Volume 1, Issue 7
October 2021
The Impact of Obesity on Total Knee Replacement
Syed Hasan, Hatim Alhazmi, Muaath Alrehaili, Husam Tamim, Ahmed Alhusayni , Marwan Almohammadi, Omar Owaidah
DOI: http://dx.doi.org/10.52533/JOHS.2021.1702
Keywords: obesity, total knee replacement, management, complications, osteoarthritis
Worldwide estimates indicate the high prevalence of obesity and overweight, and some countries even consider it a pandemic. Obesity is correlated with many disorders like hypertension, diabetes, osteoarthrosis of the knee, and coronary artery disease. Many investigations have been published to study the impact of and correlation between obesity and total knee arthroplasty procedures. Evidence is contradicting regarding the perioperative outcomes in these patients. In the present study, we have conducted a literature review to elaborate on the effects of obesity on total knee arthroplasty. Obesity can be considered as the single modifiable risk factor for performing osteoarthritis-induced total knee arthroplasty. Evidence regarding the effect of obesity on the perioperative outcomes and revision approach following a total knee arthroplasty contradicts as many studies reported that the impact is not significant while others indicated the opposite. According to the various risks that obesity poses on the patients’ general condition and the potential adverse impact on the outcomes of the surgery, we recommended that weight gain should be conducted before the patient has been indicated to perform the surgery, which was also validated by previous investigations. However, evidence regarding this is still scarce in the current literature and further investigations are needed.
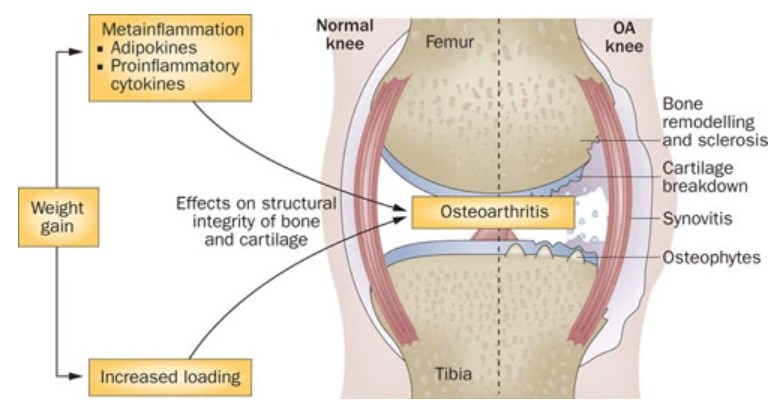
Worldwide estimates indicate the high prevalence of obesity and overweight, and some countries even consider it a pandemic. For instance, in the United States, it has been demonstrated that 33.9% of the adult population suffers from obesity (1). Body mass index has been used as a valid measure to adequately define obesity and overweight (Figure 1) (2). Obesity is correlated with many disorders like hypertension, diabetes, osteoarthrosis of the knee, and coronary artery disease.
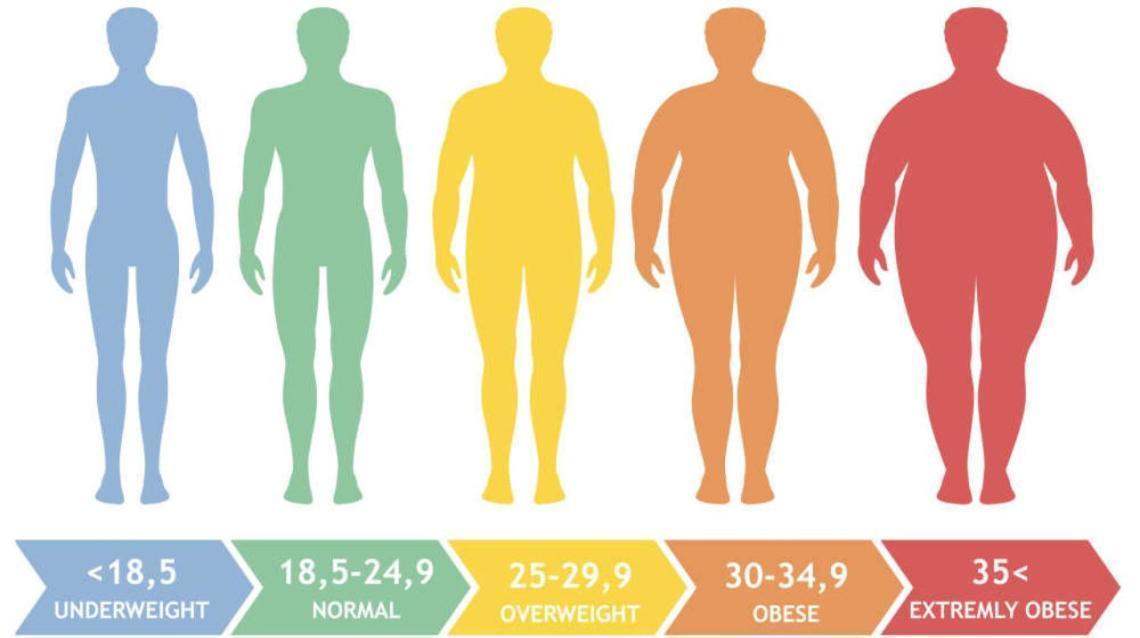
Figure 1. Interpretation of the body mass index.
