Volume 3, Issue 12
December 2023
Etiology, Histopathology, Staging and Complication of Wilson Disease
Samar Alharbi, Saleh Bajahlan, Hassan Almohsin, Ahmed Altashani, Mohammed Alsairy, Abdulaziz Alsakhri, Mohamed Ali, Munif Alqahtani, Zeyad Alsehli, Abdullah Alilwit, Hassan AlMirza
DOI: http://dx.doi.org/10.52533/JOHS.2023.31209
Keywords: Wilson's disease, ATP7B gene, Hepatic copper transport,Sunset glow hepatocytes, Multidisciplinary management
Wilsons disease is a disorder that occurs when there are mutations, in the ATP7B gene. This leads to problems with copper transport and metabolism in the body. In this review we explore the causes, effects, symptoms and management of Wilsons disease. We delve into the factors that contribute to the condition and how it affects the livers’ ability to handle copper. A key diagnostic feature is the presence of "sunset glow" hepatocytes indicating a buildup of copper. The disease manifests with symptoms affecting organs such as the liver nervous system, mind, blood, kidneys and eyes. Due to this range of symptoms an accurate diagnosis requires an approach. Prognosis and tailored treatment strategies can be aided by staging using the Leipzig scoring system. We discuss complications associated with Wilsons disease. Highlight its impact on organs underscoring why timely diagnosis is crucial. The management section outlines approaches including medication to remove copper from the body or regulate zinc levels as well as dietary modifications to control copper absorption. Regular monitoring through liver function tests, copper measurements and neurological assessments is essential for managing this condition. Genetic counseling plays a role in helping individuals make decisions about their health when it comes to Wilsons disease. In cases where other treatments have failed or are inadequate, for controlling symptoms or preventing organ damage liver transplantation may be considered as a resort option. Finally, we conclude by highlighting how ongoing research continues to improve our understanding of Wilsons disease and refine methods and treatment strategies.
Introduction
Wilsons disease is a disorder that occurs due to mutations in the ATP7B gene leading to disruptions in copper transport and metabolism. The underlying cause of Wilsons disease lies in a malfunctioning liver copper transport system, which results in the buildup of copper in the liver and other important organs (1, 2). This abnormality arises from the impaired ability to incorporate copper into ceruloplasmin and its subsequent elimination through bile (3). The liver, being crucial for maintaining copper balance becomes the point of copper accumulation. The hereditary nature of Wilsons disease is evident through identified mutations in the ATP7B gene contributing to differing manifestations among affected individuals (4). Genetic testing plays a role in confirming diagnoses and identifying carriers, enabling interventions. From a perspective Wilsons disease exhibits liver abnormalities (5, 6). Copper deposition within the liver leads to the formation of apical granules rich in copper often referred to as "sunset glow" hepatocytes. These granules can be detected using staining techniques like rhodanine or orcein stains serving as markers for diagnosing through tissue examination (7). Progressive liver damage such as steatosis (fatty changes) hepatocyte ballooning (swelling) and fibrosis (scarring) highlight the nature of copper accumulation over time (8). The potential progression, from fibrosis to cirrhosis complicates the clinical course of this condition. Additionally, excessive copper levels contribute to stress further worsening damage. Neurological and psychiatric symptoms often arise as a result of copper buildup, in the system in Wilsons disease (9). This highlights the effects of the condition beyond the liver. Accurately determining the stage of Wilsons disease is crucial, for predicting outcomes and guiding treatment decisions. The scoring system developed in Leipzig is a framework that takes into account biochemical and genetic factors. It helps categorize patients into stages; presymptomatic, asymptomatic or symptomatic. By detecting and intervening early in individuals through family screening we can effectively manage the condition and prevent complications from arising (10). When someone reaches the stage of Wilsons disease, they may experience a range of symptoms affecting their liver, system and mental health. This requires tailored strategies to address the clinical presentation of each individual (11). The complications associated with Wilsons disease are diverse. Affect organs, in the body. Liver disease can lead to the development of conditions, such as cirrhosis and hepatocellular carcinoma. Neurological issues may appear as movement disorders, speech difficulties (dysarthria) and muscle contractions (dystonia), suggesting the basal ganglia’s involvement (12). Psychiatric complications such as depression and changes in personality also contribute significantly to the burden of the disease. Timely diagnosis along with therapy involving copper chelating agents are crucial for managing these complications. Wilsons disease is caused by mutations that disrupt copper metabolism resulting in an array of symptoms affecting the liver nervous system and mental health. The presence of "sunset glow" hepatocytes under examination helps with diagnosis while staging systems provide guidance for predicting outcomes. Given that these complications involve organ systems it is essential to adopt an approach to management. The progress made in testing early identification and treatment interventions has enhanced results underscoring the importance of ongoing research, in refining our comprehension of how Wilson's disease develops and improving therapeutic approaches to achieve better outcomes, for patients. The changing field of Wilsons disease research continues to influence the future of diagnosing, managing and overall clinical course of the condition. This review aims to overview the etiology, histopathology, staging and complications of Wilson Disease.
