Volume 3, Issue 10
October 2023
Indications, Evaluation, Technique and Complications of Otoplasty
Ashraf Abduljabbar, Roaa Alkanderi
DOI: http://dx.doi.org/10.52533/JOHS.2023.31011
Keywords: otoplasty, indication, complication, procedure
Protruding ears are one of the most prevalent congenital auricular anomalies, with significant behavioural and psychological consequences. The management of protruding ears has developed over time and currently involves a wide variety of cutting-edge surgical methods. These procedures have undergone constant improvement to maximize aesthetic outcomes while also reducing the necessity of surgical revision. Otoplasty is a surgical procedure that uses long-lasting sutures to alter the location, size, or form of the ear. Prominauris, or protruding ears, are the primary indication of otoplasty. Several techniques—almost over 200—are described for otoplasty procedures, among which the majority of technical advancements are only slight adaptations of methods that were first published 40–50 years ago. These procedures are broadly classified as cartilage-cutting or cartilage-sparing procedures. Like any other surgical procedure, otoplasty has related risks and complications; however, they are relatively rare and quite few. The complications of otoplasty can also be classified into early and late complications, depending on the time of presentation. Hematoma, hemorrhage, and postoperative infections, including perichondritis, dehiscence, and skin necrosis, are some of the early complications of otoplasty. Excessive scarring, suture extrusion, hypersensitivity, keloids, and the telephone ear are a few of the late complications. However, overall, otoplasty is considered a safe and effective procedure. The purpose of this research is to review the indication evaluation technique and complications of otoplasty, for which a comprehensive literature search in various databases, including PubMed, ScienceDirect, Web of Science, and Cochrane Library, was performed.
Introduction
Around the globe, almost over 10% of the general population has prominent ears and other ear abnormalities, which are some of the most prevalent congenital deformities of the head and neck (1). Prominauris, or protruding ears, is the most common congenital malformation of the external ear and is distributed in an autosomal dominant manner with varied penetrance. It is believed that up to 5% of the population has prominauris. This anatomic defect normally does not result in any physiologic change about hearing. Underdevelopment of the antihelical fold and an increase in conchal bowl depth are the two most frequently occurring anatomical defects that cause ear prominence. The need for surgical treatment is frequently driven by the prominauris' detrimental psychosocial effects, which result from name-calling, bullying, and ridicule among adolescents and children. The stress and anxiety introduced by these psychosocial stresses might cause anxious and aberrant conduct and a loss of concentration (2, 3).
Numerous auricular malformations, such as the prominent ear, the constricted ear, Stahl's deformity, and cryptotia, among others, can be corrected with otoplasty procedures. For the correction of these malformations, several procedures and methods have been devised, including ones that remove, bend, stitch, scrape, or move the auricular cartilage. The diversity of methods suggests that there doesn't appear to be a single, unambiguously effective method for solving these issues (4). Otoplasty refers to the surgical correction of the ears. Although there are over 200 otoplasty treatments, the majority of technical advancements are only slight adaptations of methods that were first published 40–50 years ago. These procedures are broadly classified as cartilage-cutting or cartilage-sparing procedures. In recent times, several methods seem to incorporate a combination of both. Several popular techniques have recently undergone retrospective assessments, and each has proven to be trustworthy and effective with very less morbidity, making otoplasty a safe and efficient procedure. The last several years have also seen a number of technical changes and advancements. With its foundation in time-tested methods, the otoplasty technique is continually being improved. Today's frequent trend in otoplasty is the adoption of a graded approach that combines components of different procedures (5).
