Volume 3, Issue 10
October 2023
The Use of Lasers in Pediatric Dentistry: Applications, Benefits, and Limitations
Roaa AlDomyati, Raghad Bajaber, Faisal Alrumi, Maram Alghamdi, Abdulkarim Alharbi, Nasser Alsour, Somaya Alhafi, Rawa Alsughayer, Abdulelah Alquwayi, Abdullah Baaboud, Shahad Alshahrani
DOI: http://dx.doi.org/10.52533/JOHS.2023.31009
Keywords: Pediatric dentistry, laser, fluorescence, argon lasers, erbium lasers, and carbon dioxide lasers
The application of laser technology in pediatric dentistry holds immense promise for improving the quality of care and treatment experiences for young patients. Laser technology offers efficient methods for diagnosing and addressing oral and dental issues in children, encompassing both soft and hard tissues. Research indicates that the use of lasers in restorative, pulpal, and surgical procedures enhance children's cooperation and results in better care quality. Different kinds of lasers, including laser fluorescence (LF), argon lasers, erbium lasers, and CO2 lasers, are used in a range of dental applications, such as identifying, preventing, and treating cavities, as well as performing various other dental procedures. Laser technology also offers benefits in endodontics, soft tissue applications, trauma management, pain relief, and orthodontics. However, the implementation of lasers requires specialized training, initial investment costs, and careful infection control measures. Despite these limitations, lasers hold the potential to become a standard approach in pediatric dentistry, revolutionizing the way oral and dental issues are diagnosed and treated in young patients.
Introduction
Laser technology has recently surfaced as a revolutionary instrument within the medical field, holding the potential to improve both diagnostic and therapeutic procedures (1). This innovation finds its roots in the theory of stimulated emission, a concept originally conceptualized by Albert Einstein in 1916. The term "laser" itself is an acronym that stands for "light amplification by stimulated emission of radiation." Although lasers were initially employed primarily for soft tissue incisions, their evolution has seen them gain the capacity to interact with water molecules, enabling them to ablate dental hard tissue. This advancement has introduced fresh avenues for utilizing lasers in dentistry, transforming them into effective instruments for preventing, diagnosing, and treating cavities in various dental specialties. These initial interactions are pivotal in promoting healthy dental practices and creating positive memories for children (2). Here, laser technology shines as a minimally invasive and contemporary approach, significantly reducing the pain associated with dental procedures for young patients. In addition to alleviating pain, lasers demonstrate remarkable adaptability in pediatric dental care by serving as efficient instruments for identifying oral and dental conditions, addressing both hard and soft tissues, and halting the advancement of dental problems (3).
Dental lasers can be classified into four main categories: solid-state lasers, liquid lasers, gas lasers, and semiconductor lasers. Among these, gas lasers have a relatively simpler design, emitting atoms distributed relatively evenly, which allows them to function as continuous-wave lasers when compared to other laser types. Liquid lasers demonstrate the capability to alter their frequency, and semiconductor lasers are popular due to their lightweight nature and high optical output power (3). Dental lasers are available in various types with different wavelengths, and they can operate in continuous-wave, pulsed, or running pulsed modes. The wavelength of a laser determines its clinical applications and device type, with applicable wavelengths ranging from 193 to 10,600 nm in medicine and dentistry.
Methodology
This study is based on a comprehensive literature search conducted on October 10, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the applications, benefits, and limitations of lasers in pediatric dentistry. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Dental lasers have wide-ranging applications in dental procedures, promising innovative and precise treatments for oral health.
Laser application in pediatric dentistry
Encouraging children to make dentist visits a priority is vital for preventing oral and dental problems. Consequently, apart from dental fundamentals, pediatric dentists must be aware of modern technology. Laser technology offers an efficient method for diagnosing and addressing oral and dental issues in young patients, covering both soft and hard tissues (3, 5).
