Volume 4, Issue 12
December 2024
Advances in Craniofacial Reconstruction: The Role of Augmented Reality
Yasser Eid Al-Thobaiti, Sultan Hamad Al-jery, Zakher Eid Alrayes, Dania Hamoud Aljeaid, Hamad Ibrahim Alzaydan
DOI: http://dx.doi.org/10.52533/JOHS.2024.41227
Keywords: Augmented reality, craniofacial reconstruction, surgical precision, 3D imaging, postoperative assessment
Advancements in augmented reality (AR) are transforming craniofacial reconstruction by enhancing precision, improving planning, and optimizing outcomes. AR integrates three-dimensional imaging with real-time overlays, allowing surgeons to visualize and interact with patient-specific anatomy during every phase of the surgical process. Preoperative planning benefits from AR’s ability to generate dynamic simulations of procedures, enabling surgeons to anticipate challenges and refine techniques. Virtual models derived from imaging modalities such as CT and MRI are used to assess bone alignment, symmetry, and graft positioning with remarkable accuracy. Collaborative planning becomes seamless as multidisciplinary teams interact with the same virtual models, improving communication and decision-making. Intraoperatively, AR provides real-time guidance through overlays projected onto the surgical site. This technology facilitates precise osteotomies, graft placements, and soft tissue manipulation while preserving vital structures such as nerves and blood vessels. Head-mounted displays and markerless tracking systems enhance usability, enabling surgeons to maintain focus on the operative field. AR’s integration with robotic systems further improves precision, particularly in minimally invasive procedures where access to deep anatomical structures is limited. Postoperative assessment leverages AR for detailed comparisons between preoperative plans and surgical outcomes. Healing progress, such as bone remodeling and graft integration, can be tracked dynamically, offering insights into recovery. AR-based telemedicine platforms also enable remote monitoring, reducing the need for frequent in-person follow-ups while maintaining consistent care. Despite challenges related to cost and accessibility, AR’s transformative impact on craniofacial reconstruction is undeniable. Its ability to enhance visualization, streamline workflows, and improve patient outcomes highlights its potential to redefine surgical standards. As technology continues to evolve, AR is set to become an indispensable tool in advancing the precision and effectiveness of craniofacial surgery.
Introduction
Craniofacial reconstruction is a multifaceted domain of surgical intervention that aims to restore both function and aesthetics in patients with congenital anomalies, trauma-related deformities, or oncological resections. This field has witnessed substantial advancements over the years, driven by technological innovations that enhance surgical precision and optimize patient outcomes. Among these, augmented reality (AR) has emerged as a transformative tool, offering unparalleled opportunities for visualization, planning, and execution in craniofacial surgery.
Augmented reality integrates virtual information into the real-world environment, allowing surgeons to access critical data in real-time without diverting their attention from the surgical field. This technology is distinct from virtual reality, which immerses users in a completely synthetic environment, and it holds particular promise in craniofacial surgery due to the complexity of the anatomical structures involved. AR enables precise mapping of anatomical landmarks, which is crucial for surgeries that require meticulous reconstruction of facial symmetry and function (1). The application of AR in craniofacial reconstruction begins with preoperative planning, where advanced imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) are utilized to create three-dimensional (3D) models of the patient's anatomy. These models can then be superimposed onto the surgical field via AR, enabling surgeons to visualize the underlying structures with remarkable clarity. Such visualization is particularly beneficial in complex cases involving severe trauma or congenital deformities, where conventional imaging might not provide sufficient spatial context (2). Additionally, AR allows for dynamic manipulation of these models, enabling surgeons to simulate various surgical approaches and anticipate potential challenges before the actual procedure.
Intraoperative use of AR has also gained traction in recent years. By overlaying critical anatomical information directly onto the surgical site, AR assists surgeons in achieving greater precision during osteotomies, graft placements, and soft tissue reconstruction. For instance, AR can project virtual guides onto bone surfaces, ensuring accurate cutting angles and minimizing errors. Furthermore, this technology reduces dependency on external monitors, streamlining workflows and potentially shortening operative times. Studies have demonstrated that the use of AR in craniofacial procedures not only enhances surgical accuracy but also reduces the risk of complications associated with misalignment or incomplete reconstruction (3).
