Volume 4, Issue 12
December 2024
Biomechanics in Implant Prosthodontics: Principles for Optimal Design and Function
Khairiah Adel Madani, Abdulaziz Abduallah Alljarallah, Faten Abdullah Alnasser, Mnhal Khalid Alfuraih, Abdullah Hamad Al-Mutairi, Raed Mohammed Barayan
DOI: http://dx.doi.org/10.52533/JOHS.2024.41209
Keywords: Dental implantology, biomechanics, stress distribution, implant design, bone-implant interface, load management
Recent advancements in dental implantology have significantly transformed the field, accommodating both clinicians' aesthetic demands and rising patient expectations. Various implant designs now exist, differing in shape, surface, and size, requiring clinicians to meticulously evaluate each option based on biomechanical principles tailored to individual patient anatomy. Biomechanics, which examines mechanical principles in relation to biological issues, is essential for the success of dental implants. It involves the transfer of loads from the implant to surrounding bone tissues, requiring a deep understanding of how these forces impact the bone-implant interface. Differences in the biomechanical behaviour between natural teeth and implants underscore the need for specialized approaches to implant placement and design to manage stress distribution effectively and prevent overload. Innovations in implant surface treatments and loading protocols further contribute to enhancing implant integration and longevity. This detailed study, based on a thorough review of literature and clinical data, discusses the biomechanical interactions and their impact on the optimal functionality and longevity of implants.
Introduction
Over recent decades, there have been significant technological and scientific developments in dental implantology. With growing aesthetic demands from clinicians and increasing patient expectations, there has been a corresponding evolution in implant designs and clinical approaches (1). The market offers various implants differing in design, surfaces, platforms, connections, and sizes (2). Clinicians must evaluate these options biomechanically, tailored to each patient's unique biological and anatomical needs. The effective distribution of mechanical stresses from the implant to the bone is crucial for the durability of both implants and prostheses. The term biomechanics is related to the application of mechanical engineering to solve biological problems (3).
The durability and effectiveness of dental implants depend on the biomechanical environment, the physical and geometric characteristics of the implant components, and the clinician’s knowledge of these elements (4-6). It is essential for clinicians to grasp how stress is transferred to the bone, which is affected by the type of load applied, the implant's design, and the characteristics at the bone-implant interface (7). This knowledge is crucial for ensuring the durability and functionality of the implants within the biological and mechanical context of the patient's oral anatomy.
In biomechanics, the equilibrium of forces and bending moments is crucial for stabilizing teeth and implants within the jaw. When external forces are applied, they generate equal and opposite internal stresses at the bone anchorage (8). The bone-implant interface, particularly prone to mechanical vulnerabilities, frequently undergoes bone loss due to intricate interactions. Stress from implant loads is transferred to the cervical region, a phenomenon aligned with an engineering principle that highlights stress concentration at the junction of two materials. Compressive forces are essential for maintaining bone-implant integrity, whereas tensile forces could undermine it. Cortical bone exhibits greater resistance to compressive forces compared to shearing forces. Excessive stress, exceeding physiological thresholds, can accelerate bone resorption. Although normal stress levels are crucial for bone stability, an overload can disturb osteoclast activity, potentially resulting in considerable bone loss (3).
Stress distribution in bone around an implant is influenced by factors such as implant position, angulation, and the implant-abutment connection, as well as the magnitude of the occlusal load. Successful load transmission to the surrounding bone depends on the nature of the applied load, the design of the implant, and the biomechanical properties at the bone-implant interface. Immediate implants are more prone to biomechanical failures due to excessive micromotion, which highlights the critical need for primary stability and controlled micromotion to ensure the success of the implant. Consequently, optimizing the design of the implant is essential for maintaining bone integrity at the interface and for extending the overall longevity of the implant (9, 10). This approach helps in mitigating the risks associated with implant placement and in enhancing the functional lifespan of dental implants.
Review
The forces on a dental implant are transmitted to the adjacent biological tissues. The nature of implant biomechanics can be either reactive or therapeutic, focusing on biomechanical factors that may be harmful to implants and adjusting each factor to mitigate the overall response that leads to implant overload (11).