Research has shown that utilizing lasers in restorative, pulpal, and surgical procedures enhances children's cooperation, resulting in better quality of care and treatment experiences (5, 6). The expectation is that lasers will soon become the standard approach in pediatric dentistry. Pediatric dentistry involves various types of lasers designed for specific applications.
|
Table 1. Common types of dental lasers and their uses (4). |
|||
|
Laser Type |
Wavelength |
Mode |
Application |
|
CO2 |
10 600 nm |
Pulse or continuous-wave |
|
|
Nd:YAG |
1064 nm |
Pulse |
|
|
Er:YAG |
2940 nm |
Pulse |
|
|
Er,Cr:YSGG |
2780 nm |
Pulse |
|
|
Argon |
572 nm |
Pulse or continuous |
|
|
Diode |
810 or 980 nm |
Pulse or continuous-wave |
|
|
HO:YAG |
2100 nm |
Pulse |
|
Detection of dental caries
The accurate detection of dental caries is essential for dentists to perform appropriate and efficient tooth restorations while saving time and costs (3). Numerous studies have highlighted the enhanced precision and efficiency of clinical caries detection achieved through the use of laser fluorescence (LF). LF, which utilizes a non-ablative red light with a wavelength of 655 nm, serves as an additional method for identifying occlusal surface caries in both primary and permanent teeth (7). Its high reliability, predictability, and reproducibility contribute to a reduction in diagnostic errors. In laboratory studies, the commercial product DIAGNOdent, employing LF technology, has demonstrated superior effectiveness in caries detection. In contrast to visual examination, probing, and radiographic methods, laser fluorescence (LF) has demonstrated clear benefits in the detection of occlusal dentin caries in primary teeth. Earlier studies have also indicated that LF provides similar or even better precision than bitewing radiography when it comes to spotting caries and cavities in the proximal areas of primary teeth. Nevertheless, the effectiveness of LF depends on the depth of the carious lesion; it shows greater accuracy in identifying dentin caries compared to enamel caries. However, it is less reliable when it comes to detecting initial enamel caries and tooth demineralization (8).
A different diagnostic laser, known as the argon laser, functions at a wavelength of 488 nm (in the blue-green color range) and relies on fluorescence characteristics to identify caries, particularly in the interproximal and occlusal surfaces of teeth. The quantitative-light induced fluorescence (QLF) method has shown superior effectiveness in quantitatively detecting demineralization in primary teeth, surpassing its performance in permanent teeth. QLF also provides the benefit of being able to detect caries beneath pit and fissure sealants during regular and periodic dental examinations.
Caries prevention
Numerous studies have explored the utilization of various laser wavelengths, either on their own or in conjunction with fluoride gel or varnish, to alter the superficial enamel structure to enhance the tooth's resistance to acid damage (9-13). However, it is essential to emphasize that additional long-term clinical investigations are required to substantiate the effectiveness of this approach before it can be widely adopted in preventive dentistry. Laser technology offers a valuable method for preparing tooth surfaces before applying pit and fissure sealants (14). It serves a variety of functions, including preparing, cleansing, and sterilizing pits and fissures.
Molar-incisor hypomineralisation (MIH) treatment
In the context of treating molar-incisor hypomineralisation (MIH), the available literature on the application of erbium lasers is limited, primarily consisting of a few case reports. The current approach to MIH treatment involves a minimally invasive strategy that focuses on strengthening and safeguarding the existing dental structure, with restorative treatment reserved for the most severe cases (15). However, there is potential for erbium lasers to enhance the uptake of fluoride and increase enamel resistance, as suggested by previous research (9-12). Moreover, when dealing with severe MIH lesions, erbium laser preparation offers advantages due to its minimal and favorable modifications of dental tissues, along with the reduced discomfort it causes, making it a viable elective procedure for children (16).
Caries removal and cavity preparation
Over the past 25 years, researchers have extensively studied laser settings for tooth preparation, assessing their effects on both hard dental tissues and the pulp. In recent years, interest has been resurgent in the 9,300nm wavelength of CO2 lasers for ablating both hard and soft tissues. However, further research is needed to validate this new technology before its introduction into pediatric dental care (16).
The interaction between erbium lasers and primary enamel and dentin depends on the water and mineral composition of these tissues. The lower presence of hydroxyapatite and higher water content in primary teeth mean that less energy is required for laser ablation of primary enamel and dentin. Studies have assessed the effectiveness of the Er:YAG laser for caries removal in children and its safety for the pulp in both primary and permanent teeth. Due to the laser's ability to deeply decontaminate infected dentin, it is believed that a deeper and softer layer of dentin can be left to remineralize, allowing for maximum preservation of dental structure (17).
Comparing different dentin excavation methods in deciduous teeth, it was found that the erbium laser group exhibited a lower level of over-preparation compared to the steel bur group, confirming the minimally invasive nature of laser-based approaches. Furthermore, when compared to bur preparation, the Er:YAG laser was found to be less effective but equally efficient in caries removal at the pulpal wall of primary molars (18). The level of decontamination of affected dentin in the pulpal wall was similar for all methods (19).
