressions is vital in conveying feelings and facilitating social engagement. Therefore, any impairment in the control of facial muscles can lead not only to physical challenges but also to social and psychological difficulties (1). The facial nerve is a mixed nerve carrying fibers from and into three distinct nuclei in the midbrain pons (2). The motor nucleus generates fibers that activate the muscles responsible for facial expressions; the superior salivatory nucleus dispatches early-stage parasympathetic fibers to the tear, sublingual, and submandibular glands; and the solitary tract nucleus takes in sensory fibers from the external ear canal as well as taste fibers from the front two-thirds of the tongue (3). Bell's palsy is the leading reason for one-sided peripheral facial paralysis, a prevalent issue from which a third of patients may experience insufficient recovery, leading to subsequent physical and social challenges (1). Bell's palsy is named after Sir Charles Bell, who lived from 1774 to 1842. While he was the first to outline the anatomical foundations of the condition, modern studies have shown that earlier clinical summaries and reports on the paralysis of the seventh peripheral cranial nerve were actually provided by other European medical professionals (4). The earliest documented case of unexplained facial paralysis is thought to have been published by Nicolaus Friedrich, an 18th-century professor of medicine in Wurzburg. His report detailed the experiences of three middle-aged men who suffered from one-sided facial paralysis that was either acute or subacute in nature and improved over a period of weeks to months. Subsequently, Charles Bell conducted studies on the functioning of the facial nerve in animals. During his surgical work in London, he came across several cases of one-sided facial nerve paralysis. His most famous and frequently referenced case was published in 1828; it involved a man who had been struck by a bull, resulting in permanent damage to his facial nerve (5). The onset of symptoms usually occurs abruptly and can vary in intensity from mild to severe, often reaching their peak between 24 and 72 hours. These symptoms may consist of weakened facial muscles, pain behind the ear, reduced ability to tolerate noise, and disturbances in taste on the same side as the facial weakness (6). In general, the outlook is positive. One study that involved 1,701 Bell's palsy patients found that 1,202 (or 71%) regained normal facial movement without any treatment. Among the 1,189 patients who had complete paralysis, 721 (or 61%) recovered normal facial expressions; the rest did not. Importantly, the chances of fully recovering facial functions dropped significantly after three months. By that time, 64% of patients had regained normal function, but none of those who still had issues after six months saw a return to normal facial movements. Long-term complications in Bell's palsy are considered to be any facial paralysis that continues for more than three months from the time symptoms first appear (7). The main cause is still unknown but is closely linked to specific viral infections that lead to nerve inflammation. This inflammation results in localized swelling, loss of myelin, and reduced blood supply. Various research studies have indicated that some risk factors, such as elevated blood sugar levels (8), uncontrolled blood pressure, advanced pre-eclampsia (9), migraine (10), and exposure to radiation (11) contribute to the disease mechanisms and increase a person's susceptibility to facial paralysis. The resulting weakness can range from total to partial and may come with symptoms like numbness, slight pain, heightened sensitivity to noise, and changes in taste perception. Diagnosis mainly relies on a physical examination and is typically made by ruling out other possible conditions.
Methodology
This study is based on a comprehensive literature search conducted on September 17, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the surgical treatment of acute and chronic facial paralysis. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Injuries to the facial nerve at varying anatomical locations produce different types of impairments. Generally speaking, the farther along the nerve the injury occurs (more distal), the more it results in isolated motor problems and fewer sensory and parasympathetic issues (2). The surgical treatment of facial paralysis calls for the reconstructive surgeon to employ an extensive range of both reconstructive and cosmetic principles. Utilizing a diverse set of surgical techniques, such as microsurgery, peripheral nerve surgery, and aesthetic facial surgery, is essential for enhancing patient results. Table 1 summarizes the different clinical presentations based on the anatomical location of facial nerve injury. Thorough knowledge of facial nerve anatomy is pertinent to diagnosis and optimal treatment planning. This article aims to summarize current knowledge on facial nerve trauma management strategies and offer a practical approach to the majority of traumatic facial palsy patients (2).