The generally acknowledged objectives of otoplasty have been well-described and include reducing ear prominence and protrusion, creating an antihelical fold, restoring superior crus when absent or effaced, and bringing the lobule into proportion with the rest of the ear. Any surgical procedures must also allow for symmetry and achieve a natural-looking auricle while eliminating the appearance of pinned ears. Commonly performed techniques include variations of the Masturdè, Furnas, and Stenstrom cartilage scoring procedures (6). Like any other surgical procedure, otoplasty has related risks and complications; however, they are relatively rare and quite few (7). With the frequency of haematoma or infection ranging from 0% to 15.6% and 0%-10%, respectively, there is a wide range of reported post-operative outcomes for otoplasty. Other complications of otoplasty include skin/wound healing problems suture-related complications, scars, pain and itching, revision operations, and recurrence (8). The indications or need for revision otoplasty primarily include recurrent prominence/under correction, distortion of the scaphoid fossa, distortion of the antihelical fold, hypertrophy of the conchal bowl, and telephone ear (9).
Otoplasty plays a significant role in improving both the physical appearance and psychological well-being of patients. It also contributes to the advancement of medical knowledge, surgical techniques, and ethical considerations in the field of plastic surgery. Therefore, in this review, we aim to assess the evaluation and indications for otoplasty and describe various techniques used to perform otoplasty. Additionally, report complications associated with these procedures in light of existing literature, which can further aid in an elaborate and comprehensive understanding of otoplasty in all these domains, signifying its importance.
Methodology
A comprehensive literature search in the PubMed, Web of Science, Science Direct, and Cochrane databases utilizing the medical topic headings (MeSH) and relevant keywords such as ‘Otoplasty’, ‘indications’, ‘reasons’, ‘evaluation’, ‘techniques’, ‘approach’, ‘complications’, ‘adverse events’ and a combination of all available related terms was performed on October 16, 2023. All relevant peer-reviewed articles involving human subjects and those available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, or participant age.
Discussion
In most cases, protruding ears appear at a young age. However, the right timing for corrective surgery should balance the patient's maturity level, auricular growth, cartilage pliability, and the psychological burden imposed by the auricular deformity. These factors come into perfect alignment between the ages of 4 and 6 and allow for the best application of reconstructive procedures to enhance the ear's cosmesis (3). Certain aspects of otoplasty are discussed below.
Indications and evaluation
The primary indications for otoplasty include prominent ears or protruding ears, shell ears (undeveloped helical rims), macrotia, Stahl's ears, restricted ears, cryptotia, and question mark ears (10). A comprehensive evaluation of the deformity, its relation to normative guidelines, and the pursuit of symmetry are essential components of the otoplasty procedure. The algorithmic use of cartilage-sparing procedures appropriate for the particular deformity can begin once the patient is deemed to be sufficiently mature. This method can maximize the outcome in terms of form and symmetry while also correcting the prominent ear (11). Moreover, the best course of action for the surgeon is to thoroughly examine protruding ears. To ensure that no divergence from the norm in auricular dimensions is missed, an objective method must be used. With precise preoperative measurements, the surgeon can reduce post-corrective surgical dissatisfaction caused by asymmetry or size distortion. Ear size, position, projection, rotation, shape, and symmetry are the most crucial anatomical factors for surgical planning when evaluating ear architecture. The dimensions of the auricle dictate ear size. The superior border of the helical rim and the lateral brow are the first and inferior borders of the lobule, and the nasal columellar base, respectively, are the second horizontal distances used to determine ear position on the scalp. To assess the level of ear prominence, a three-dimensional study of ear projection is essential. The two criteria most frequently employed to describe ear projection are the auriculocephalic angle and the helix-to-mastoid distance throughout the entire auricular rim. Since anomalies in these two features are the main causes of the projecting ear, special care must be taken when inspecting the antihelix and conchal bow (3).
