Volume 4, Issue 12
December 2024
Role of Molar and Mandibular Distalization in Orthodontic Treatment
Zainab Mahdi Al-Musally, Kifayah Abdulaziz Alfaran, Zahra Hassan Alosaif, Lojain Hassan Alam, Fahad Abdulrahman Alghamdi, Ayah Abdullah Alshams
DOI: http://dx.doi.org/10.52533/JOHS.2024.41246
Keywords: Molar distalization, mandibular distalization, orthodontic treatment, skeletal anchorage, malocclusion correction
Molar and mandibular distalization are essential techniques in orthodontic treatment, primarily employed to address malocclusions, space discrepancies, and crowding while preserving the integrity of the dental arch. Molar distalization facilitates the correction of Class II malocclusions by moving the maxillary molars distally, often using appliances like the pendulum, distal jet, or miniscrews. These methods create additional space in the anterior region and improve occlusal alignment without resorting to extractions. Mandibular distalization, though more challenging due to anatomical and biomechanical constraints, has seen advancements through skeletal anchorage systems, such as miniscrews and miniplates, enabling precise posterior movement of mandibular molars. The clinical applications of distalization techniques extend to treating various malocclusions, with case selection heavily dependent on skeletal relationships, crowding severity, and patient-specific factors. Younger patients benefit from skeletal growth potential, enhancing treatment outcomes, while adult patients often require customized appliances and meticulous biomechanical planning to overcome limitations like denser bone and reduced adaptability. Key considerations include anchorage management, anatomical boundaries, and maintaining long-term stability of distalized teeth. Technological advancements, including three-dimensional (3D) imaging based appliances, have refined these techniques, allowing for precise force application and improved patient comfort. However, challenges such as relapse, unwanted tipping, and anchorage loss persist, underscoring the need for robust retention protocols. Research into bioadaptive materials, enhanced force systems, and artificial intelligent-driven treatment planning is shaping the future of distalization, offering promising solutions to current limitations. These innovations hold potential to optimize outcomes, reduce side effects, and enable more individualized orthodontic care. Distalization techniques continue to evolve, providing effective alternatives to extraction-based treatment and contributing to the broader goal of achieving functional and aesthetic harmony in orthodontics.
Introduction
Orthodontic treatment aims to achieve functional occlusion, facial aesthetics, and periodontal health. Among the many approaches utilized, molar and mandibular distalization have gained considerable attention as techniques to correct malocclusions, particularly in cases involving space discrepancies, crowding, or excessive overjet. These methods are often employed to avoid extraction, reduce anterior dental crowding, or correct Class II molar relationships, thereby preserving the integrity of dental arches and ensuring long-term stability. Molar distalization is a key orthodontic strategy in correcting dental Class II malocclusion, where the maxillary molars are moved distally without extractions. This movement creates additional space in the anterior segment, reducing crowding and aligning teeth more effectively. Several methods for achieving molar distalization include intraoral appliances such as distal jet, pendulum appliances, and miniscrew-assisted techniques, as well as extraoral anchorage like headgear. Each technique is selected based on patient-specific factors such as age, skeletal maturity, and malocclusion severity, balancing treatment efficiency with minimizing undesired tooth movements (1).
Mandibular distalization, though less common due to the anatomical and biomechanical challenges associated with distalizing mandibular teeth, has seen advancements in technique and technology. Skeletal anchorage systems, such as miniscrews and plates, have significantly improved the feasibility of mandibular distalization by providing stable anchorage points. These innovations address the difficulties of achieving distal movement in a narrow mandibular arch and minimizing reciprocal movements that could compromise overall treatment outcomes (2). Mandibular distalization can be particularly beneficial in borderline cases where extraction might otherwise be indicated, offering a non-invasive alternative for space creation. The role of molar and mandibular distalization extends beyond achieving space in the dental arch; it also influences facial esthetics and occlusal harmony. Correcting sagittal discrepancies without extractions has implications for facial soft tissue profiles, particularly in young patients, as it avoids the risk of unfavorable aesthetic outcomes associated with extraction-based treatments. Moreover, distalization may offer functional benefits, such as improved occlusal relationships, reduced temporomandibular joint stress, and better masticatory efficiency. However, the success of these approaches depends on meticulous treatment planning, appliance selection, and close monitoring to prevent unwanted side effects, such as tipping or rotation of distalized teeth (3).
Despite the benefits, molar and mandibular distalization are not without limitations. The extent of achievable distalization is often restricted by anatomical structures like the maxillary sinus or mandibular ramus. Furthermore, maintaining the stability of distalized teeth in the long term remains a challenge, necessitating robust retention protocols. Continued research and innovation in distalization techniques, materials, and biomechanics are essential to address these limitations and optimize patient outcomes (4).
