Volume 3, Issue 12
December 2023
Etiology, Epidemiology and Clinical Assessment of Hand, Mouth and Foot Disease
Abdulghani Alzamzami, Omar Alkhaldi, Mousa Alamoudi, Nawaf Aljadani, Abdulmohsin Alahmadi, Mayada Alyamani, Meshari Almalki, Abdulrahman Almazni, Abdullah Alqahtani, Naif Alalyani, Noor Sheikh
DOI: http://dx.doi.org/10.52533/JOHS.2023.31212
Keywords: hand-foot-and-mouth disease, enteroviruses, Coxsackievirus, etiology, epidemiology
Hand-foot-and-mouth disease (HFMD), first identified in 1957, has evolved into a significant global health concern. It is caused primarily by enteroviruses, particularly Coxsackievirus (CV) and Enterovirus A71 (EV-A71), HFMD predominantly affects children under five. The disease's etiology has shifted over the years, with newer strains like CV-A6 and CV-A10 emerging as notable culprits in recent outbreaks across Asia, America, and Europe. Epidemiologically, HFMD poses a major challenge in regions like the Western Pacific, with countries like China reporting over 10 million cases between 2008 and 2014. Clinical manifestations range from asymptomatic to severe, including potentially fatal neurological or cardiopulmonary complications. Treatment is primarily supportive, lacking specific antiviral therapies, and involves antiviral and immunoglobulin therapies, respiratory and cardiovascular support, and traditional Chinese medicine. Prevention focuses on hygiene practices, with no vaccines currently available. This review synthesizes current knowledge on HFMD's etiology, epidemiology, and clinical assessment, aiming to enhance understanding and inform effective public health strategies.
Introduction
In 1957, Toronto reported the first recorded instance of a disease characterized by fever and a vesicular rash on the hands and feet, attributed to Coxsackievirus (CV), particularly strain CVA16 (1, 2). This marked the beginning of our understanding of a condition that would later be known as hand-foot-and-mouth disease (HFMD). In the ensuing years, the disease's profile has evolved considerably, both in terms of its epidemiology and the challenges it presents to public health. By 1959, this disease was officially named HFMD by Robinson et al., who recognized it as a distinct clinical entity with symptoms similar to those initially reported. This naming was a pivotal moment in the medical history of HFMD, providing a framework for further research and understanding (3). HFMD is a mild, contagious viral infection common in young children. In the decades following these initial reports, there was a significant increase in the frequency of HFMD outbreaks around the globe. These outbreaks were predominantly caused by several strains of enteroviruses, including Enterovirus A71 (EV-A71), CVA16, CVA6, and various echoviruses (Echo) (4). Each of these viruses contributed to the spreading and diversification of HFMD, making it a disease of global concern. EV-A71, in particular, garnered significant attention when it was first isolated in 1969 from a child suffering from meningitis. This strain proved to be highly virulent and was responsible for numerous severe outbreaks of HFMD, especially in the Asia–Pacific region (5). The disease, typically mild and short-lived, presents with fever, a characteristic blister-like rash on the hands and feet, and oral ulcers resulting from ruptured blisters in the mouth. However, it was the potential for severe complications that set EV-A71 apart and raised alarms in the medical community.
A notable aspect of HFMD is the variability in its severity. While most cases are mild and resolve within a week, a significant number of patients experience fatal neurological or cardiopulmonary complications. This aspect of HFMD has been a major concern for healthcare professionals, highlighting the unpredictable nature of the disease and the importance of early diagnosis and intervention. Recent follow-up studies have shed light on another concerning aspect of HFMD: the occurrence of severe neurological sequelae in patients who have recovered from more serious forms of the disease. These findings have emphasized the need for continued monitoring and research into the long-term effects of HFMD (5). As the 21st century progressed, HFMD increasingly became a significant public health concern, particularly in the Asia–Pacific region (6). The discovery of "tomato flu," a HFMD-like illness caused by an enterovirus in India, further underscored the evolving nature of HFMD and related diseases.
Methodology
This study is based on a comprehensive literature search conducted on December 7, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the etiology, epidemiology, and clinical assessment of hand, mouth, and foot disease. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Etiology
HFMD is primarily caused by EVs, which are part of the Picornaviridae family. These EVs are positive-sense single-stranded RNA viruses classified into four species: EV-A, EV-B, EV-C, and EV-D, each encompassing various types (7). In over 90% of HFMD cases, the causative types are from species A (8). Previously, most of the remaining cases were attributed to Coxsackievirus CV-B2 and CV-B5, but recent years have seen a rise in HFMD cases caused by CV-B3, especially in China and its neighboring countries (9).
Historically, EV-A71 and CV-A16 were the predominant viruses causing HFMD outbreaks globally (10-12). However, in recent times, CV-A6 and CV-A10 have emerged as significant pathogens, replacing EV-A71 and CV-A16 in many instances. Since 2010, outbreaks caused by these emerging viruses have been documented across Asia, America, and Europe (9).
