Volume 4, Issue 9
September 2024
Advances in Laboratory and Imaging Techniques for Detecting Minimal Residual Disease in Leukemia
Ashgan Mohammed Almnzlawi, Rana Abdulrahim ALaeq, Yosef Mohammed Alotaibi, Khalid Mohammed Ahmed, Sultan Ahmad Alqahtani, Abdulaziz Obaid Alharbi
DOI: http://dx.doi.org/10.52533/JOHS.2024.40913
Keywords: Minimal residual disease, leukemia, laboratory, radiology, imaging, cytometry
Minimal residual disease (MRD) detection plays a crucial role in the management of leukemia, offering insights into treatment efficacy and the risk of relapse. Advances in laboratory techniques have improved the sensitivity and accuracy of MRD detection, enhancing clinical decision-making and patient outcomes. Flow cytometry, one of the most established methods, allows for the identification of leukemic cells through immunophenotypic markers, providing high sensitivity in detecting one leukemic cell among thousands of normal cells. Despite its effectiveness, challenges such as phenotypic shifts in leukemic cells and sample processing limitations remain. Molecular techniques, including quantitative polymerase chain reaction (qPCR) and next-generation sequencing (NGS), have further transformed MRD detection. qPCR provides high sensitivity by amplifying leukemia-specific genetic markers, enabling early relapse detection. NGS offers broader genomic coverage, identifying multiple mutations and clonal populations, which allows for the detection of clonal evolution and resistance. While these molecular methods are powerful, they require specialized laboratories and can be cost-prohibitive in routine settings. Emerging imaging technologies, such as positron emission tomography (PET), magnetic resonance imaging (MRI), and optical imaging, are providing new opportunities to visualize leukemic cells in anatomical locations that traditional methods may not access. These non-invasive techniques offer a complementary approach to molecular and flow cytometry methods, though challenges such as sensitivity and cost remain. The integration of these advanced technologies into clinical practice offers the potential for earlier intervention, personalized treatment adjustments, and improved long-term outcomes for leukemia patients. Continued innovation and research will be critical to overcoming current limitations and expanding the use of these methods in routine MRD monitoring. These advancements promise to reshape the landscape of leukemia management, ensuring more effective and tailored approaches to treatment and follow-up care.
Introduction
Minimal Residual Disease (MRD) refers to the small number of cancer cells that remain in a patient's body after treatment and can eventually lead to relapse. This is a crucial concern in the management of leukemia, as the inability to detect and eliminate MRD can compromise the long-term success of treatment. Advances in treatment protocols have significantly improved remission rates for various types of leukemia, such as acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML). However, even with these advances, detecting MRD remains a critical challenge. Early and accurate identification of MRD can allow clinicians to adjust treatment strategies, thereby improving patient outcomes and reducing relapse rates.
Over the past few decades, the development of more sensitive and specific laboratory techniques has greatly enhanced the ability to detect MRD. Traditional methods, such as microscopic examination, lack the sensitivity required to identify low levels of residual leukemic cells. Consequently, newer molecular and immunological approaches have emerged as superior alternatives. Techniques such as flow cytometry and polymerase chain reaction (PCR) have become the cornerstone of MRD detection. These methods offer greater sensitivity and specificity, allowing for the detection of as few as one leukemic cell in a million normal cells (1, 2). Moreover, these techniques provide valuable information that can guide the clinical decision-making process, especially in the post-treatment phase.
The prognostic significance of MRD detection has been well established, with numerous studies showing that patients with undetectable MRD have a significantly lower risk of relapse compared to those with detectable MRD (3). However, despite these advances, there is still a need for more sophisticated approaches to improve the accuracy and feasibility of MRD detection. Emerging technologies, such as next-generation sequencing (NGS) and digital droplet PCR, are poised to revolutionize MRD monitoring by offering even higher sensitivity and the ability to detect clonal evolution over time (4). These advancements are likely to redefine the landscape of leukemia treatment and monitoring in the coming years. This review will discuss the evolution of laboratory techniques for MRD detection in leukemia, focusing on recent advances that have enhanced the sensitivity and clinical utility of MRD assays.