Review
The implementation of molar and mandibular distalization in orthodontic treatment has revolutionized non-extraction strategies for managing various malocclusions. Advances in distalization techniques have provided clinicians with alternative methods to achieve space creation and sagittal correction while preserving the integrity of dental arches. Molar distalization, often achieved using intraoral appliances such as the distal jet or pendulum, facilitates Class II correction by distalizing maxillary molars to create anterior space. These techniques have proven effective in treating crowding and overjet without extractions, although care must be taken to manage side effects such as anterior anchorage loss or undesired tipping (5). In contrast, mandibular distalization presents unique challenges due to the anatomical constraints and biomechanical complexity of the mandible.
The advent of skeletal anchorage systems, such as miniscrews, has expanded the feasibility of mandibular distalization by providing robust anchorage to overcome these challenges. These methods allow precise tooth movement while minimizing reciprocal forces, enhancing treatment outcomes for complex malocclusions. However, long-term stability of distalized teeth remains a concern, emphasizing the need for comprehensive retention strategies and regular follow-ups (6). As these techniques evolve, their integration with digital technologies and customized appliances promises greater precision, efficiency, and patient satisfaction in orthodontic care.
Mechanisms and Techniques for Molar and Mandibular Distalization
The methodologies for molar and mandibular distalization have significantly evolved, combining biomechanics, innovative appliances, and anchorage systems to address malocclusions effectively. Understanding these mechanisms is essential for clinicians to tailor treatment approaches that achieve precise and predictable outcomes while minimizing adverse effects. Molar distalization relies on controlled forces to move the maxillary molars distally within the confines of the dental arch. Appliances like the pendulum and distal jet have long been staples in orthodontic practice due to their ability to generate consistent distalizing forces. The pendulum appliance, introduced as an intraoral alternative to headgear, relies on a spring system anchored to the premolars or anterior teeth, moving molars distally with minimal patient compliance. Similarly, the distal jet appliance uses a compressed spring mechanism anchored to a palatal framework, providing efficient molar movement without additional anchorage reinforcement (7). Both methods have shown efficacy in creating space for anterior alignment and resolving Class II molar relationships.
Advancements in skeletal anchorage systems have enhanced the precision and versatility of distalization techniques. Miniscrews and miniplates offer stable anchorage that is independent of dentition, allowing clinicians to generate unidirectional forces without compromising anterior anchorage. This approach is particularly advantageous in cases requiring extensive distalization or involving high anchorage demands. Miniscrews, when strategically placed in the buccal cortical bone or palatal region, provide a robust foundation for fixed mechanics. For example, the combination of miniscrews with sliding mechanics enables controlled distal molar movement while reducing tipping and unwanted reciprocal forces (8).
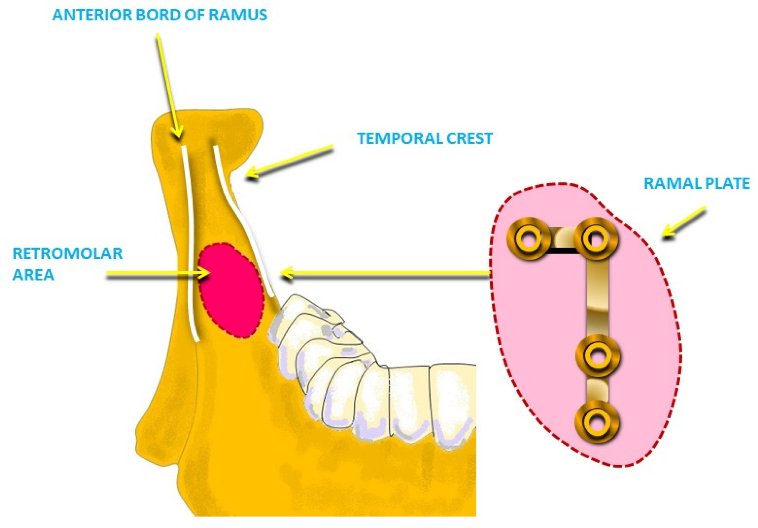
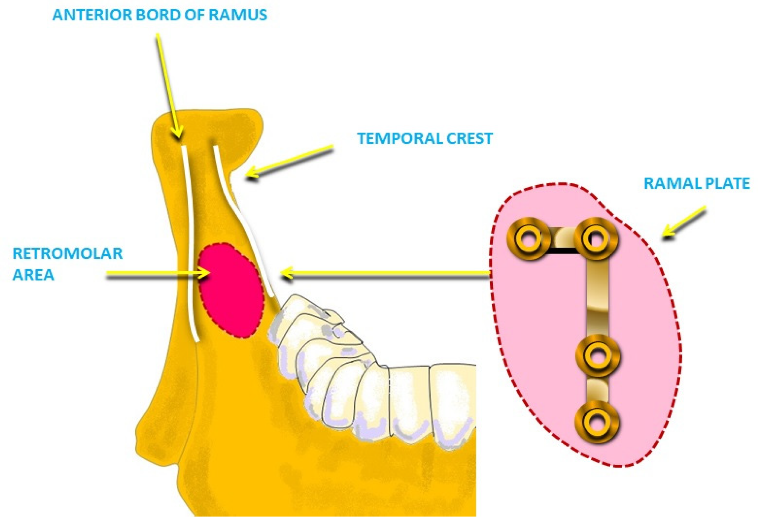
Mandibular distalization, while inherently more complex, has become increasingly feasible through the integration of skeletal anchorage and innovative appliance designs. The anatomical constraints of the mandible, including the dense cortical bone and proximity to the lingual nerve, present unique challenges to achieving distal movement. Techniques such as midline miniscrew anchorage have emerged to overcome these obstacles. By positioning a miniscrew in the symphyseal region and employing custom sliding mechanics, distalization of mandibular molars can be achieved with minimal side effects. Studies have reported successful distalization in adult patients, a demographic previously considered challenging for non-extraction approaches (9, 10). Furthermore, the lower arch distalization technique using Ramal plates (Figure 1) has been highlighted in several clinical studies emphasizing its benefits (11).