Techniques employed for Otoplasty
Modern otoplasty procedures can be divided into two broad surgical categories: cartilage-sparing and cartilage-cutting (12). These procedures, however, have diverse variations and subcategories. Some of these procedures are briefly described below:
Cartilage-sparing
In order to reduce the risk of complications and produce an aesthetic result that seems natural, a unique suture-based approach for cartilage-sparing has been developed. A conchal bulge, which may otherwise develop if no cartilage is removed, is avoided using this technique, which is based on two to three critical sutures that shape the concha into its ideal natural form. The two fundamental objectives of otoplasty are accomplished by these sutures, which also support the neo-antihelix made by four additional sutures anchored to the mastoid fascia. The surgical procedure is reversible if necessary due to the preservation of cartilaginous tissue. Additionally, anatomical distortion, pathologic scarring, and persistent surgical stigmata can also be avoided. In the years 2020 and 2021, 91 ears weretreated using this method, and just one (1.1%) of those ears needed revision (13). Figure 1 shows antihelical fold creation with cartilage-sparing techniques to lessen ear prominence (14). Ferzli et al. reported that numerous improvements to the cartilage-sparing otoplasty procedure have been documented since it was first introduced. Recent studies have shown that these treatments produce better results than cartilage-invasive ones; nonetheless, each patient must be treated individually, and the best aesthetic results frequently call for a combination of both (15). Similarly, Smittenberg et al. concluded that, according to the views of different groups, the cartilage-sparing approaches produce a more aesthetically pleasing result. However, the results from their study further demonstrated that patients who have had procedures using cartilage-sparing or cartilage-cutting techniques experienced equal levels of complications and the need for additional surgery (16).
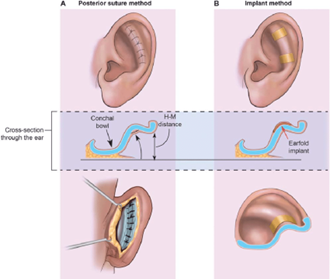
Figure 1: Antihelical fold creation with cartilage-sparing techniques to lessen ear prominence (14)
Mustardé technique
In 1963, Mustardé introduced an otoplastic procedure designed for reshaping the antihelical fold in children with delicate or thin ear cartilage. The goal of this technique is to achieve optimal symmetry in the corrected ears, which is assessed by measuring the distance between the ear and head using Wodak's criteria both before and after the surgery. To perform the procedure, a skin incision is made behind the ear, approximately 8-10 mm below and parallel to the helical rim. The skin overlying the cartilage is gently mobilized downward to the mastoid region and upward to the helical rim. It's essential not to overextend this mobilization to avoid postoperative skin distortions. During this process, the perichondrium as well as the auricular cartilage itself remain intact. The new antihelical fold is created and nonabsorbable mattress sutures, typically made of materials like Goretex 4.0, are placed at the marked locations. These sutures are inserted through the auricular cartilage and perichondrium using a retroauricular approach without penetrating the front skin. The knots of these sutures can be turned inward to prevent them from protruding later. If excess skin needs to be removed, a crescentic excision can be performed, but care should be taken to avoid excessive tension to prevent the formation of postoperative keloids. Figure 2 shows a pictorial representation of the Mustardé suture technique (17).
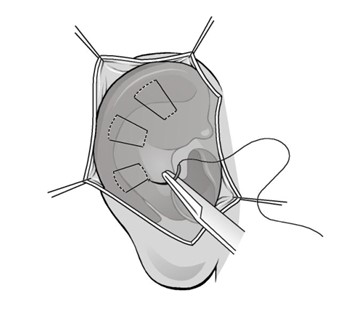
Figure 2: Mustardé suture technique (17)
One of the most common approaches to cartilage-sparing is the Mustardé technique. By generating and anchoring an antihelical fold with 2-4 horizontal mattress fixing sutures, mustardé sutures cure conspicuous ear deformity. Regarding efficacy/safety profiles, postoperative complications, patient satisfaction scores, andoverall resource utilization, the Mustardé otoplasty technique continues to be a leader among otoplasty procedures that have been documented in the literature. With short operating times and low overall case costs, it is in fact proving to be a good, swift, and affordable option for treating the prominent ear (18). Similarly, Eryilmaz et al. reported that no complications, such as internal suture bowstringing, hemorrhage, or infection, were noted. High levels of patient satisfaction with the outcomes were reported. Technical errors are extremely unlikely with this technique, which is an easy, simple, and rapid procedure to perform. These benefits make this procedure a dependable otoplasty technique (19).