Methodology
We conducted this review study from Cochrane Library, PubMed, and Scopus. This review delves into the causes, cellular changes, stages and potential complications associated with Wilson's Disease. I focused specifically on studies conducted in English after 2008 that aimed to provide an understanding of this condition. The ultimate goal was to equip healthcare professionals with insights into assessment methods and early detection systems, for managing Wilson Disease and safeguarding patient well-being.
Discussion
The symptoms of Wilsons disease can vary widely. Affect parts of the body. The liver plays a role, in the presentation because it is where copper tends to accumulate. Liver symptoms can range from a liver to jaundice and cirrhosis indicating the nature of copper buildup. Neurological symptoms, such as movement disorders and speech difficulties result from copper deposits in the system making diagnosis and management more complex (13, 14). Psychiatric symptoms further complicate matters as they can mimic health conditions. The disorder also has effects on blood, kidneys and eyes highlighting its impact. Given the range of age at onset and the possibility of combined symptoms, a clinical approach involving thorough evaluation and collaboration among various specialists is crucial. Since conditions overlap, advanced testing methods like genetic testing and specialized assessments of copper metabolism are necessary for accurate diagnosis. In terms of treatment, using medications that help eliminate copper (copper chelating agents) or promote zinc absorption is the focus. The choice between these treatments depends on factors such as symptom severity and patient tolerance. Additionally, dietary modifications like a low copper diet are beneficial, alongside medication to reduce copper absorption. Regular monitoring strategies, such as conducting liver function tests and assessing copper levels play a role in adjusting the necessary treatment approaches. Genetic counseling is a source of support and valuable information for individuals affected by this condition and their families. In instances the possibility of liver transplantation becomes an important consideration underscoring the seriousness of potential complications.
Clinical Manifestation
Wilsons disease is a condition that presents a wide range of symptoms making it challenging to diagnose and manage. The main issue in this disorder is the buildup of copper in different organs, particularly the liver and central nervous system (CNS). Among these organs the liver plays a role. Often determines how the disease manifests. One of the common signs is a liver indicating copper accumulation within hepatocytes (Figure 1). As the disease progresses inflammation in the liver can cause jaundice, characterized by yellowing of the skin and eyes due to problems, with bilirubin metabolism.