|
Table 1. Clinical presentations based on the anatomical location of facial nerve injury |
||||
|
Anatomical Region |
Sub-Location |
Type of Neuron (UMN/LMN) |
Clinical Presentation |
Additional Symptoms |
|
Intracranial |
Pons |
LMN |
Complete facial paralysis on the same side |
Contralateral hemiparesis, ipsilateral abducens palsy |
|
Intratemporal |
Meatal segment |
LMN |
Complete facial paralysis on the same side, diminished taste on the front 2/3 of the tongue, reduced tear production |
Decreased hearing, increased tinnitus, vestibular symptoms |
|
Intratemporal |
Labyrinthine segment |
LMN |
Same-side facial paralysis, reduced tear production, diminished taste on front 2/3 of the tongue, increased sensitivity to loud sounds |
Decreased hearing, increased tinnitus, vestibular symptoms |
|
Intratemporal |
Horizontal segment |
LMN |
Same-side facial paralysis, diminished taste on front 2/3 of the tongue, increased sensitivity to loud sounds |
Decreased hearing, increased tinnitus, vestibular symptoms, no hyperacusis |
|
Intratemporal |
Mastoid segment |
LMN |
Peripheral facial paralysis; if near chorda tympani, loss of taste on front 2/3 of the tongue |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Temporal branch |
LMN |
Paralysis of forehead muscles affecting various facial movements like raising eyebrows |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Temporal & zygomatic branches |
LMN |
Orbicularis oculi muscle affected: gentle or forceful eyelid closure |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Zygomatic & buccal branches |
LMN |
Zygomaticus major muscle affected: corner of the mouth lifts up, aiding in smiling |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Buccal branch |
LMN |
Midface paralysis affecting smiling and blinking |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Buccal & marginal mandibular |
LMN |
Multiple facial muscles affected, mostly related to mouth and lip movements |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Marginal mandibular |
LMN |
Platysma affected: pulls down corners of mouth |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Cervical |
LMN |
Affects muscles related to the outer ear and the occipital part of occipitofrontalis muscle |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Posterior auricular branch |
LMN |
Elevates the hyoid bone |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Posterior head of digastric branch |
LMN |
Elevates the hyoid bone |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Stylohyoid branch |
LMN |
Pulls corners of mouth down and laterally |
Lacrimation, salivation, taste intact, no hyperacusis |
|
Extracranial |
Depressor labii inferioris |
LMN |
Pulls lower lip down and laterally |
salivation, taste intact, no hyperacusis |
|
Extracranial |
Mentalis |
LMN |
Pulls skin of chin upward |
Lacrimation, salivation, taste intact, no hyperacusis |
UMN: Upper Motor Neuron; LMN: Lower Motor Neuron.
"Lacrimation, salivation, taste intact, no hyperacusis" in the additional symptoms’ column indicate that these functions are unaffected.
Clinical presentation and evaluation
In assessing a new case of facial palsy, three fundamental factors must be evaluated: the duration of the palsy, its anatomical location, and the underlying cause or mechanism. A comprehensive history and thorough physical examination serve as the bedrock for diagnosis. In addition to these, various diagnostic tools can also provide valuable insights. These include computed tomographic (CT) scans, magnetic resonance imaging (MRI), electroneurography, and electromyography. Electromyography has been shown to predict unfavorable outcomes with an accuracy of 80.8% in a study of 355 patients, although its role in guiding surgical intervention remains unclear (2). However, it is important to note that the value of electroneurography and electromyography are limited in certain contexts. Their utility is notably restricted in the initial 10 days following the injury, and electroneurography becomes unreliable 21 days post-injury. Given these limitations, while these tools can contribute to the diagnostic process, they may not be universally applicable or reliable in all trauma settings. Therefore, while technological tools offer adjunctive diagnostic support, the cornerstone of evaluation remains a meticulous clinical examination and history-taking.
