Volume 3, Issue 12
December 2023
Prevalence, Diagnosis and Management of Allergic Rhinitis in Asthmatic Children
Abdulghani Alzamzami, Zahra AlAlwan, Hassan Thubab, Roaa Alkanderi, Faten Althomali, Aljazi Alajmi, Osamah Alkhaldi, Manal Aldaihani, Amir Alrajhi, Noor Almakinah, Nouf Alnafisi,Ahmed Almehmadi,Abdulelah bakhsh
DOI: http://dx.doi.org/10.52533/JOHS.2023.31211
Keywords: asthma, allergic, rhinitis, diagnosis, treatment, management
Allergic rhinitis is a prevalent upper airway inflammatory disease that is especially widespread in the paediatric population. In the medium- to long-term, allergic rhinitis can have a significant impact on quality of life, sleep, and everyday functioning. Watery rhinorrhea, nasal congestion and obstruction, sneezing, and nasal itch are the hallmark clinical manifestations of allergic rhinitis. The diagnosis is based on a thorough history, a chest and nasal examination, and tests for certain immunoglobulin E. Usually, allergic rhinitis coexists with other allergic diseases, including asthma and allergic conjunctivitis. Asthma and allergic rhinitis are prevalent conditions that often coexist. In the literature, this idea has been referred to as a unified airway disease. According to epidemiological research, rhinitis is a common co-occurring condition in most asthma patients, and having rhinitis increases the chance of developing asthma. Patients with rhinitis and asthma have similar physiologies. Avoiding allergens that trigger allergic rhinitis and using pharmacological therapies in accordance with guidelines are essential for its proper management. A tripartite treatment plan incorporating pharmacological treatment, immunotherapy, and environmental control is recommended for the optimal management of allergic rhinitis. However, the sole treatment for the cause is still allergen-specific immunotherapy and various nutraceuticals have been employed for symptomatic relief.
Introduction
Rhinitis is one of the most prevalent conditions affecting young children (1). The classic constellation of nasal symptoms that indicate underlying inflammation and/or malfunctioning nasal mucosa, such as sneezing, pruritus, rhinorrhea, and congestion/obstruction, is represented by rhinitis. There are three recognized subcategories, or phenotypes, of rhinitis: non-allergic, non-infectious rhinitis, allergic rhinitis (AR), and infectious rhinitis. A dynamic evolution over time may be observed in several patients exhibiting overlapping or mixed features (2, 3). AR is a symptomatic disease that results from allergy-induced inflammation of the nasal membranes following allergen contact. Watery rhinorrhea, nasal congestion and obstruction, sneezing, and nasal itch constitute typical symptoms of AR (4). An illustrative representation of the pathophysiology of AR is presented in (Figure 1) (5).
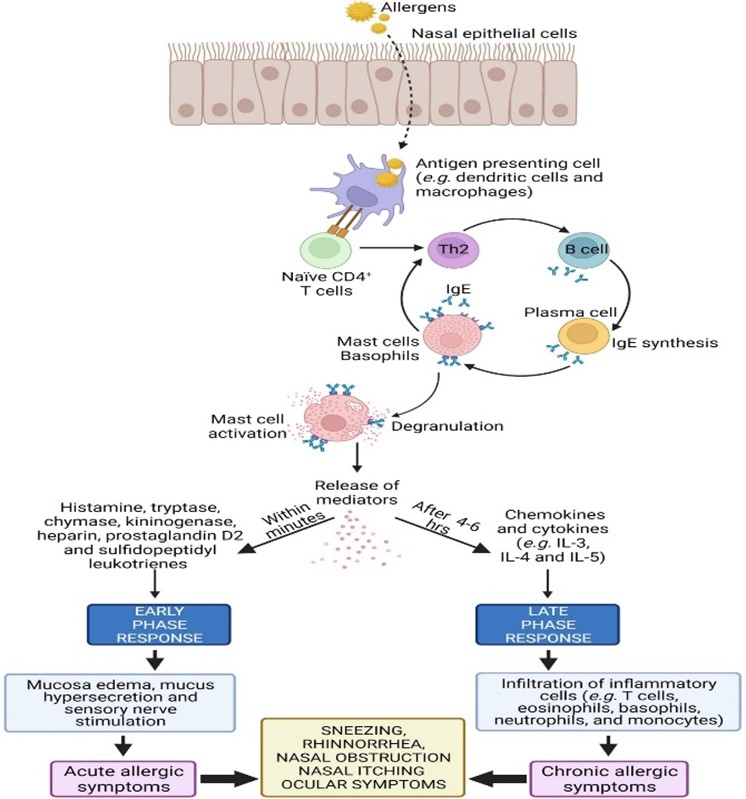
Figure 1: An illustrative representation of the pathophysiology of AR (5)
Among children, AR is one of the most prevalent and persistent diseases. It is still, nevertheless, underdiagnosed and undertreated. Its prevalence, which ranges from 2% to 25%, has been increasing in recent years (6). Evidence from present times research suggests that AR may be a part of a systemic airway disease that affects the entire respiratory tract, contrary to the previous belief that it is a disorder exclusive to the nose and nasal passages (7). In accordance with a World Health Organization report, there is a correlation between rhinitis and asthma. Approximately 30% of individuals with rhinitis develop asthma, and up to 80% of patients with persistent asthma also have rhinitis. Asthma is a diverse disease that is typically characterized by persistent inflammation of the airways. It is identified by a history of respiratory symptoms that change over time and in intensity, including wheeze, shortness of breath, chest congestion, and coughing, as well as fluctuating expiratory airflow limitation (8).