Peri-Implant Biology
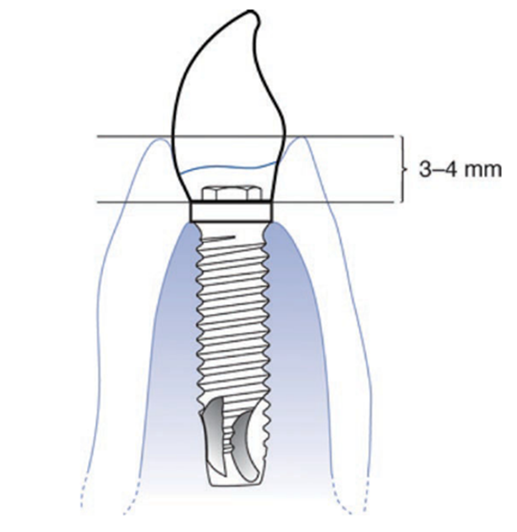
When replacing a tooth with Osseo integrated dental implants, it is essential to consider the biological principles of the adjacent soft and hard tissues. Inserting an implant between two periodontally healthy teeth ensures the maintenance of bone and soft tissue, partly due to the neighbouring teeth. Early research by Waerhaug (12) and Gargiulo and associates (13) identified the dent gingival complex's width around natural teeth as close to 3 mm. Although peri-implant tissues differ, Cochran and his team (14) found these tissues to approximate a similar width. Consequently, implants should be placed about 3–4 mm below the soft tissue's free margin (Figure 1) (15). This spacing accommodates the biological width, allows for proper restoration emergence and aesthetics, and facilitates the soft tissue and bone remodelling that occurs within 6 months to a year (16). The type of periodontium is thought to affect the extent of this remodelling, with thin, scalloped gingiva potentially receding more than thick, flat gingiva (17, 18).
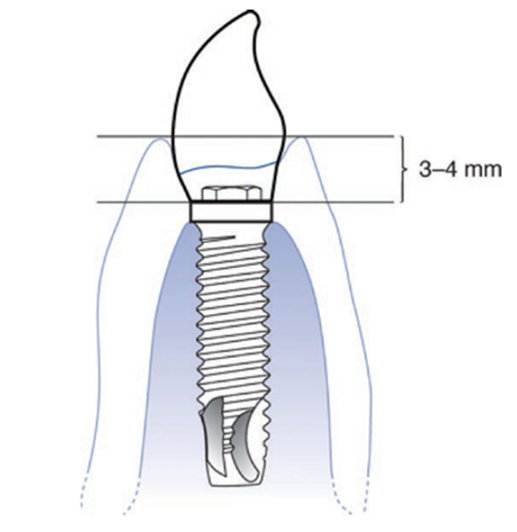
Figure 1: Osseo integrated implant placed at a depth of 3–4 mm for biologic width and emergence profile (15).
It is crucial to keep restorative interfaces with metal below the free margin of tissues due to expected remodelling. Tarnow and colleagues demonstrated a correlation between the underlying bone and soft tissue in the gaps between natural teeth (19). Connections between implant to natural tooth and implant to implant have also been shown (20). The recommended distance from the implant to the adjacent tooth is approximately 2 mm to prevent horizontal bone loss that could affect the neighbouring tooth. Furthermore, Tarnow and associates (20) identified that a critical distance of about 3 mm between implant surfaces is necessary to prevent the acceleration of lateral bone resorption that can negatively impact each implant (Figure 2) (15). Typically, each implant experiences peri-implant bone loss within the first year and then stabilizes, which is a key criterion for success as noted by Albrektsson and colleagues (21).
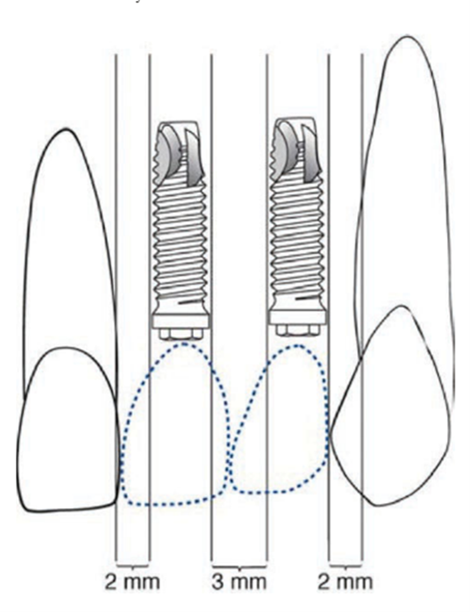
Figure 2: Suggested minimum distances of implant to natural tooth and implant to implant (15).