Amount of time, site, and cause of the injury: impact on treatment approaches
An accurate assessment of both the duration and the prior functional state of facial palsy is essential for effective management. The duration of palsy is generally categorized into three somewhat nebulous phases: acute (0 to 72 hours), subacute (72 hours up to 12 to 18 months), and chronic (longstanding) (beyond 12 to 18 months). The demarcation between acute and subacute stages is not sharply defined. For instance, while stimulating distal nerve branches becomes impractical after 72 hours due to Wallerian degeneration, the management approach often remains similar for both acute and subacute periods. This is because the treatment strategy is primarily influenced by the injury's mechanism and location rather than the stage of palsy. The focus is largely on the salvageability of mimetic muscles. On the other hand, longstanding facial paralysis usually calls for a different therapeutic approach, necessitating the introduction of a new neuromuscular unit. This is due to the irreversible atrophy of mimetic muscles caused by prolonged denervation. Thus, understanding the palsy's duration and mechanism of injury is crucial for tailoring appropriate and effective treatment plans.
Acute facial paralysis (48 to 72 Hours)
Management of acute facial paralysis varies based on the location and nature of the injury.
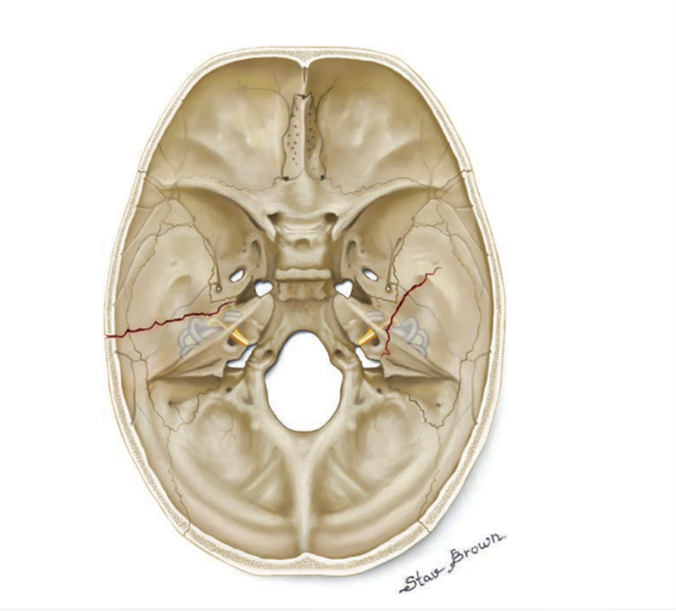
Acute Intratemporal Facial Nerve Injuries
It is often caused by blunt or penetrating trauma; the prognosis is better for longitudinal temporal bone fractures than for transverse fractures (Figure 1) (12-16). Evidence supporting surgical interventions like nerve decompression is limited and inconclusive (17-19). For decision-making, high-resolution CT scans, electroneurography, and electromyography can be useful, although the surgeon's expertise remains paramount (18, 20). Direct nerve repair, or primary neurorrhaphy, is seldom feasible in intracranial injuries due to factors like nerve gaps and tension issues. When it comes to repair techniques, neither suturing nor the use of fibrin glue have been proven superior. In some cases, acute nerve grafting may be considered, although the literature shows poor functional results for immediate intracranial grafting (21).