Asthma and AR are prevalent conditions that often coexist. In the literature, this idea has been referred to as unified airway disease. According to epidemiological research, rhinitis is a common co-occurring condition in most asthma patients, and having rhinitis increases the chance of developing asthma. Patients with rhinitis and asthma have similar physiologies, such as increased reactivity to different stimuli and heightened bronchial hyperresponsiveness. The immunopathology of allergic rhinitis is likewise comparable, with tissue eosinophilia and T-helper type 2 inflammation predominating. The unified airway idea has been explained by several processes, but the strongest lines of evidence point to the possibility that systemic inflammation can be triggered by localized airway inflammation. Pharmacotherapeutic research has demonstrated that the treatment of rhinitis in turn improves the condition of asthma and vice versa (9).
A tripartite treatment plan incorporating pharmacological treatment, immunotherapy, and environmental control is recommended for the optimal management of AR. Nowadays, immunotherapy is thought to have preventive potential and be able to change how AR develops. The World Health Organization's guidelines for treating AR suggest a tiered approach that combines diagnosis and treatment. According to this approach, AR is divided into two categories: mild or moderate to severe, depending on severity, and either intermittent or persistent in terms of frequency. Depending on the severity of the condition, oral or topical antihistamines and intranasal corticosteroids are the mainstays of pharmacologic therapy for AR; several of these medications have been approved for use in children as young as five years old (10). Since asthma and AR are one of the most widespread conditions among children and they often co-exist it is essential to understand and discuss these especially in the context of their diagnosis and management. Additionally, studying allergic rhinitis in asthmatic children is significant because it can help improve the management of both conditions, enhance the quality of life for affected children, and potentially lead to better prevention and treatment strategies. Therefore, in this paper, we aim to review the existing evidence from the literature for the prevalence, diagnosis, and management of AR, especially among asthmatic children, and from the findings of our comprehensive review, we will not only highlight the burden of these diseases but also provide evidence-based strategies for the management of these diseases that can further help clinicians in their practice, especially among this group.
Methodology
A comprehensive literature search in the PubMed, Web of Science, Science Direct, and Cochrane databases utilizing the medical topic headings (MeSH) and relevant keywords such as ‘rhinitis’, ‘allergy’, ‘asthma’, ‘prevalence’, ‘frequency’, 'diagnosis', 'management', 'treatment', and a combination of all available related terms was performed on December 1, 2023. All relevant peer-reviewed articles involving human subjects and those available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, or participant age.
Discussion
Since AR is not linked to a high rate of morbidity or mortality, it may appear benign in comparison to other medical conditions. Nonetheless, the disease's impact and the associated socioeconomic costs are significant. For many patients, AR reduces quality of life by impairing sleep, diminishing cognitive function, and causing fatigue and irritation. Additionally, it is linked to worse performance at school, particularly during pollen-peaking seasons. Frequently, patients with AR seek care from family pediatricians, primary care clinics, and hospitals, including emergency rooms and regular outpatient clinics. Appropriate management of AR enhances quality of life, reduces symptoms, and boosts productivity at school (11). Moreover, Asthma and AR are both considered to be symptoms of the same disease. Asthma issues may also improve with AR treatment (12).
Findings of a systematic review and meta-analysis from recent times explained that asthma incidence is correlated with AR. All subgroups showed this relationship, though to varying degrees. The atopic march hypothesis, which views atopic disorders as a sequence of sequential clinical manifestations that begin with atopic dermatitis, proceed with AR, and conclude with asthma as sensitizations in upper and lower airways, respectively, offers a plausible explanation for this association. The one airway, one disease approach, which holds that asthma and AR are just one special disease, reflects a similar point of view (13).