Patient factors
Evaluating soft tissue before implant placement is essential for long-term success and maintenance. Proper assessment of soft tissue and bone volume is essential for predicting long-term implant stability and aesthetic outcomes. Local and systemic conditions such as smoking, osteoporosis, periodontal disease, and bruxism also play critical roles in the success rates and longevity of implants. Additionally, conditions like diabetes and autoimmune disorders present challenges that require careful management to optimize implant success. Advances in implant surface technology have improved outcomes in patients with risk factors such as smoking. A comprehensive patient evaluation and tailored treatment planning are crucial to managing these factors effectively, ensuring the longevity of the implants, and enhancing the patient's overall quality of life (15).
Forces acting on the Implant
The forces exerted on a dental implant are vital considerations for its long-term stability and functionality. These forces can be categorized by type, direction, magnitude, duration, and the presence of any parafunctional forces. From the basic equation (Stress = Force ÷ Surface area), it becomes clear that reducing stress on the implant can be achieved either by increasing the functional surface area or by decreasing the force exerted (22). In 1989, Cowin noted that cortical bone has the highest strength under compression and is capable of effectively managing the stresses imposed by the bone-implant system (23). However, shear and tensile forces, which are angular and direct stress across the crestal bone and bone-implant interface, can be potentially harmful over time. An angled load of 30 degrees can result in a 50% increase in stress compared to a load applied along the implant's long axis (24).
The bite force is strongest in the molar region, reaching approximately 200 pounds, less in the canine area at about 100 pounds, and weakest in the anterior incisor area, ranging from 25 to 35 pounds (25). Under parafunctional habits such as bruxism, clenching, and tongue thrusting, these forces can escalate to 1000 pounds. These habits not only increase the magnitude but also the duration of bite forces, potentially exceeding the endurance limit of the implant components. This excessive stress can lead to complications such as screw loosening or fatigue failure of the implant components (26), underscoring the importance of managing these forces effectively to ensure the longevity and success of the implant.
Implant related factors
Implant design should aim to increase the surface area of the implant, thereby enhancing stress distribution and achieving better primary stability (22). Implant design is targeted at increasing the surface area, enhancing stress distribution, and achieving better primary stability. The macro design of dental implants involves specific thread shapes such as square, V-shape, buttress, and reverse buttress, which are key to facilitating easier insertion and efficient force transmission to the surrounding bone. These thread designs, using a rotational linear motion during placement, improve surface contact and minimize negative stimuli. Chia Ching Lee and colleagues utilized Finite Element Analysis to determine that the square thread design provides the largest contact area and reduces force dissipation around the marginal bone (27). Similarly, a study by Eraslan et al, using a 100 Nstatic axial load, found that this thread type also experiences the lowest stress concentrations at the cervical cortical regions near the first thread (28). Thread pitch and lead also play crucial roles; a smaller pitch results in a greater number of threads, which enhances the implant's surface area and improves load distribution (29). Paolo Trisi et al's study on sheep bone showed that larger threads significantly increase bone-to-implant contact and stability in low-density bone (30). The lead, or the distance a thread travels axially after one complete rotation, affects the implant's insertion speed and is critical for achieving primary stability.
Thread depth and width are critical parameters in implant design, as detailed by Misch. He defines thread depth as the distance from the outermost tip to the innermost body of the thread, and thread width as the distance between the highest and lowest points of a single thread, measured axially (31). Implants with shallow thread depths are easier to place in high-density bone, while those with deeper threads are preferable for low-density bone to enhance the functional surface area. A study by Sun-Young Lee et al. emphasized that deeper threads improve mechanical stability in low-density bone (27). Progressive threads, which gradually decrease in depth from the apical to the coronal end, are utilized in systems like Ankylos (Dentsply Friadent, Mannheim, Germany) to optimize engagement and stress distribution (32). Furthermore, implant dimensions such as length and width significantly influence implant stability and biomechanical performance. Increasing the length of an implant improves its initial stability by expanding the surface area, which enhances its resistance to torque and shear forces and promotes bicortical stabilization. Likewise, wider implants increase the bone contact area, aiding in the effective dispersal of forces. A study by Hamidreiza revealed that while implant length may not significantly impact primary stability in D1 type bone, in low-density bone, augmenting both the width and length of the implant is essential for achieving primary stability and reducing stress, thereby minimizing the risk of implant fracture (33). Additionally, the crest module, or the trans-osteal region of the implant, plays a pivotal role in surgical outcomes, biological width, and loading profiles, characterized by high mechanical stress, and serving as a barrier against bacterial and fibrous tissue ingress during initial healing.