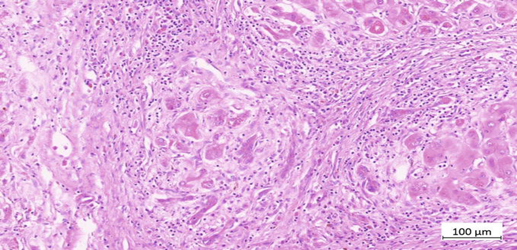
Figure 1: Histopathology of Wilson Disease
Excessive copper buildup can lead to liver cirrhosis, which can result in complications, like hypertension, ascites (fluid retention) and splenomegaly (enlarged spleen). In cases hepatocellular carcinoma (liver cancer) can emerge as a serious complication highlighting the seriousness of liver involvement in Wilson's disease (15). Another significant aspect of this condition is its impact on the system, where copper deposition leads to manifestations. Common symptoms include movement disorders such as tremors, dystonia (involuntary muscle contractions and abnormal postures) and dysarthria (slurred speech). The distinct "wing beating" tremor characterized by flapping hands and arms is particularly noticeable. Additionally, Wilsons disease affects health giving rise to psychiatric symptoms. Personality changes with irritability, mood swings and depression are frequently observed. Some individuals also experience impairment and difficulties concentrating which significantly impact their quality of life (16). Psychiatric symptoms do not make the clinical presentation more complex. Also pose diagnostic challenges as they can overlap with other mental health conditions. Although common Wilsons disease can affect blood and iron metabolism leading to manifestations (17, 18). Anemia may occur due to difficulties in absorbing copper in the tract. Liver dysfunction caused by Wilsons disease can also result in coagulation issues, indicated by time due to impaired synthesis of clotting factors. Kidney complications, although less frequent are possible in Wilsons disease. Copper buildup in the kidneys can cause dysfunction in tubules leading to copper excretion through urine. This process can contribute to the formation of kidney stones. In cases renal impairment. Ocular involvement introduces an aspect where Kayser Fleischer rings appear as a distinctive sign—these rings display golden brown to greenish hues in the cornea due to copper deposition (19). While not always present their identification serves as a clue, for diagnosing Wilsons disease. The clinical presentation of Wilsons disease varies widely. Can affect organ systems or multiple systems simultaneously. Additionally, the onset of symptoms varies across age groups including childhood, adolescence or early adulthood. The diverse range of symptoms in this condition requires attention from healthcare providers particularly when dealing with liver problems, neurological issues and mental disturbances. Diagnosing these symptoms accurately can be challenging due to their nature often resulting in delays. To confirm the diagnosis, it is crucial to conduct tests such as liver function tests and specialized assessments of copper metabolism, which involve measuring copper levels and serum ceruloplasmin levels. In summary Wilsons disease manifests, as a condition that impacts parts of the body, including the liver, central nervous system (CNS) and other organs.
The combined effects on the liver, CNS, psychiatric health blood related issues, kidneys and eyes contribute to the nature of this disorder. The variability in symptoms onset and the possibility of combined manifestations emphasize the need for a multidisciplinary approach to diagnosis and treatment. It is crucial to identify these signs on in order to intervene promptly and improve outcomes, for individuals affected by Wilson's disease.
Management
Managing Wilsons disease, a disorder that affects how the body handles copper requires a detailed and lifelong approach. The goal is to reduce symptoms prevent complications and improve the quality of life for those affected. Treatment involves using medications to help remove copper from the body and prevent it from building up to levels. Alongside medication dietary considerations and careful monitoring play roles, in ensuring the outcomes for individuals living with this condition (20). The main focus of treatment revolves around copper chelating agents like penicillamine and trientine. These agents create complexes, with copper increasing its excretion through urine and effectively reducing copper levels in the body. However, using penicillamine may come with side effects, such as complications in blood and kidney function. Trientine is often preferred as a second line option due to its side effect profile. In addition, zinc can be used as another choice by stimulating cells to produce metallothionein—a protein that binds and inhibits copper absorption. Zinc is frequently used for maintenance therapy after copper reduction with chelating agents especially when individuals have difficulties tolerating these agents or as a long-term strategy to prevent copper from building up. The decision between using copper chelating agents or zinc depends on factors such as symptom severity, individual tolerance and the presence of contraindications or side effects. It's crucial to tailor the approach to each patient needs in order to optimize therapeutic outcomes and ensure the most effective treatment plan (21, 22). While medications play role dietary adjustments are also essential, in managing Wilsons disease. It is recommended that people follow a diet, in copper, which means they should limit their intake of copper foods such as organ meats, shellfish, nuts, chocolate and certain legumes. These dietary changes work together with medication to reduce the absorption of copper. It is important to monitor the status to address any potential deficiencies that may result from dietary restrictions or issues, with absorbing nutrients due to the disease or its treatment. Making sure that we have zinc and selenium which're essential nutrients, is also crucial for overall well-being. In terms of management, it is important to monitor and follow up with patients. This