Review
MRD in leukemia has become a cornerstone in the management of the disease, as it offers insights into the effectiveness of treatment and the risk of relapse. Over the years, the evolution of laboratory techniques has significantly improved MRD detection. Flow cytometry, for instance, has gained widespread use due to its ability to differentiate between normal and leukemic cells based on immunophenotypic markers. Its sensitivity has been shown to detect one leukemic cell among 10,000 normal cells, making it an invaluable tool in clinical practice (5). Despite its advantages, the interpretation of flow cytometry results can be challenging, especially in cases with ambiguous cell populations.
The introduction of molecular techniques, such as real-time PCR, has further enhanced the sensitivity of MRD detection. This method is capable of identifying leukemia-specific genetic abnormalities, such as fusion genes or mutations, with a sensitivity of detecting one leukemic cell among one million normal cells (6). This level of sensitivity allows for earlier detection of relapse, thus enabling timely intervention. However, despite these advancements, limitations such as the need for highly specialized laboratories and high costs remain a challenge for widespread implementation. As laboratory techniques continue to evolve, the integration of multiple methods may provide the most comprehensive approach to MRD detection.
Flow Cytometry in MRD Detection
Flow cytometry has revolutionized the detection of MRD in leukemia due to its ability to analyze multiple cell surface markers simultaneously, providing a rapid and detailed assessment of cellular phenotypes. This method has become a gold standard in MRD detection, especially in ALL and chronic lymphocytic leukemia (CLL). Flow cytometry can detect one leukemic cell in 10,000 to 100,000 normal cells, offering high sensitivity and specificity. Its utility lies in identifying leukemic cells that may have phenotypic characteristics similar to normal cells but with subtle differences that can be used for detection and monitoring (7). The approach typically involves staining cells with fluorochrome-labeled antibodies that bind to cell surface antigens. By analyzing multiple markers simultaneously, flow cytometry can differentiate between normal and abnormal populations, allowing for a precise assessment of MRD. For instance, in ALL, the use of multiple panels of antibodies can highlight aberrant expression patterns that are characteristic of residual leukemic cells. This level of precision enables clinicians to identify patients who are at high risk of relapse and to adjust treatment strategies accordingly (8). Flow cytometry is also valuable because it can be adapted in real-time to emerging markers and advancements in understanding leukemia biology.
Flow cytometry has several limitations. One significant challenge is the requirement for high-quality sample collection and processing, as delayed or improper handling can lead to inaccurate results. Furthermore, leukemic cells may undergo phenotypic shifts during or after treatment, leading to a phenomenon known as immunophenotypic drift. This can complicate MRD detection, as the leukemic cells may lose or alter their expression of the markers used in the original diagnosis (9). As a result, flow cytometry protocols must often be updated to account for these changes, requiring continuous adjustments in antibody panels to maintain detection accuracy. Moreover, the subjective nature of data interpretation in flow cytometry introduces a level of complexity, particularly when distinguishing between low-level MRD and background noise in a given sample. Despite these limitations, the flexibility and adaptability of flow cytometry make it a valuable tool for MRD detection. Continuous advancements in technology, including the use of more sensitive fluorochromes and automated analysis systems, promise to further enhance its diagnostic utility in the future.
Molecular Techniques: qPCR and Next-Generation Sequencing
Molecular techniques have become increasingly important in the detection of MRD, offering greater sensitivity and precision than traditional methods. Among the most widely used molecular techniques are quantitative polymerase chain reaction (qPCR) and NGS. These techniques are particularly valuable in identifying specific genetic abnormalities associated with leukemia, such as fusion genes, mutations, and clonal rearrangements of immunoglobulin or T-cell receptor genes. These genetic markers enable highly sensitive detection of residual leukemic cells, with qPCR capable of detecting one leukemic cell among 100,000 to one million normal cells (10).
qPCR has become a gold standard for MRD detection due to its high sensitivity, specificity, and quantitative nature. This technique amplifies specific DNA sequences associated with leukemia, enabling the detection of minute quantities of residual leukemic cells. One of the key benefits of qPCR is its ability to provide quantitative data on the level of MRD, which can help guide treatment decisions. For example, in CML, monitoring BCR-ABL1 transcript levels through qPCR is a routine part of treatment, and a decrease in MRD levels is often associated with improved long-term outcomes (11). However, qPCR is limited by its need for prior knowledge of specific genetic targets. This means that it can only be applied to leukemias with known molecular markers, and it may miss cases with novel or rare genetic abnormalities. In addition, qPCR is less effective in detecting clonal evolution, which can occur during the course of treatment and may lead to relapse.