Incidence
The findings of a Japanese cohort study showed a 77.7% incidence of AR. The average age at which rhinitis and asthma started was 2.9 and 2.8 years, respectively. In 8.9% of the children, nasal problems first appeared in the first year of life. In children with co-occurring AR and asthma, the co-occurring condition began in the same year in 26.7% of cases, rhinitis in 33.7% of cases, and asthma in 31.7% of cases (14). While findings of a Korean nation-wide survey in 2020 showed asthma was predicted to affect 0.9% of newborns, 2.3% of preschoolers, 4.1% of school-age children, 2.3% of adults, and 4.1% of senior citizens, AR was assessed to be prevalent in 9.0%, 20.2%, 27.6%, 17.1%, and 6.9% of cases, respectively (15). Results of a recent Nigerian cross-sectional population-based survey demonstrated that among those with clinical asthma, AR was prevalent in 74.7% of cases. Asthma confirmed by a physician, clinical asthma, and wheeze have been identified in 2.5%, 6.4%, and 9.0% of cases, respectively. There was a 22.8% prevalence of AR. Age was associated with a rise in the incidence of rhinitis and asthma with the incidence of clinical asthma: 3.1%, 9.8%, and 10.7% among 6–17 years old, 18–45 years old, and >45 years old, respectively (16).
Results of a clinical trial in the United States in 2015 demonstrated that AR has been observed in 18% of the population overall. Strong correlations were found with other allergic diseases: AR was present in 53% of children with asthma compared to 15% in those without asthma (P < 0.001) (17). Togias et al. in 2019 reported that among the asthmatic children, 93.5% suffered from rhinitis (18). While results of a study from the Middle East in 2021 showed that among the 6- to 7-year-old group's prevalence were hay fever (22.1%), atopic dermatitis (12.9%), wheezing (44.2%), asthma (11.9%), and AR (46.5%). Whereas the incidence rate was 9.8%, 33.1%, 51.3%, 19.9%, and 14.6%, respectively, in the 13–14-year-old age group (19). Findings of a meta-analysis from Saudi Arabia in 2022 reported that, compared to adults, children and adolescents had a lower prevalence of AR (13.7% vs. 31.1%) (20). The results of a cross-sectional study from Saudi Arabia in 2023 demonstrated that a historical prevalence of 31.8% was determined for clinically diagnosed bronchial asthma. Almost 45.8% of people with present wheezing (within the last 12 months) and 51.0% of those with lifetime wheezing reported having asthma symptoms. Clinically diagnosed atopic dermatitis had a frequency of 30.2%, while AR had a prevalence of 56.8%, which is quite high (21).
Diagnosis and management
The diagnosis is based on a thorough history, a chest and nasal examination, and tests for certain immunoglobulin-E (22). Diagnostic markers of AR include clinical symptoms like sneezing, itching, rhinorrhea, and nasal congestion without any signs of lower respiratory tract infections or abnormalities of the nose's anatomy. To bolster the association between possible allergens and clinical history, this is linked to a positive prick test and an elevated level of a particular immunoglobulin E. Due to the substantial hereditary component of the allergic response, the patient's history and the family history are crucial in the diagnosing process (23). Various diagnostic cellular and molecular modalities for AR and asthma are described in (Figure 2) (24).
When co-morbid disorders arise, the well-described pathways of customized treatment for asthma and rhinitis diverge. Studies on widely used pharmaceutical interventions, however, indicate an intriguing field. Children with asthma and rhinitis may find that intranasal glucocorticosteroids, immunotherapy, antihistamines, and anti-leukotrienes act as weapons, reducing the symptoms of both conditions. Helping patients achieve better treatment compliance appears to be a viable tactic. The continuous observation of treatment compliance is essential until the ideal degree of symptom management is reached. Effective communication is essential, as is providing patients and parents of small children with knowledge of all possible treatment options and scrupulously adhering to a stable care strategy (11).
Oral antihistamines are frequently chosen over intranasal corticosteroids, despite the latter being the most efficacious pharmacologic treatment for AR. Since first-generation antihistamines are readily available and affordable, they may be used to treat AR symptoms; however, because of their weak receptor specificity, they have sedative and cardiovascular side effects. Second-generation antihistamines were therefore created with the goal of minimizing side effects without sacrificing effectiveness. The highly selective second-generation antihistamine fexofenadine does not cause cardiovascular side effects, is non-sedating since it reduces blood-brain barrier permeability, and efficiently relieves symptoms of allergic reactions. However, the necessity to gather efficacy and safety data in young children with AR is underscored by the fact that there are fewer clinical studies conducted in children than in adults (25).