Estimates indicate that obesity is a major contributor to the development and prognosis of osteoarthrosis (3). It has been furtherly demonstrated that up to 60% of the patients who underwent total knee replacement procedures suffer from obesity (4-6). A previous comparative Canadian investigation indicated that the risk of needing a total joint replacement procedure was 8.53 folds higher in obese patients than the normal population in this investigation (7). The authors also estimated that the risk even doubled with the different classes of obesity, based on the higher body mass indices.
Many investigations have been published to study the impact of and correlation between obesity and total knee replacement procedures. Evidence is contradicting regarding the perioperative outcomes in these patients. Therefore, we aimed to conduct this investigation to adequately discuss the effect of obesity on total knee arthroplasty based on evidence from the current studies in the literature.
Review
Evidence shows that performing total knee replacement in obese patients is associated with various challenges to the performing surgeons. Most of these challenges are associated with difficulties in procedures regarding surgical exposure. It should be noted that body mass index might not be a significant predictor for the development of these complications or the success of the procedure because having an index >35 might be associated with a non-pathological distribution of the body fat. For instance, many patients might carry their excess adipose tissue in the abdominal region while having thin extremities, and therefore, this might not have a significant risk over their limbs (8). It has been furtherly demonstrated that having a suprapatellar index <1.6 is significantly associated with increased tourniquet time. Therefore, we decided to provide further evidence regarding the impact of obesity on the need to perform total knee replacement and the impact on the perioperative outcomes based on evidence obtained for the relevant investigations in the literature.
Many studies have been identified about our intended outcomes. These investigations have validated evidence regarding the impact of obesity and the associated clinical parameters on total knee replacement events. Many of the included studies in the literature reported no significant adverse events or complications related to the procedure of total knee replacement when performed in obese patients (9-14). The functional outcomes following TKA were not significantly adversely impacted by the patients’ body weight or body mass index at 1, 3, 6, and 12 months (11, 15, 16). It has also been indicated that favorable outcomes regarding the Short Form-12 Health Survey score, Knee Society Score, Hospital for Special Surgery score, Western Ontario and McMaster Universities Arthritis Index, and pain prognosis at 2 and 5 years following the operation were also noticed and were not significantly impacted by obesity or body mass index (7, 9, 13). Furthermore, studies also indicated that the functional outcomes and symptoms were also significantly relieved among morbidly obese and obese patients following 3 years from performing total knee replacement similar to other populations (17, 18). Accordingly, it has been concluded among the different investigations that obese patients should not be excluded from performing total knee replacement procedures because the reported favorable outcomes did not significantly differ from other patients with lower body mass index scores (12, 19). It has been furtherly demonstrated that both non-obese and obese patients did not significantly differ in the rates of perioperative complications in the settings of total knee replacement procedures (17, 20-22). Long- and mid-term survival rates were also comparable among the two groups (7, 10, 22, 23), although it has been demonstrated that early complications and body mass index were weakly correlated (21). A report also showed that for non-obese and obese patients, the Kaplan Meier survivorship was 95% for both groups with any re-operative procedure as the significant endpoint (7).
On the other hand, it should also be noted that many other investigations have also reported that obesity adversely impacted the outcomes of total knee replacement procedures and that obese patients had significantly more poor outcomes than the non-obese population (5, 24-28). Lower post total knee replacement procedures were significantly reported with obese patients (24). These studies also showed that satisfaction levels, quality of life for patients, and functional outcomes following total knee replacement procedures were significantly adversely impacted by the patients’ body weight and body mass index (25, 27). The clinical outcomes among obese patients that also suffered from diabetes as associated comorbidity were also significantly impacted (29). In an investigation by Issa et al. (30), the authors reported that obese patients had significantly more complications than patients in the non-obese group (10.5% versus 3.8%), in addition to significantly having more reduced post-total knee replacement activity scores than the non-obese population, as well. Following total knee replacement by 3 years, the analysis by Jones et al. (28) indicated that severe obesity could be considered a significant risk factor for predicting slow recovery and the related prognostic outcomes. Increased rates of hypertension and diabetes were also observed to be more significant in the obese group. A previous investigation by Namba et al. (5) estimated that obese patients had an increased risk of infection by 6.7 times than those with the non-obese group. This has been furtherly indicated in another investigation by Dowsey et al. (6), which reported that the increased rates of infections were associated with the presence of diabetes in obese patients that are indicated for total knee replacement procedures. A previous investigation also compared the obese and non-obese patients in terms of the outcomes related to undergoing the total knee replacement procedure. It has been reported that the total rates of complications were 10-30% in the morbidly obese group. Moreover, the authors estimated that the obese group had a 3-9 time increased rates of deep prosthetic infections than the other group (31). An estimated odds ratio of 1.9 and 2.38 were also estimated for developing infections and deep infections, respectively, in the obese group undergoing total knee replacement procedures (32). Liljensøe et al. (33) furtherly explained that following total knee replacement by 3-5 years, reduced quality of life and worsened clinical outcomes were significantly associated with an increased body mass index. Accordingly, evidence shows that recommendations should be provided to obese patients about the risk of developing infections following total knee replacement (34, 35). Increased rates of early complications were also significantly associated with the morbidly obese group. Some of these complications include abdominal or gastrointestinal pain and diarrhea, peripheral edema, extra-surgical site infections, wound infections and inflammation, and respiratory tract infections (36). However, it should be noted that there was no significant increase in the risk of developing neither bleeding nor venous thromboembolic events. On the other hand, an investigation by Guan et al. (24) reported that the risk of developing deep venous thrombosis was significantly associated with obesity. As a result of these events, Samson et al. (31) suggested that obese patients should lose weight amid performing total knee replacement procedures and explained how bariatric surgeries can be beneficial in these situations. Postoperative limb alignment has been reportedly associated with the body mass index of the patients and the preoperative limb alignment before total knee replacement procedures (37). Another investigation by Bozik et al. (38) also concluded that the risk of performing revision total knee replacement is significantly increased in obese patients 12 months after the operation.