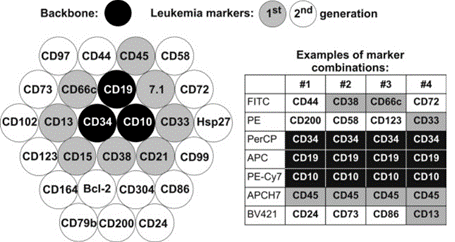
NGS overcomes many of the limitations of qPCR by offering a broader and more comprehensive analysis of the leukemia genome. NGS allows for the detection of multiple mutations and clonal populations simultaneously, making it a powerful tool for monitoring clonal evolution and emerging resistance. This is particularly important in diseases such as acute myeloid leukemia (AML), where the heterogeneity of the disease can complicate MRD detection. NGS can detect as few as one leukemic cell in a million, offering unparalleled sensitivity (12). While NGS is a more powerful tool, it is also more complex and expensive, requiring advanced bioinformatics and significant computational resources to analyze the vast amount of data generated. Despite these challenges, the ability of NGS to detect clonal evolution and novel mutations makes it an essential tool for the future of MRD detection in leukemia. Figure 1 summarizes first and second generation markers for MRD studies in ALL.
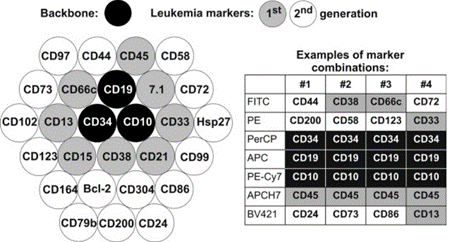
Figure 1: First and second generation markers for MRD studies in ALL
Emerging Imaging Technologies for MRD: Visualizing Leukemia
Recent advances in imaging technologies have introduced novel approaches to detecting MRD in leukemia, complementing traditional molecular and flow cytometry techniques. Imaging offers the potential to visualize leukemic cell distribution and residual disease in anatomical sites that are difficult to assess through conventional sampling techniques, such as the bone marrow and central nervous system. These emerging imaging technologies include Computed Tomography (CT) Positron Emission Tomography (PET), Magnetic Resonance Imaging (MRI), and optical imaging modalities, which have demonstrated potential in MRD detection and monitoring by visualizing leukemia at the cellular and molecular levels. The study by Kumasaka et al. (13) explores the novel application of computed tomography (CT) attenuation values to predict AML by measuring bone marrow density. In their findings, patients with AML exhibited significantly higher CT attenuation values in the iliac bone compared to controls, suggesting that this imaging marker could be a useful diagnostic tool for AML. Figure 2 from Kumasaka et al. study illustrates the regions of interest and the method used for measuring CT attenuation values, highlighting the technical precision in excluding cortical bone and other artifacts to ensure accurate measurements.
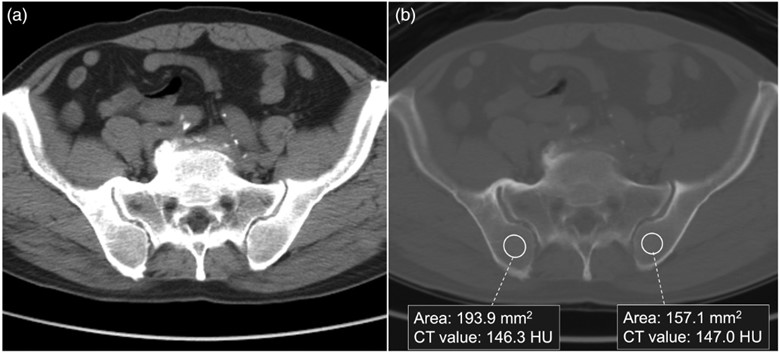
Figure 2: Placement of regions of interest in the iliac bones to measure CT attenuation values, using (a) an abdominal window and (b) a bone window to exclude artifacts like cortical bone and fractures (13).