Cartilage-cutting
Techniques for cartilage-cutting and cartilage-preserving sutures have been described to replicate the antihelical fold. Cartilage-cutting procedures are now used for thicker, rigid auricular cartilage that needs acute dissection to regulate location better. The authors further described various techniques of this approach from the literature like Ozturan and colleagues defined that older patients may benefit more from cartilage-cutting procedures because their cartilage becomes stiffer and less malleable as people age. Converse and associates explained how to position the superior ear at a desirable distance from the mastoid by suturing a tubed cartilaginous strip. Pitanguy and colleagues described performing parallel full-thickness incisions in the targeted antihelix region to form a cartilage strip island. The strip is then projected laterally to generate the antihelical fold by joining the underlining cartilage margins deep into the island. Farrior described the utilizatintoion of a combination of full- and partial-thickness incisions to restore the superior fold while reducing angular external abnormalities (20). However, patients who underwent cartilage-cutting procedures tended to experience a higher risk of revision and lingering postoperative stigmata (21). Similarly, Cihandide et al. stated that the increased risk of hemorrhage, skin necrosis, and ear deformity associated with cartilage-cutting techniques has led to criticism of them and therefore cartilage-sparing techniques are preferred (22). Figure 3 illustrates the creation of an antihelical fold and the reduction of ear prominence by cartilage-cutting and sculpting techniques (14).
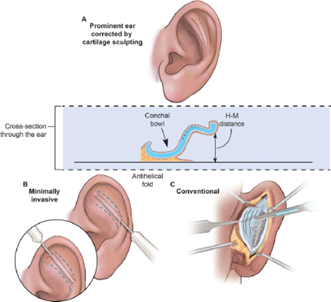
Figure 3: Creation of antihelical fold and reducing ear prominence by cartilage-cutting and sculpting techniques (14)
Conchal cartilage excisions
Procedures including cartilage excisions, scoring-incision techniques that weaken cartilage, and suture techniques are all available to reduce the height and/or size of the concha or the cavum conchae. These concha excisions can be carried out via an anterior approach with a combined cartilage-and-skin excision or by a retroauricular access with little skin disruption. Regarding the benefits and drawbacks of the anterior approach and posterior method, there is currently limited evidence. Converse provided a description of an excision procedure via a retroauricular approach in 1955. He recommended a spindle-shaped cartilage strip excision to reduce the concha while sparing the anterior perichondrium. While Stenström used anterior access to reveal and score the antihelical cartilage while simultaneously reducing the concha using an anterior excision with a spindle-like structure (17, 23, 24). One Conchal reduction method, including posterior suturing is shown in Figure 4 (25).

Figure 4: Conchal reduction method including posterior suturing. (Left) An incision is made to the lateral aspect of the conchal bowl; (Center) the contralateral conchal bowl is partially removed after the ear prominence has been adjusted with a nger; and (Right) the cartilage is sutured (25).
Cavum rotation and fixation
Vargas suggests that there should be a 20–30-degree angle between the mastoid and the helical rim. Due to conchal bowl hyperplasia, this angle can reach 90 degrees in protruding ears. In addition to the methods for antihelix development, it is frequently necessary to decrease the cavum-mastoid angle to return the ear to the cranial bone. To do this, a retroauricular incision is first made along and parallel to the helical rim, and the posterior portion of the cartilage is then prepared in a caudal direction up to the mastoid plane. The extra connective, fatty, and muscle tissue in the retroauricular region is removed, leaving the temporal fascia entirely unharmed (26, 27). Figure 5 shows an illustrative description of the cavum rotation technique (17).
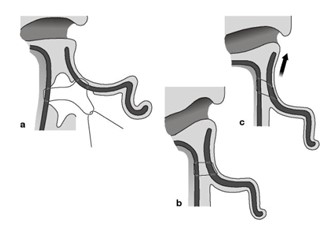
Figure 5: cavum rotation technique. a) adipose and connective tissue in the retroauricular region is removed, b) the temporal fascia is prepared, and c) the cavum is rotated and fixed (17).