Implants with a round cross-section need anti-rotational features to withstand torsional shear forces when abutment screws are tightened. The microtopography and nano topography of dental implants play critical roles in their success and integration. The microtopography of an implant is enhanced through techniques like sandblasting, acid etching, and grit blasting (22). These methods intentionally create imperfections on the implant's surface, which increase the surface area and improve the implant's ability to attract osteogenic cells necessary for bone formation. Moving to a smaller scale, implant nano topography involves detailed manipulations at the cellular and protein levels. Techniques like anodic oxidation, laser ablation, and TiO2 blasting are used to refine the implant surface. These methods have been demonstrated to prevent crestal bone loss and enhance the soft tissue seal around the implant, thereby improving its overall integration and longevity (34, 35). Additionally, the application of loading protocols significantly influences implant success.
Bone factors
Bone factors are critical for the successful placement and long-term stability of dental implants (Table 1). Bone factors help clinicians assess the potential challenges and requirements for implant procedures, ensuring optimal outcomes by matching implant characteristics with bone conditions (22).
|
Table 1. Summarizes the critical bone factors that influence the placement and success of dental implants (22) |
|
|
Bone Factor |
Description |
|
Bone Density |
Critical for implant success. Ideal placement occurs in structurally sound bone, sufficient in all dimensions. Challenges include width deficiencies, dimensional resorption, or complete alveolar bone resorption. |
|
Available Bone Height |
Measured from the crest of the ridge to an opposing anatomical landmark. High-density bone can accommodate shorter implants, while low-density bone may require longer implants for stability. |
|
Available Bone Width |
Determines the implant size. Wider ridges allow for larger-diameter implants, increasing surface area for load distribution and enhancing force dissipation. |
|
Available Bone Length |
The minimum required length is at least 8mm for adequate anchorage and support of the implant. |
|
Bone Angulation |
Bone should be perpendicular to the occlusal plane and aligned with occlusal forces to evenly distribute forces and minimize the risk of implant failure. |
Clinical Moment Arms
Clinical moment arms are the leverages exerted around an implant, crucial for understanding biomechanics in implant dentistry. These forces can induce microrotations and stress concentrations at the crest of the alveolar ridge, potentially leading to crestal bone loss due to the dynamic loads applied during mastication and other oral functions (22).
In implant dentistry, three clinical moment arms, occlusal height, cantilever length, and occlusal width are pivotal in managing the biomechanical integrity of dental implants. Occlusal height, the vertical distance from the implant platform to the occlusal plane, influences vertical lever arm effects and is affected by facio-lingual, mesio-distal, and vertical axes, which shape how occlusal forces are distributed during function and can impact the leverage of other forces. Cantilever length, which extends the prosthesis beyond the most distal implant, creates significant moment arms that increase mechanical failure risks, especially if the cantilever is extended beyond 2.5 times the anterior-posterior spread. This dimension is critical as off-center lingual forces can induce twisting moments at the implant neck, though direct forces over the implant typically do not induce moment loads or rotation. Occlusal width, the horizontal measurement across the occlusal surface, affects lateral force distribution; a wider occlusal table may increase facio-lingual tipping or rotation, whereas a narrower table promotes more centric contacts and enhances stability. Minimizing these dimensions is essential to prevent complications such as unretained restorations, component fractures, crestal bone loss, or complete failure of the implant system, making precise control of these moment arms crucial for long-term success (22).
Conclusion
The longevity and functionality of dental implants are deeply influenced by the precise management of biomechanical forces at the bone-implant interface. Understanding and optimizing these forces through advanced implant design and strategic placement are essential for enhancing implant success and patient satisfaction.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical Consideration
Not applicable.
Data Availability
Data that supports the findings of this study are embedded within the manuscript.
Author Contribution
The authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.