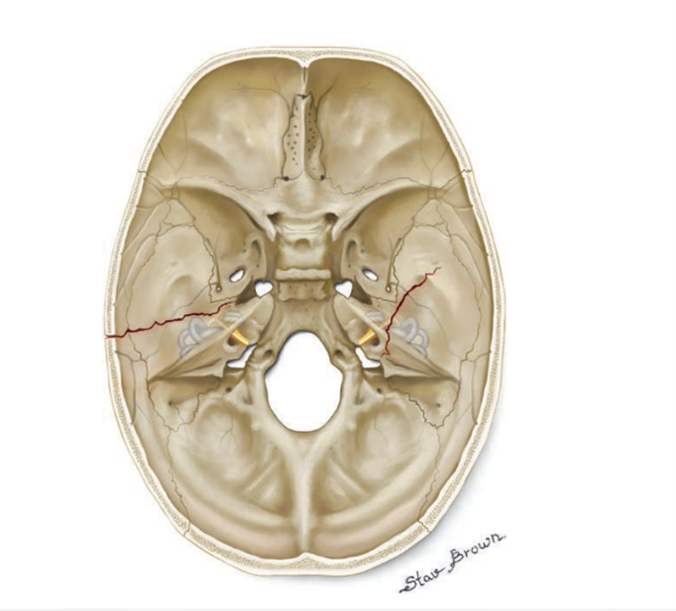
Figure 1: Longitudinal temporal bone fractures on the left versus transverse fractures on the right (2).
Acute extracranial facial nerve injuries
For acute extracranial facial nerve injuries, primary neurorrhaphy is generally the treatment of choice, as it provides the best chances for functional recovery (22). Tension-free coaptation is vital for success. If there is a nerve gap, grafting is indicated (23, 24). Donor nerves, like the great auricular or sural nerves, can be used based on the graft length required. Other options include the medial and lateral antebrachial cutaneous nerves.
Subacute facial paralysis (72 Hours to 12 to 18 Months)
Management of subacute facial paralysis (72 hours to 12–18 months post-injury) demands a nuanced approach shaped by the duration of denervation, type of injury, and patient-specific variables. Although some recovery might occur even after one-year, earlier reinnervation, preferably within 6 months, yields optimal results (25-27).
Intratemporal subacute injuries
Here, options such as nerve decompression and grafting have limited evidence of efficacy. Nerve transfers could be a more viable option in this phase. Early nerve transfers, especially when distal facial nerve branches are intact, help maintain mimetic muscle viability. Immediate cross-facial nerve grafting may avoid revisiting a scarred field, whereas delayed coaptation could increase accuracy in targeted reinnervation.
The anatomical location of the nerve transfer is another factor. More proximal nerve transfers are advised in situations of proximal nerve injuries where there is no hope of healing or continuation of the facial nerve (Figure 2) (2).
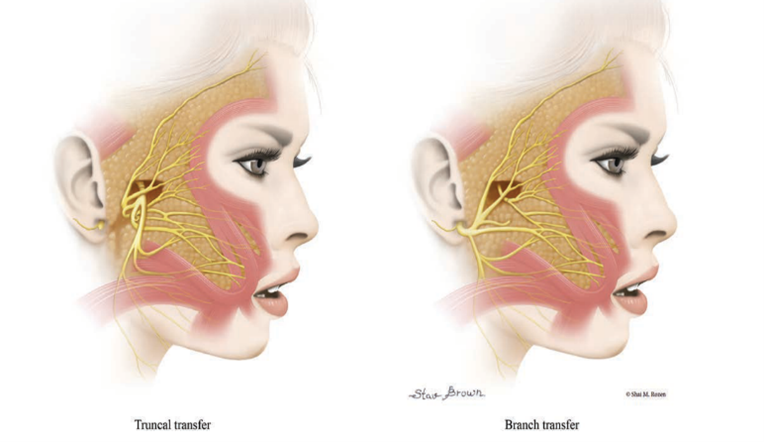
Figure 2: Selective distal fifth-to-seventh nerve transfer in cases with facial nerve continuity versus nonselective proximal fifth-to-seventh nerve transfer when facial nerve continuity is disrupted (2).
Extracranial subacute injuries
Surgical intervention becomes highly recommended if no motion is detected at the 6-month mark. Direct nerve repair is less feasible here due to scar tissue. Ipsilateral nerve grafting may be possible, but it demands a meticulous evaluation of muscle viability, nerve gap length, and injury proximity to the muscle. If combined with ipsilateral nerve transfers, contralateral nerve grafting becomes an option.