Postoperative assessment is another area where AR is proving to be invaluable. By comparing preoperative and postoperative 3D models, surgeons can objectively evaluate the outcomes of their interventions and identify areas for improvement. AR-based tools also have the potential to improve patient communication by providing visual representations of surgical outcomes, thereby setting realistic expectations and enhancing patient satisfaction. Moreover, the integration of AR into telemedicine platforms has opened new avenues for remote surgical planning and consultation, further broadening its impact on the field (4). Despite its potential, the adoption of AR in craniofacial reconstruction is not without challenges. High costs, technical limitations, and the need for specialized training remain significant barriers to widespread implementation. However, as technology matures and becomes more accessible, it is poised to play an increasingly central role in craniofacial surgery, driving the field toward a new era of precision and innovation.
Review
Augmented reality (AR) has become a transformative tool in craniofacial reconstruction, providing surgeons with enhanced visualization and precision. By integrating three-dimensional (3D) imaging with real-time overlays, AR allows detailed mapping of complex anatomical structures, aiding in both preoperative planning and intraoperative guidance. Studies have highlighted its ability to improve surgical outcomes by reducing errors and enhancing spatial awareness. For instance, AR enables precise alignment of bone fragments in trauma cases, ensuring better symmetry and function (5). Additionally, AR-based systems reduce dependency on external navigation tools, streamlining surgical workflows and potentially shortening operative durations.
Intraoperative AR applications, such as projecting cutting guides or virtual templates onto bone surfaces, have been shown to improve accuracy in osteotomies and graft placements. This not only minimizes the risk of complications but also enhances aesthetic outcomes, which are critical in craniofacial reconstruction. Postoperative assessments also benefit from AR through comparisons of preoperative and postoperative models, allowing for more objective evaluations of surgical success (6). Despite its promise, challenges remain, including high implementation costs and the need for specialized training. Nevertheless, with continuous advancements in AR technology, its integration into routine clinical practice is likely to grow, paving the way for more precise and patient-centered craniofacial procedures.
Technological Foundations of Augmented Reality in Craniofacial Surgery
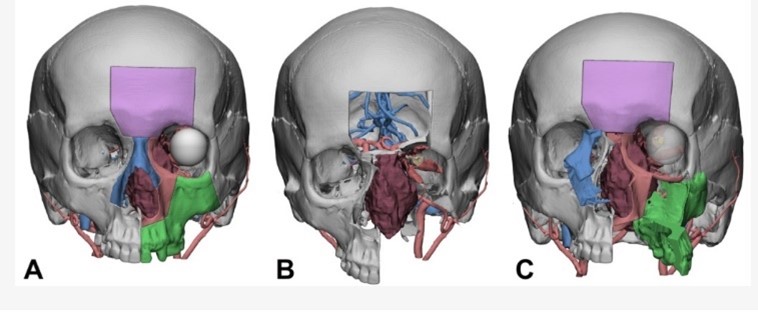
Augmented reality (AR) has emerged as a sophisticated technological innovation in craniofacial surgery, leveraging advanced imaging and computational techniques to enhance surgical precision. By integrating real-world visuals with digital overlays, AR provides a transformative platform that bridges the gap between virtual preoperative planning and real-time surgical execution. This process begins with the creation of high-fidelity three-dimensional (3D) models derived from imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI). These models form the backbone of AR applications, offering surgeons an accurate representation of a patient’s anatomy to navigate complex craniofacial structures effectively (7). For instance, Tel A. et al, in their report of a case series of 4 patients who underwent craniofacial oncologic surgery, they were able to split the midface in a maxillary cheek flap and a contralateral nasal–maxillary cheek flap using AR and implement it on real time surgery (Figure 1) (8).