Phylogenetic analysis of EVs involved in HFMD outbreaks reveals that EV-A71 strains are divided into three genotypes (A, B, and C) and further into 11 sub-genotypes. The most common genotypes responsible for outbreaks are B and C, or a combination thereof. However, the specific sub-genotypes involved vary, indicating shifts between genotypes. In some cases, multiple sub-genotypes have circulated simultaneously, leading to recombination and the emergence of new genotypes. An example is the recombination between EV-A71 C2 and CV-A8, resulting in genotype B4, which caused epidemics in Japan, Taiwan, and other countries. In Malaysia, different combinations of B4, B5, and C1 sub-genotypes caused epidemics in various years from 1998 to 2006. In China, sub-genotype C4, particularly variant C4a, was the most prevalent (13), while in Europe, sub-genotype C1 was common until 2005, later replaced by C2 after 2007 (14). There have also been recent cases of EV-A71 C4 HFMD in Europe, suggesting the introduction of this sub-genotype from Asia (15).
CV-A16 is categorized into genotypes A and B, with B further divided into B1 and B2, and further into sub-genotypes B1a, B1b, B1c, B2a, B2b, and B2c (16). In China and nearby regions, B1a and B1b have been the predominant genotypes (17). CV-A6 strains fall into genotypes A to F, with varying genotypes identified in different countries. Genotype F, mainly detected in China, is a recent development (18). These strains appear to have evolved from recombination of previously circulating groups (19).
CV-A10 has four identified genotypes (A–D), each with several sub-genotypes. In China, genotype B was common until 2008, then genotype C emerged and was also found in Spain and France (20). Initially, sub-genotypes 1 and 2 were frequent, but by 2012, lineages 3 and 4 became more common (21). The co-circulation of different viral genotypes and sub-genotypes is common during outbreaks. These variations in the molecular epidemiology of HFMD-causing viruses are due to recombination or spontaneous mutations, which can also lead to changes in antigenic properties, potentially causing new infections in previously affected individuals.
Epidemiology
HFMD epidemiology is primarily focused on regions where the disease is endemic and has seen a significant number of severe cases. The Western Pacific Region, as defined by the World Health Organization (WHO), is a prime example of this. In many countries within this region, specific surveillance systems for HFMD have been established, and in some instances, reporting the disease to health authorities is mandatory.
China, which has the largest population and one of the most advanced surveillance systems, made HFMD a notifiable disease in 2008. Since then, the characteristics of the infectious agents have been continuously monitored (9). From May 2008 to June 2014, China reported a staggering 10,717,283 HFMD cases, resulting in 3,046 deaths and a fatality rate of 0.03%. The morbidity rate among survivors increased significantly from 37.6 per 100,000 in 2008 to 139.6 per 100,000 in 2013, with a peak in 2012 of 166.8 per 100,000. Notably, over 90% of these cases were diagnosed in children under five years old. Mortality rates were highest in children aged two years or younger, with 84.02% of deaths occurring in this age group, suggesting that both susceptibility and severity of HFMD are age-related (22).
Other factors associated with HFMD include gender, hygiene, social contact, and meteorological conditions. While infection rates are similar in males and females (23, 24), males are more prone to develop symptoms, experience diffuse infections, and require medical assistance (25-28). Poor hygiene and social contacts have also been linked to the development of HFMD (29). Meteorological factors like high temperatures and humidity have been associated with increased susceptibility to HFMD.
Clinical manifestations
HFMD can manifest in various ways, ranging from asymptomatic infections to severe complications (Figures 1-3) (30). The exact prevalence of asymptomatic EV infections that can lead to HFMD is unknown, as few studies have focused on this aspect, often employing questionable methodologies. Data from two prospective studies during a large EV-A71 epidemic indicate that about 30% of initially negative subjects seroconvert without showing clinical signs, suggesting a third of infections may be asymptomatic (31). The incubation period for HFMD is generally thought to be 3-5 days, but concrete evidence supporting this is limited. Recent data suggest this period may vary across different pediatric ages, with longer incubation times observed in older children, likely due to better hygiene practices (32).

Figure 1: Maculopapular lesions on the palms of a patient with HFMD (30).
Most symptomatic HFMD cases are seen in children under 5, but adults, particularly those in close contact with infected children, can also be affected. During EV-A6 epidemics in Finland and the USA, about 30% of cases were in adults. Classic HFMD symptoms include low-grade fever, malaise, and a maculopapular rash or blisters on the hands, soles, buttocks, and painful ulcerative lesions in the mouth and tongue. These symptoms usually resolve within 7-10 days. However, atypical cutaneous manifestations linked to CV-A6 and, less commonly, CV-A16, have been reported. These include unusual skin lesions, exacerbated eruptions in atopic dermatitis areas, hemorrhagic or purpuric lesions, and lesions resembling Gianotti-Crosti disease (9).

Figure 2: Maculopapular lesions on the soles of a patient with HFMD (30).