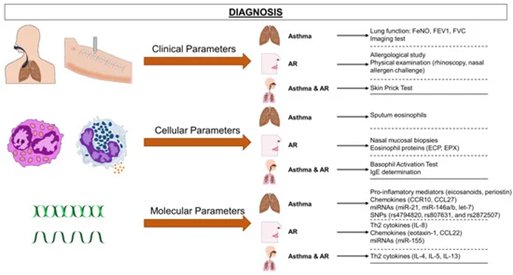
Figure 2: Various diagnostic instruments for asthma and AR. Asthma can be diagnosed using a wide range of diagnostic techniques, including cellular (eosinophil counts, basophil activation test), molecular (measurements of cytokines and chemokines, and other biomarkers such as miRNAs), and classical (lung function, medical history, skin prick test) approaches (24).
Yu et al. demonstrated in their findings that, compared to people without asthma, asthma with AR patients who used intranasal corticosteroids and/or second-generation antihistamines had a decreased chance of an acute exacerbation; however, this was not the case for patients with asthma who did not receive any medication. Leukotriene receptor antagonists decreased the chance of an acute exacerbation for asthma patients between the ages of 2 and 6, but not for those between the ages of 7 and 18. In contrast to patients receiving inhaled corticosteroids, patients receiving a combination of two or three controls were more likely to experience an acute exacerbation (26).
Moreover, Baena-Cagnani et al. described that it has been shown that using a monoclonal antibody against immunoglobulin-E can effectively lessen rhinitis and asthma symptoms. It permits a decrease in the amount of inhaled steroids, the frequency of exacerbations, emergency room visits, and hospital stays for individuals with asthma who are difficult to treat. In clinical trials, specific sublingual immunotherapy produced encouraging results by altering immunoglobulin and cytokine profiles and promoting T-cell tolerance. With comparable efficacy, sublingual immunotherapy has overtaken subcutaneous immunotherapy in terms of safety. The novel inhaled steroid ciclesonide only activates in the respiratory system, is ineffective against pre-existing inflammation, and has very little systemic impact (27).
Children who have asthma frequently experience AR, which significantly impairs asthma control. The authors postulate that diagnosing and treating this disease in children with nasal corticosteroids may enhance asthma control; however, in order to verify this theory, randomized clinical trials are required (28). Most likely, AR is the most significant extra-bronchial predictor of asthma control as well as the most significant risk factor for the onset of asthma. From this angle, allergen immunotherapy must always be viewed through the lens of precision medicine. Allergen immunotherapy does offer a singular chance to target the immunological basis of allergic reactions, enhance the management of both bronchial and allergic reactions, and stop the progression of allergic diseases. Every clinician treating children with AR should prioritize confirming the patient's eligibility for that choice, particularly if the condition is linked to bronchial asthma (29).
Allergen immunotherapy is available to children with positive skin prick test results or immunoglobulin-E against one or more allergens whose exposure is associated with moderately severe allergic reactions and AR symptoms, including conjunctivitis that interferes with daily activities or sleep, and/or allergic asthma. Another justification for allergen immunotherapy is inadequate symptom control, even with medicine or in circumstances where avoidance is not an option. When a patient wants to avoid long-term treatment or if they frequently experience serious adverse drug reactions, allergen immunotherapy should also be considered. However, it is critically important to consider the patient's readiness as well (30, 31). Nevertheless, young patients with AR or their parents frequently self-manage the condition or undervalue its symptoms. Self-management frequently results in the adoption of inappropriate or unrecommended therapeutic choices, such as alternative medicine cures, or in the wrong scheduling of therapy sessions. Such a strategy runs the risk of increasing the burden of the disease and decreasing the likelihood of total remission (29). Therefore, counselling by physicians for children and their parents is highly recommended. Our review provides deep insights into the diagnosis and management of AR among asthmatic children with evidence from recent times. Additionally, we discuss the incidence among different global geographical locations, which is one of the strengths of our study. However, due to the dearth of studies and clinical trials among children, we could not describe the efficacy of various management strategies employed, which is the limitation of this paper, for which we would highlight the need for future clinical research in this aspect.
Conclusion
Allergic rhinitis among asthmatic children shows a diverse prevalence pattern among various geographical areas; however, it is routinely observed in clinical practice, and timely diagnosis and effective management strategies are needed to prevent exacerbation events among children. Apart from the pharmacological therapy as per guidelines, allergen immunotherapy does offer a special chance to target the immunological basis of AR, enhance control over both AR and bronchial asthma, and stop the progression of allergic diseases.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