PET imaging, particularly when combined with computed tomography (PET-CT), has shown promise in tracking leukemic cell activity. This technique works by utilizing radiotracers, such as fluorodeoxyglucose (FDG), to highlight metabolically active cells. Leukemic cells often exhibit high glucose uptake, making FDG-PET a valuable tool for detecting areas of residual disease. While PET imaging is traditionally used in solid tumors, recent studies have explored its potential application in hematologic malignancies, including leukemia. PET imaging can detect metabolically active MRD in extramedullary sites, which may not be accessible by bone marrow biopsy or blood tests (10). However, the sensitivity of PET in leukemia remains a subject of ongoing research, as it may not detect small clusters of cells or cells with low metabolic activity.
Magnetic resonance imaging (MRI) offers another non-invasive approach to visualizing MRD. Advanced MRI techniques, such as diffusion-weighted imaging and dynamic contrast-enhanced MRI, provide high-resolution images of soft tissues, including the bone marrow, where residual leukemic cells may reside. MRI has been used to detect bone marrow infiltration in leukemia patients and has the potential to assess changes in marrow composition after treatment. By detecting alterations in cellular density and vascularization, MRI can provide indirect evidence of residual disease (14). One advantage of MRI is its ability to distinguish between leukemic infiltration and other causes of increased cellularity in the bone marrow, such as reactive changes following chemotherapy. However, further validation is needed to establish MRI as a standard tool for MRD detection in leukemia.
Optical imaging technologies are also emerging as promising tools for MRD detection. Techniques such as bioluminescence imaging and fluorescence molecular tomography are being investigated for their ability to visualize leukemic cells labeled with specific markers. These techniques rely on the use of fluorophores or bioluminescent probes that can bind to leukemia-specific antigens, allowing for the real-time visualization of residual disease. Optical imaging has the potential to detect MRD at very low cell numbers, offering a highly sensitive approach to monitoring disease progression (15). For instance, preclinical studies have demonstrated the utility of bioluminescence imaging in tracking leukemic cells in animal models, providing insights into the dynamics of MRD over time. While this technology is not yet widely used in clinical practice, it represents a promising area for future research and development.
Another emerging modality is the use of single-photon emission computed tomography (SPECT), which has shown potential in detecting MRD in patients with leukemia. SPECT imaging works by detecting gamma radiation emitted by radiolabeled tracers that specifically target leukemic cells. When combined with anatomical imaging techniques such as CT, SPECT can provide both functional and structural information, allowing for the localization of MRD within the body. Studies have demonstrated the ability of SPECT to detect low levels of disease in patients with ALL and CLL, highlighting its potential as a valuable tool for MRD monitoring (15, 16). However, SPECT imaging is still limited by its relatively low spatial resolution compared to other imaging modalities, and further advancements are needed to enhance its sensitivity and accuracy.
Despite the potential of these imaging technologies, several challenges remain. One of the main limitations is the sensitivity of current imaging modalities, which may not yet be sufficient to detect the very low levels of MRD often present in leukemia patients. Additionally, the high cost and complexity of imaging equipment, coupled with the need for specialized expertise, limit the widespread adoption of these technologies in routine clinical practice. Moreover, imaging techniques may not provide the same level of molecular detail as qPCR or NGS, and they are often used in conjunction with these methods to achieve a more comprehensive understanding of MRD (16). Imaging technologies hold significant promise in the detection and monitoring of MRD in leukemia. Techniques such as PET, MRI, and optical imaging offer non-invasive alternatives to traditional MRD detection methods, providing valuable insights into the localization and dynamics of residual disease. As these technologies continue to evolve, they are likely to play an increasingly important role in the management of leukemia, particularly in cases where conventional methods may fall short. However, further research and technological advancements are needed to enhance their sensitivity and establish their role in routine MRD assessment.
Conclusion
Advancements in MRD detection techniques, such as flow cytometry, molecular methods like qPCR and NGS, and emerging imaging technologies, have significantly improved the accuracy and sensitivity of leukemia monitoring. These tools provide crucial insights into disease progression and relapse risk, allowing for timely interventions. However, challenges related to cost, accessibility, and sensitivity still exist, and further research is needed to integrate these technologies into routine clinical practice. As these methods evolve, they hold the potential to revolutionize leukemia treatment and improve patient outcomes.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable.
Consent for publications
Not applicable.
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
The authors have declared that no financial support was received from any organization for the submitted work.