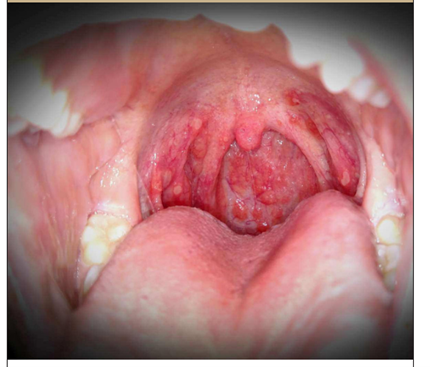
Figure 3: Oral ulcerations in a patient with HFMD (30).
A notable late complication of HFMD is nail issues, with nail shedding, Beau’s lines, and onychomadesis occurring days after traditional symptoms. These are thought to be due to transient nail matrix arrest and direct viral replication. The most severe HFMD complications involve the central nervous system (CNS), including aseptic meningitis, acute flaccid paralysis, and encephalomyelitis, sometimes leading to autonomic dysregulation, pulmonary edema, myocardial impairment, and death (33). Survivors often develop neurological sequelae like cognitive and motor disorders (9). CNS damage is primarily associated with EV-A71 (34, 35), but recent epidemics have shown CNS involvement in 3.6 to 18.2% of EV-A6 HFMD cases. All genotypes and sub-genotypes have been linked to CNS involvement, with certain genotypes, like C4 in China and B3 and B4 in other Asian countries, being more frequently associated with severe cases (9).
Severe CNS involvement in HFMD is not well documented globally. However, data from China (2008-2012) indicated a rate of severe neurological or cardiovascular complications at 1.1% (36). Risk factors for severe disease include persistent high fever, increased neutrophil count, male gender, young age, and absence of mouth and skin lesions. Genetic factors, including single-nucleotide polymorphisms in certain chemokines and interleukins, have been linked to the susceptibility and severity of EV-A71 infections. Severe cases, particularly brainstem encephalitis, are thought to be exacerbated by a strongly systemic and CNS inflammatory response, leading to cardiotoxicity and pulmonary edema (37). Significant concentrations of proinflammatory cytokines and chemokines have been detected in the plasma and cerebrospinal fluid of these patients, suggesting that monitoring these markers could be crucial in identifying patients at risk of life-threatening disease (9).
HFMD treatment
Currently, there is no established antiviral treatment specifically for HFMD, and clinical management methods are not well-defined. Treatment generally involves supportive care, isolation to prevent cross-infection, and meticulous oral and skin care to avoid secondary infections. For severe cases, treatments may include antiviral therapy, immunoglobulin therapy, and support for the respiratory and circulatory systems (Table 1) (5).
|
Table 1. Treatment methods for HFMD (5) |
||
|
Treatment category |
Description |
Specific treatments |
|
General care |
Supportive care, isolation, and meticulous oral and skin care |
|
|
Antiviral therapy |
Used for managing HFMD, though not specifically established for it |
IFN-α, Ribavirin, antiviral peptides. |
|
Intravenous immunoglobulin (IVIG) |
Used in severe cases, can improve disease progression and reduce mortality |
IVIG combined with conventional therapy |
|
Respiratory support |
Critical for severe cases, especially with oxygen supply issues |
Mechanical ventilation, anti-convulsants (e.g., midazolam, phenytoin) |
|
Catecholamine storm treatment |
Stabilizes vital signs in severe cases |
Esmolol, Phentolamine |
|
Cardiovascular support |
Supports cardiac function in severe cases |
Milrinone, Dobutamine, Dopamine, Epinephrine, Vasopressin, Levosimendan |
|
Intracranial pressure control |
Reduces increased intracranial pressure |
Mannitol, Hypertonic Saline, Diuretics |
|
Traditional chinese medicine |
Used alongside conventional therapy for better efficacy |
Andrographolide Sulfonate, S. baicalensis |
|
Other treatments |
For cases unresponsive to routine treatment |
Continuous veno-venous hemodiafiltration, Extracorporeal life support (ECMO) |
Prevention
Preventing HFMD largely relies on effective hygiene practices. Handwashing regularly has been demonstrated to lessen the chance of developing HFMD. This is especially true after changing clothing, using the restroom, and before meals. Disinfecting frequently touched surfaces and objects, like toys, and avoiding close contact or sharing personal items with infected individuals are also important preventive measures. Despite misconceptions, breastfeeding does not affect the incidence of HFMD, and mothers are not advised to cease breastfeeding for prevention. Currently, no vaccines or chemoprophylactic agents are available to prevent HFMD or herpangina. In the United States, excluding children from childcare settings has not been found to effectively reduce the spread of the disease and is recommended only if the child's participation is severely limited or if their presence compromises the care of others (30).
Conclusion
HFMD remains a complex global health issue, requiring continued research and public health efforts. Understanding its evolving etiology, epidemiological patterns, and clinical presentations are crucial for developing effective treatment and prevention strategies. Future work should focus on comprehensive management approaches, vaccine development, and global surveillance enhancements to mitigate the impact of this prevalent disease.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