The use of different laser wavelengths in endodontics is widely reported in adults, but few studies refer to primary teeth. Lasers can be used for vital and nonvital pulp therapies such as pulpotomy and pulpectomy.
Laser pulpotomy
Pulpotomy is a widely employed procedure for primary teeth, and laser treatment has been suggested as an alternative to substances like formocresol and ferric sulfate.
Moreover, in vitro studies assessing the antimicrobial effectiveness of diode lasers, as compared to triphala and sodium hypochlorite, against Enterococcus faecalis-contaminated primary root canals have revealed a significant reduction in colony count in the laser-treated group compared to the other groups (20, 21). Laser pulpotomy has also been found to excel in terms of operating time, patient cooperation, ease of use, and pain management. However, it is important to note that the choice of different capping materials remains a critical aspect of this procedure (22).
Laser pulpectomy
Soares et al. conducted a study comparing the cleaning and shaping of root canal walls in primary teeth using the Er,Cr:YSGG laser as well as manual and rotary instruments (23). Their findings revealed that the laser technique was notably quicker in completing the cleaning and shaping process compared to both rotary and manual instruments. Moreover, the laser method produced cleaning results similar to those achieved with rotary instrument preparation and was superior to manual instrumentation.
Soft tissue application of laser
Laser technology represents a safe and efficient treatment alternative for a variety of periodontal conditions in pediatric patients (18). Unlike traditional approaches, laser therapy eliminates the risks associated with allergic reactions and bacterial resistance. It can be used for gingivectomy, gingivoplasty, and operculectomy (Figure 1) without requiring local anesthesia, leading to minimal bleeding (5, 24).
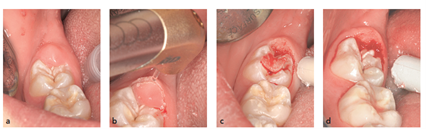
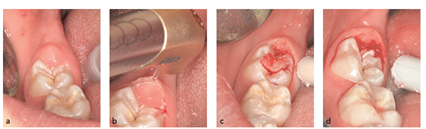
Figure 1: (a) A painful gingival operculum overlapping the mandibular right second molar in a 12-year-old boy. (b) An Er,Cr:YSGG laser was used to perform the operculectomy at a very low power of 0.75 W and 15 Hz with water spray. No anesthesia was used. (c and d) Note the limited bleeding and the clean laser incision without signs of thermal damage (25)
Beyond its use in periodontal care, laser treatment offers numerous advantages in pediatric dentistry. It can assist in addressing abnormal gingival lesions resulting from tooth movement, managing drug-induced gingival hyperplasia, removing fibromas, and treating various oral conditions like aphthous lesions, herpes labialis, mucoceles, and pyogenic granulomas. Laser procedures can also be utilized for aesthetic purposes.
When dealing with infants who have tight maxillary frenums or severe ankyloglossia, frenectomy procedures can be performed using Er:YAG lasers. Furthermore, CO2 lasers are efficient in eliminating vascular tumors in the oral cavity and addressing cyclosporine-induced gingival enlargement. Compared to traditional surgical scalpels, CO2 lasers offer advantages such as disinfection and coagulation.
In micro-gingival surgery for traumatic injuries to unerupted teeth, laser technology, particularly erbium lasers, allows for the removal of gingival tissue covering cervical carious lesions, providing an alternative to conventional methods (26). Moreover, studies have indicated that low-level laser therapy (LLLT) can accelerate the process of orthodontic tooth movement. Laser or light-emitting diode (LED) treatments can also assist in shortening the duration of herpetic lesions and facilitating healing in children dealing with conditions like primary herpetic stomatitis.
Trauma and vitality testing
Injuries to teeth can have detrimental effects on pulp vitality, both in the short and long term (14, 19). Laser Doppler flowmetry (LDF) provides a non-invasive and accurate method for measuring pulp blood flow (PBF) and assessing pulp vitality. This painless procedure is well-tolerated by children. LDF is also valuable in tracking revascularization processes and assessing the condition of mobile teeth.
Laser technology serves a variety of purposes in the treatment of traumatized teeth (27). It can be used to prepare fractured tooth edges before restoration. Laser treatment is effective for coagulating exposed pulp, performing a pulpotomy, and, when necessary following dental trauma, a pulpectomy (using erbium lasers). Moreover, Er:YAG and Er,Cr:YSGG lasers can be utilized to seal dentinal tubules, especially in cases of fractured teeth or open tubules. This effectively decreases tubule permeability and alleviates tooth hypersensitivity. Beyond their dental uses, lasers can also play a valuable role in treating soft tissue injuries, facial wounds, and swelling. The application of laser or LED therapy to these areas can help alleviate symptoms and expedite the healing process. Additionally, laser therapy can be employed in severely traumatized regions to reduce post-traumatic discomfort.