Figure 1: Virtual surgical planning for facial disassembly to be imported in AR headset. (A) osteotomies are traced in VSP software; (B) all bone flaps are removed (purple—frontal bone flap; blue—nasal bridge; red—subspinal medial orbital wall flap; green—maxilla flap), leaving the tumor (brown) visible in its relationships with the surrounding structures; (C) facial translocation is simulated, pivoting and rotating bone segments according to the surgical prediction (8).
One of the critical components of AR is its tracking and registration systems, which ensure that virtual elements align seamlessly with the surgical field. Marker-based systems, such as optical or electromagnetic trackers, are commonly used to maintain spatial accuracy. However, recent advancements have moved toward markerless technologies, relying on advanced algorithms to recognize anatomical landmarks directly. This evolution not only reduces the need for invasive attachments but also increases the adaptability of AR systems in dynamic surgical environments. For instance, markerless approaches have demonstrated promising results in maintaining alignment during procedures requiring frequent movement of surgical instruments or patient repositioning (9).
The integration of AR into surgical workflows often involves the use of head-mounted displays (HMDs) or projector-based systems. HMDs, such as Microsoft HoloLens or Magic Leap, enable surgeons to visualize virtual guides and annotations directly within their field of view. This eliminates the need for external monitors, reducing cognitive distractions and improving procedural focus. Projector-based AR, on the other hand, casts digital overlays directly onto the surgical site, providing a more intuitive and collaborative environment for surgical teams. Both methods aim to enhance precision and reduce reliance on manual measurements, which is especially critical in cases requiring symmetry restoration, such as cleft palate repairs or post-traumatic reconstructions (10).
Beyond visualization, AR technologies are increasingly incorporating artificial intelligence (AI) and machine learning algorithms to enhance their utility. These algorithms can process vast amounts of imaging data to identify key anatomical features, predict surgical outcomes, and provide real-time feedback. For example, AI-driven AR systems have been developed to automate the identification of cranial sutures and mandibular landmarks, significantly reducing the time required for surgical planning. Additionally, these systems are capable of adapting to intraoperative changes, such as tissue swelling or unexpected anatomical variations, ensuring consistent accuracy throughout the procedure (11). While AR technology continues to evolve, challenges related to latency, resolution, and user adaptability remain focal points for improvement. Current systems are being optimized to deliver faster response times and higher resolution overlays, addressing surgeon feedback regarding usability. Furthermore, ergonomic considerations, such as the weight and comfort of HMDs, are being prioritized to ensure seamless adoption in prolonged surgical procedures. Developers are also focusing on refining intuitive interfaces that require minimal training, allowing surgeons to interact effortlessly with virtual elements without disrupting the surgical flow (12, 13).
Preoperative Planning and Simulation Using Augmented Reality
Preoperative planning is a cornerstone of successful craniofacial reconstruction, and the integration of augmented reality (AR) into this phase has introduced a new dimension of precision and interactivity. By transforming static imaging data into dynamic, three-dimensional (3D) models, AR enables surgeons to gain an unparalleled understanding of the patient’s unique anatomy. This capability is particularly beneficial in craniofacial surgery, where even minor deviations can significantly affect aesthetic and functional outcomes. Advanced AR systems use imaging modalities like computed tomography (CT) and magnetic resonance imaging (MRI) to generate patient-specific 3D models, which are then visualized in an immersive environment (14, 15).
One of the significant advantages of AR in preoperative planning is its ability to simulate surgical procedures virtually. Surgeons can rehearse complex reconstructions by interacting with 3D models, manipulating them in real time to explore different surgical approaches. For example, AR can overlay virtual osteotomy lines onto the model, allowing surgeons to assess the feasibility and implications of various cutting angles. This simulation helps identify potential complications and optimizes the surgical strategy. In cases of severe craniofacial trauma, AR systems have been used to reconstruct shattered bone fragments virtually, facilitating the planning of precise repositioning during surgery (16, 17).