involves conducting liver function tests to assess how well the liver is functioning and to detect any signs of liver damage or impairment. By monitoring liver enzymes and markers, we can determine how effective the therapy is and whether any adjustments need to be made. It is also important to measure copper levels in both blood and urine as a way of evaluating the success of chelation therapy or zinc supplementation. This helps us make treatment decisions that keep copper levels within the desired range. Given the possibility of psychiatric symptoms it is crucial to assess a patient’s neurological and psychiatric status. This includes evaluating movement disorders, cognitive function and psychiatric symptoms so that any neurological involvement can be detected on. This enables us to intervene promptly and adjust strategies as needed. Throughout the management of Wilsons disease genetic counseling plays a role in providing support and information, for individuals and their families. This support helps them understand the nature of the condition, make decisions and navigate potential challenges related to genetic implications. In cases where liver disease or failure reaches a stage and doesn't respond to treatment doctors may consider liver transplantation. This procedure provides a cure by replacing the liver with a healthy organ, from a donor It is important to monitor the status to address any potential deficiencies that may result from dietary restrictions or issues, with absorbing nutrients due to the disease or its treatment. Making sure that we have zinc and selenium which're essential nutrients, is also crucial for overall well-being. In terms of management, it is important to monitor and follow up with patients. This involves conducting liver function tests to assess how well the liver is functioning and to detect any signs of liver damage or impairment. By monitoring liver enzymes and markers, we can determine how effective the therapy is and whether any adjustments need to be made. It is also important to measure copper levels in both blood and urine as a way of evaluating the success of chelation therapy or zinc supplementation. This helps us make treatment decisions that keep copper levels within the desired range. Given the possibility of psychiatric symptoms it is crucial to assess a patient’s neurological and psychiatric status. This includes evaluating movement disorders, cognitive function and psychiatric symptoms so that any neurological involvement can be detected on. This enables us to intervene promptly and adjust strategies as needed. Throughout the management of Wilsons disease genetic counseling plays a role in providing support and information, for individuals and their families. This support helps them understand the nature of the condition, make decisions and navigate potential challenges related to genetic implications. In cases where liver disease or failure reaches a stage and doesn't respond to treatment doctors may consider liver transplantation. This procedure provides a cure by replacing the liver with a healthy organ, from a donor. It's essential to keep a watch, on the condition to address any issues that may arise from dietary restrictions or difficulties in absorbing nutrients caused by the disease or its treatment. Ensuring an intake of zinc and selenium which're vital nutrients, is also crucial for overall well-being. When it comes to managing the condition it's important to monitor and follow up with patients. This involves conducting liver function tests to assess the liver’s performance and identify any signs of damage or impairment. By tracking liver enzymes and markers, we can gauge the effectiveness of the therapy. Make adjustments if needed. It's also important to measure copper levels in both blood and urine to evaluate the success of chelation therapy or zinc supplementation. This helps us make decisions about treatment while keeping copper levels within the desired range. Considering the occurrence of symptoms, it is crucial to evaluate a patient’s neurological and psychiatric status thoroughly. This includes assessing for movement disorders, cognitive function and psychiatric symptoms so that any neurological involvement can be promptly detected, and appropriate strategies can be implemented if required. Genetic counseling also plays a role throughout Wilsons disease management by providing support and information, for individuals well as their families. This assistance aids individuals in comprehending the characteristics of the situation, making choices and effectively dealing with any implications that may arise. In situations where the liver becomes severely diseased or fails to respond to interventions physicians may contemplate the option of liver transplantation. This surgical procedure offers a remedy by substituting the liver with a healthy organ obtained from a donor.
Conclusion
The intricate nature of Wilsons disease, including its causes, varied symptoms and challenges, in treatment highlights the importance of a personalized approach. Progress in testing monitoring techniques and available treatments has greatly improved outcomes. However ongoing research on Wilsons disease emphasizes the need for refinement in diagnosis and care. Managing this condition involves an approach that includes medication, dietary considerations and addressing aspects to optimize results. It is crucial for healthcare professionals to recognize the difficulties associated with Wilsons disease in both diagnosis and long-term management to improve the quality of life for those affected. As research continues to shape our understanding and treatment of Wilsons disease, collaboration between doctors, researchers and patients will play a role, in advancements in this field.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