Muscle-related paralysis
In high-energy or multilevel injuries, both nerves and muscles could be compromised. Distinguishing the source of paralysis is crucial and is usually carried out clinically. If proximal motion is observed without distal translation, muscle repair should be attempted.
Longstanding (chronic) facial paralysis (>12 to 18 Months)
Managing longstanding facial paralysis (>12 to 18 months) often involves introducing a new neuromuscular unit. The treatment can range from free functional muscle transfers to local muscle transfers. There are two types of muscle transplant methods: two-stage reanimation and one-stage reanimation.
In two-stage reanimation, the first stage involves selecting an ideal facial nerve donor branch and proceeding with a cross-facial nerve graft. Cross-facial nerve grafts have been traditionally considered the gold standard for providing spontaneity in facial reanimation (28, 29). However, recent evidence suggests masseteric and dual-innervation techniques may offer additional benefits like strength and, possibly, synchronicity. The second stage, following axonal growth, which usually takes between 6 and 12 months, involves functional muscle transplantation.
The one-stage method, especially beneficial in trauma settings or for patients wanting a quicker recovery, often utilizes the masseter nerve for neurotization. Younger patients generally fare better than older patients in procedures involving long nerve grafts, owing to more robust axonal loads. Several techniques are under exploration for optimizing these grafts, including specific coaptation points for improved axonal load.
Local muscle transfers often utilize the lengthening temporalis myoplasty (or Labbé procedure), offering the advantage of avoiding microsurgical techniques (30-34). While these offer less excursion than free functional muscle transfers, some degree of spontaneity has been reported. The procedure has its limitations in cases where there is severe scarring or prior irradiation, and an MRI might be essential for planning.
The selection of muscle for grafting is vital; the partial gracilis is often the go-to choice due to its anatomical reliability, low impact on the donor site, and adequate length of the neurovascular pedicle. Other options, such as the latissimus dorsi, serratus anterior, and pectoralis minor muscles, have also provided good outcomes. The dilemma of weighing a limited range of motion with naturalness against a more reliable but less spontaneous movement is still unresolved. However, progress in surgical methods and knowledge of nerve function hold potential for enhancing results.
Static and other auxillary procedures
Static procedures, while lacking the ability to restore movement, play a crucial role in managing facial paralysis. They offer both aesthetic and protective benefits and can be carried out at various stages—before, during, or after dynamic interventions. These static treatments are especially beneficial for older patients (2). Commonly employed methods include the use of springs for addressing paralytic lagophthalmos in the upper eyelid, as well as poralis slings and eyelid weights. Treatments for lower eyelid issues like ectropion can vary, from canthoplasties to tarsal strips, depending on the level of horizontal slackness. Lifting procedures are available for brows affected by paralysis-induced drooping. Static slings for the midface are another option, particularly for treating sagging at the mouth corners and nostrils. Tensor fasciae latae is often the preferred material for these slings due to its autologous nature and adaptability to multiple strips. Other options for lower lip asymmetry include transferring the platysma muscle or using fascial strips. To achieve facial symmetry, injections of botulinum toxin on the opposite side of the face can also be effective. In addition to these, further aesthetic procedures like eyelid surgeries (blepharoplasties), fat grafting, and wrinkle-removing surgeries (rhytidectomies) can and should be used to enhance visual results.
Conclusion
Diagnosing and treating facial nerve damage is a complex endeavour due to the diverse ways it can manifest clinically. Factors such as how long the paralysis has lasted, as well as the injury's location and cause, significantly influence treatment options. The role of supplemental and cosmetic procedures is highly significant; they contribute to optimal outcomes and greatly enhance both surgeon and patient satisfaction. Ultimately, these efforts help patients regain not only external smiles but also inner joy.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.