The use of AR in this phase extends beyond visualization to functional simulations. For instance, AR-based tools can predict the biomechanical outcomes of planned reconstructions, such as the impact of graft placements on facial symmetry and jaw movement. This predictive modeling is powered by advanced algorithms that incorporate factors like bone density, tissue elasticity, and expected healing patterns. Such simulations enable a more informed decision-making process, reducing uncertainties and enhancing patient outcomes. Furthermore, AR can simulate aesthetic results, providing a visual representation of postoperative appearances that can be shared with patients to align expectations (18).
Collaboration among multidisciplinary teams is critical in craniofacial surgery, and AR fosters this by creating shared, interactive environments. Surgeons, radiologists, and prosthetists can simultaneously interact with the same virtual model, discussing and refining the surgical plan. AR tools also allow for remote collaboration, where specialists from different locations can contribute to the planning process in real time. This capability has proven invaluable in complex cases requiring expertise from multiple subspecialties, such as maxillofacial surgeons, orthodontists, and neurosurgeons. Collaborative planning using AR not only improves surgical precision but also enhances the efficiency of team communication (18, 19).
The integration of AR into preoperative planning has also advanced patient engagement. Through AR, patients can visualize the planned procedure and its expected outcomes, gaining a clearer understanding of the surgical process. This transparency builds trust and enhances patient compliance with postoperative care instructions. For pediatric cases, where parents often have heightened concerns, AR visualization helps explain complex procedures in an intuitive manner, alleviating anxiety and fostering informed consent. Additionally, AR simulations allow surgeons to demonstrate the surgical strategy, helping patients understand the rationale behind specific approaches (18). Despite its significant potential, AR's integration into preoperative planning is still evolving. Technical challenges, including the time required to generate detailed models and the computational power needed for real-time simulations, remain barriers. However, as AR technology continues to advance, its role in preoperative planning is likely to expand, setting a new standard for precision and patient-centered care in craniofacial surgery.
Intraoperative Applications: Enhancing Precision and Efficiency
The use of augmented reality (AR) during craniofacial surgeries has transformed intraoperative workflows, offering surgeons tools to enhance precision and streamline complex procedures. By integrating real-time data with the surgical field, AR overlays critical information directly onto the operative site, eliminating the need to shift focus to external monitors. This fusion of virtual and physical realities enables a more intuitive surgical experience, allowing surgeons to maintain spatial awareness and execute maneuvers with greater accuracy. Advanced AR systems utilize high-resolution tracking devices to ensure that the projected overlays are dynamically aligned with the patient’s anatomy, even during slight movements (19).
Intraoperative AR finds extensive use in guiding osteotomies and graft placements. The technology allows for the projection of virtual cutting guides and alignment markers onto bone surfaces, ensuring precise execution of planned procedures. For instance, in mandibular reconstructions, AR systems can display real-time templates for resection lines, reducing the risk of misalignment or excessive bone removal. Additionally, AR assists in the placement of autologous or alloplastic grafts by highlighting optimal positioning based on preoperative simulations. This capability is particularly crucial in surgeries requiring restoration of facial symmetry, where millimeter-level accuracy can significantly influence outcomes (20).
Soft tissue manipulation, another critical aspect of craniofacial surgery, also benefits from AR-guided workflows. By overlaying virtual reconstructions of soft tissue contours, AR enables surgeons to visualize the expected postoperative appearance during the procedure. This dynamic guidance ensures that adjustments made to soft tissues, such as skin or muscle flaps, align with the planned aesthetic outcomes. Furthermore, AR systems equipped with tissue-tracking algorithms adapt to real-time changes in the surgical field, maintaining the accuracy of overlays even as tissues are manipulated or retracted. Such adaptability minimizes intraoperative guesswork and enhances the surgeon’s confidence in achieving desired results (21).