The long-term outcomes of primary total knee replacement can be significantly impacted by the body weight and body mass index as these aforementioned investigations have demonstrated (25). Revision of the total knee replacement procedures was also investigated by many previous investigations. It is defined as a surgical practice that is usually done to remove or exchange the underlying complications of any underlying etiology. It is worth mentioning that an investigation by McElroy et al. (39) showed that reduced implant survivorship was significantly more prevalent in the morbidly obese than the obese and non-obese patients at 5 years following total knee replacement procedures. Kim et al. also indicated that morbidly obese patients had a significant increase in the consumption of hospital resources by 7% more than the non-obese population (40). Higher episodes of care costs and costs related to inpatient index surgeries were also significantly higher in obese patients in these settings (41). It has been demonstrated that the odds ratio for performing these approaches was 1.3, which was significantly higher in the obese than the non-obese population (32).
There is no doubt that obesity can adversely impact the functional outcomes of the joints of the affected patients and can progressively worsen the manifestations of osteoarthritis (Figure 2), which increases the risk of being indicated to perform total knee arthroplasty. In this context, a previous meta-analysis indicated that improved joint functions and reduced symptoms of obesity-related osteoarthritis were significantly improved in association with weight loss of the affected patients (42). Not many investigations have evaluated the efficacy of weight reduction on the outcomes of total knee replacement procedures. Among the very few investigations, Jin et al. (43) reported that losing >7.5% of the total weight in obese middle-aged and older adults reduced the risk of having total knee replacement procedures secondary to osteoarthritis more than other patients with a less notable weight reduction. Besides, it has been also demonstrated that the risk of having a total knee replacement in this population was not significantly impacted by neither gaining >5% nor losing 5-7.5% of the total body weight.

Figure 2. Association between obesity and osteoarthritis (44).
Based on this evidence, it can be concluded that obesity is an independent modifiable, and perhaps the only, risk factor for osteoarthritis-indicated total knee replacement. Accordingly, as a result of these findings, in addition to the well-known fact that obesity is also a risk factor for developing surgical and non-surgical complications (45-47), clinicians should exert serious efforts to encourage their obese patients to lose weight before conducting total knee replacement procedures rather than after it to achieve better interventions and reduce the risk of complications. Improved morbidity and enhanced symptomatology can be significantly enhanced after obesity has been significantly alleviated and weight loss has been significantly achieved using expert opinion in this field. This can also reduce the risk of having a total knee replacement procedure, and if indicated, the risk of operative complications would be significantly reduced. In this context, a previous cohort investigation reported that postoperative infection rates were significantly reduced by 3.5 times, and hospital admission rates were also significantly reduced by 7 times after weight reduction has been achieved using bariatric surgeries in their included population (48). These results were observed in a super obese population that was indicated to total joint arthroplasty at 30 days following the operation. Among the different obesity-related diseases, evidence indicates that obesity, in many cases, is the first presenting manifestation in these patients. However, it should be noted that not many patients are aware of the fact that they are obese and also of the impact of obesity on their health and the potential complications. Accordingly, clinicians and surgeons have a critical role in raising awareness among these patients and educating them about the potential risk that the disease might have (49).
Conclusion
Obesity can be considered as the single modifiable risk factor for performing osteoarthritis-induced total knee arthroplasty. Evidence regarding the effect of obesity on the perioperative outcomes and revision approach following a total knee arthroplasty is contradicting as many studies reported that the impact is not significant while others indicated the opposite. According to the various risks that obesity poses on the patients’ general condition and the potential adverse impact on the outcomes of the surgery, we recommended that weight gain should be conducted before the patient has been indicated to perform the surgery, which was also validated by previous investigations. However, evidence regarding this is still scarce in the current literature and further investigations are needed.
Disclosure
Statement:
The authors declare no conflict of interest.
Funding:
There has been no significant financial support for this work that could have influenced its outcome.
Ethical Consideration:
Non applicable.
Data Availability:
All data is found within the article.
Author Contribution:
All authors contributed to data collection, analysis, writing and drafting of the manuscript.