The analgesic effects and relief of pain and discomfort
Laser technology offers significant advantages in pain management for dental patients, reducing the need for local anesthetics (28). Research has shown that using lasers in near-infrared wavelengths (803-980 nm) with a non-concentrated mode can induce anesthesia by hyperpolarizing nerve fiber membranes, providing pain relief for approximately 15 minutes.
As an example, a 660 nm probe has shown a success rate ranging from 50% to 75% in achieving anesthesia while preparing class II cavities in primary molar teeth, eliminating the need for anesthesia injections. In orthodontics, CO2 lasers can be applied locally to alleviate pain caused by orthodontic forces, providing relief to patients. Additionally, low-level laser therapy (LLLT) has been found to expedite the movement of orthodontic teeth without causing any adverse effects. Laser or LED irradiation near the orthodontic site or temporomandibular joint has proven to be effective in relieving pain. LLLT can also be utilized for pain management during the eruption of primary or permanent teeth by targeting lymph nodes (29). Laser irradiation (at 4 to 6 J) of exposed primary teeth has successfully reduced pain. Moreover, LLLT can effectively reduce the initial inflammatory response, with a dosage of 3 to 4 J being suitable for alleviating pain and swelling in cases of lip and anterior teeth trauma.
Exposure of unerupted teeth
In orthodontic treatments that involve the exposure of unerupted teeth, various lasers such as Er,Cr:YSGG, Er,YAG, diode, and Nd:YAG lasers can be utilized. Among these options, erbium lasers are well-known for their effectiveness in removing both soft and hard tissues. However, when employing erbium lasers to expose unerupted teeth for orthodontic purposes, there is a potential risk of damaging the enamel at the surgical site.
Conversely, diode and Nd:YAG lasers, which operate at specific wavelengths, eliminate the risk of enamel damage, making them safer choices for these procedures.
Benefits of Lasers
The benefits of the use of lasers in medical procedures offer a multitude of significant benefits. These include unparalleled precision and selectivity, which enhance surgical accuracy; the ability to generate minimal thermal damage to surrounding tissues, reducing potential harm; the promotion of hemostasis and quicker wound healing without the need for sutures; a reduction in postoperative discomfort, edema, scarring, and the reliance on pain-relief medications; the elimination of local anesthesia and sutures in soft tissue treatments, simplifying procedures; decreased operator chair time and mitigation of inconveniences such as vibrations, noise, smell, and anxiety; decontaminating and bactericidal properties that decrease the need for post-operative antibiotics, thereby improving infection control; and finally, the capacity to provide pain and inflammation relief in various conditions without the use of pharmaceutical interventions, enhancing patient comfort and recovery. These advantages collectively make lasers an invaluable tool in modern healthcare, benefiting both patients and healthcare providers alike (30).
Firstly, there is a requirement for additional training and education for clinicians to effectively use lasers across various clinical applications and tissue types, highlighting the importance of ongoing professional development. Secondly, the high initial costs associated with purchasing equipment, implementing technology, and investing in education and training can be a significant barrier to adoption. Additionally, the need for different wavelengths for various procedures may necessitate practitioners to invest in multiple lasers, further adding to the financial burden. The use of wavelength-specific protective eyewear is essential for both operators and observers during laser procedures to prevent potential eye damage. Strict infection control protocols, including the use of high-speed suction, are necessary to manage vaporized aerosol containing infective tissue particles, ensuring the safety of both patients and healthcare professionals. Lastly, caution must be exercised when treating viral lesions in immunocompromised patients due to the potential risk of disease transmission through laser-generated aerosol, and pharmacological therapies may be a preferable alternative in such cases. Overall, while lasers offer significant benefits, addressing these limitations is crucial for their safe and effective integration into medical practice (30).
Conclusion
Laser technology offers numerous advantages and versatile applications in the field of pediatric dentistry, providing a viable alternative to traditional procedures. It proves beneficial in various dental applications, including caries diagnosis and removal, pulp therapy, infection control, inflammation and swelling reduction, minimal bleeding, promotion of soft tissue healing, pain relief, and even the reduction of the gag reflex in children. The minimally invasive nature of laser treatments often enhances children's cooperation, leading to increased satisfaction levels for both children and their parents.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.