Complications of otoplasty
After an otoplasty, complications may arise immediately or up to two weeks later. The complications of otoplasty can be categorized into early and late complications (28).
Early Complications
Post-operative haemorrhage/haematoma
Once the local anesthetic's vasoconstrictive effects have worn off, bleeding may happen after surgery if the proper hemostasis is not obtained before closure or if there is post-operative trauma. It is best to diagnose occult coagulopathies prior to surgery with a comprehensive medical history and physical examination. Intense pain is one of the hallmark indicators of a post-operative hematoma, which is especially alarming if it manifests unilaterally or asymmetrically. To avoid complications of wound infection, perichondritis, or chondritis, all of which can result in dreadful anatomical deformity or cauliflower ear, this should be treated with prompt investigation to eliminate the hematoma and attain hemostasis (29).
Infection
As with many surgical sites, infection following otoplasty often manifests 3 to 4 days after the procedure. Infection occurs between 2.4% and 5.2% of the time. Infection frequently manifests as obvious erythema, edema, or drainage, or the patient may complain of exorbitant levels of discomfort in comparison to the physical examination results. Simple cellulitis to more severe infections like perichondritis or chondritis, the latter of which can significantly distort the auricle, can all fall under the umbrella of infection. Parenteral antibiotics should be used to treat both Pseudomonas aeruginosa and gram-positive organisms when there is an infection. If necrosis has occurred, tissue debridement may also be required (30, 31). The risk of postoperative infection can be decreased with the use of postoperative antibiotic ointment, appropriate preoperative sterile preparation, administration of peri-operative intravenous antibiotics, and sterile and precise intraoperative surgical technique (29).
Late complications
Keloid and hypertrophic scarring
Certain individuals have a susceptibility to developing hypertrophic scars, particularly those with darker skin pigmentation and those who have a personal or familial history of the condition. All patients should get appropriate preoperative counselling to advise them of the risks of scarring. However, this problem can be avoided by carefully designing incisions, reducing stress at closure, and preventing infection. If keloids develop, they should be treated conventionally. To reduce the level of hypertrophy, intralesional triamcinolone (40 mg/mL) injection may be employed; nevertheless, more severe or resistant scarring may call for excision, radiation, or pressure dressings (32).
Loss of correction
With a prevalence of 6.5% to 12%, this complication is one of the more prevalent. The method utilized to fix the protruding ears has the greatest influence on the loss of correction. The highest rate of recurrence will result from skin-only excision in terms of setbacks. Furthermore, failure to overcorrect at the time of surgery, incorrect suture placement, placement of insufficient sutures that result in greater tension and a cheese wire effect across the cartilage, and placement of insufficient sutures all contribute to recurrence. The anterior perichondrium should be fully penetrated during the placement of mattress sutures. As a result of improper positioning, the cartilage may experience a cheese wire effect. Some people might have cartilage that is robust and has a significant inherent memory. If this isn't addressed with other strategies like scoring, it could result in rectification loss within a few months. Last but not least, post-operative trauma can result in the breaking of sutures, which can prevent or disrupt healing (21, 29). Our study provides an extensive understanding of the otoplasty procedure; however, several other techniques and complications of otoplasty could not be discussed in this study since it is beyond the scope of this paper to discuss all techniques and complications of otoplasty and is a limitation of this study. However, we aim to address them in our successive research studies. Additionally, future research on otoplasty in the context of modern medicine and technology needs time.
Conclusion
Otoplasty is a safe and effective procedure for the treatment of protruding ears, and several techniques for otoplasty procedures exist and are practiced, each of which has its own set of advantages and limitations. However, in the literature, cartilage-sparring techniques are preferred more. Future developments in tissue engineering and minimally invasive technologies will probably open up even more opportunities to treat auricular abnormalities, which can further reduce the risk of complications associated with otoplasty.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