Another area where AR excels is in the identification of vital structures such as nerves, blood vessels, and sinuses. The visualization of these structures through AR reduces the likelihood of accidental injury, a significant concern in craniofacial procedures due to the intricate anatomy involved. For example, AR can project the location of the inferior alveolar nerve during mandibular surgeries, helping surgeons avoid nerve damage while performing osteotomies or implant placements. Similarly, AR-guided visualization of blood vessels aids in preserving vascular integrity, which is critical for graft viability and overall healing (22).
The integration of AR into robotic surgical systems has further enhanced its intraoperative applications. Robotic platforms equipped with AR capabilities allow surgeons to execute procedures with unparalleled precision by combining the dexterity of robotic arms with the real-time guidance provided by AR. These systems are particularly advantageous in minimally invasive craniofacial surgeries, where access to deep-seated structures is limited. AR-guided robotic tools can navigate these confined spaces with exceptional accuracy, reducing trauma to surrounding tissues and expediting recovery times (23). Ensuring seamless integration with existing surgical instruments, minimizing latency in dynamic overlays, and addressing ergonomic concerns associated with head-mounted displays are ongoing areas of development. Nonetheless, the current applications of AR in craniofacial surgery underscore its potential to redefine intraoperative standards, ultimately contributing to improved surgical outcomes.
Postoperative Assessment and Patient Outcomes
Incorporating augmented reality (AR) into postoperative care has redefined the way outcomes are evaluated in craniofacial surgery. AR technologies provide surgeons with the ability to compare preoperative plans and actual postoperative results through detailed overlays of three-dimensional (3D) models. This direct visual comparison helps identify deviations in anatomical reconstruction, alignment, and symmetry. For example, discrepancies in bone position or graft integration can be easily detected using AR-enhanced imaging, offering a level of precision unattainable through conventional methods (23).
Detailed monitoring of bone healing and tissue integration has become more efficient with AR tools. These systems dynamically visualize the interaction between grafted materials and surrounding tissues, tracking changes over time. Surgeons can assess the degree of osseointegration in implants or observe the remodeling process of bone grafts in real-time. This functionality enhances the ability to detect subtle issues, such as incomplete integration or misalignment, which might otherwise go unnoticed in traditional postoperative imaging (24, 25). Functional recovery is another crucial aspect of postoperative assessment where AR plays a transformative role. By integrating motion-tracking systems, AR allows for precise evaluation of facial and jaw movements.
AR significantly enhances communication with patients and their families during the recovery phase. Visualizing surgical outcomes through AR offers a clear representation of progress, enabling better understanding of the healing process. For instance, patients can see a comparison of their preoperative and current anatomy, helping them grasp the extent of their recovery. In pediatric cases, this technology is particularly impactful, as parents can observe improvements in their child’s facial symmetry or bone integration, fostering greater trust in the treatment process and alleviating anxiety (14, 26).
The long-term potential of AR extends to remote follow-ups and monitoring, ensuring consistent postoperative care even for patients who cannot attend frequent in-person visits. Telemedicine platforms enhanced with AR allow patients to upload images or videos of their recovery for real-time evaluation by their healthcare providers. Surgeons can assess subtle changes in soft tissue or bone structure remotely, ensuring early intervention when needed. This remote capability not only reduces the burden of travel for patients but also streamlines postoperative workflows, making follow-up care more efficient. The versatility of AR in postoperative applications continues to grow, enabling healthcare teams to refine their approach to patient recovery. By providing accurate visualizations, tracking functional progress, and facilitating remote care, AR is shaping a more interactive and data-driven model for assessing surgical outcomes.
Conclusion
Augmented reality is revolutionizing craniofacial surgery, offering advancements from preoperative planning to postoperative assessment. By enhancing precision, enabling dynamic simulations, and improving patient engagement, AR addresses both technical and aesthetic challenges in complex cases. Despite current limitations in accessibility and cost, ongoing innovations are paving the way for its widespread adoption. AR’s integration into craniofacial reconstruction is transforming the field, promising improved outcomes and more personalized care for patients.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.