Digital technology has further refined these techniques, enabling more accurate diagnosis and treatment planning. Cone-beam computed tomography (CBCT) and three-dimensional (3D) imaging allow precise evaluation of anatomical structures, facilitating the design of customized appliances. Additionally, computer-aided design and manufacturing (CAD/CAM) have introduced aligners and fixed appliances tailored to individual patient needs. These advancements not only improve treatment efficiency but also enhance patient comfort and satisfaction. Biomechanical principles underpin the success of both molar and mandibular distalization. The application of optimal forces ensures efficient tooth movement while minimizing the risk of root resorption or periodontal damage. Controlled tipping or bodily movement of molars, as required by the treatment plan, is achieved through careful calibration of appliance design and activation. Furthermore, managing anchorage loss remains a critical consideration, with skeletal anchorage systems offering significant advantages over traditional methods in this regard (12, 13). The interplay between biological response and mechanical force application determines the outcome of distalization. While significant progress has been made in refining these techniques, individual variability in bone density, root morphology, and patient compliance necessitates a personalized approach to treatment planning. By integrating advanced appliances, innovative anchorage systems, and digital tools, orthodontists can effectively address the complexities of molar and mandibular distalization, opening new possibilities for non-extraction treatments.
Clinical Applications and Case Selection Criteria
The clinical application of molar and mandibular distalization extends beyond simple space creation, encompassing a wide range of malocclusion corrections and individualized treatment plans. Successful implementation requires careful assessment of case-specific factors, including malocclusion type, skeletal and dental relationships, and patient compliance. Molar distalization has become a cornerstone in addressing Class II malocclusions characterized by a discrepancy in the maxillary and mandibular dental arches. These cases often involve protrusive maxillary dentition or crowding in the anterior segment. Distalization allows the orthodontist to reposition maxillary molars without resorting to extractions, maintaining the integrity of the arch and minimizing potential adverse effects on facial aesthetics. Appliances like the pendulum or distal jet are frequently utilized in these cases, providing predictable outcomes when carefully planned. Selecting patients with favorable anchorage conditions, such as minimal need for skeletal correction, enhances the efficiency of these techniques (14).
Mandibular distalization, while traditionally more challenging, has become an essential tool in treating specific Class III malocclusions where mandibular dentition is anteriorly positioned relative to the maxilla. These cases demand precise skeletal anchorage to achieve posterior movement of the mandibular teeth without impacting the lower incisors. Miniscrew-anchored appliances have shown particular promise in addressing such malocclusions, especially in adult patients where skeletal growth modification is not viable. Proper patient selection involves evaluating mandibular anatomy, including bone density and cortical thickness, to ensure stability and predictability of distalizing forces (15, 16).
Case selection criteria also consider the degree of crowding present in the dental arches. Mild to moderate crowding is often managed effectively through distalization, while severe crowding may necessitate alternative approaches, such as extractions or arch expansion. For molar distalization, patients with adequate posterior space in the dental arch, as determined through cephalometric analysis and imaging, are ideal candidates. Similarly, mandibular distalization requires sufficient posterior clearance to accommodate molar movement. CBCT imaging is a valuable diagnostic tool in assessing posterior space availability and identifying anatomical limitations that might impede treatment (17, 18).
Patient compliance plays a significant role in determining the feasibility of distalization techniques. Non-compliance with extraoral appliances, such as headgear, has historically limited their effectiveness. However, modern intraoral and skeletal anchorage systems eliminate the dependency on patient cooperation, making distalization a viable option for individuals with variable compliance levels. For example, fixed miniscrew systems anchored in the palate or buccal region provide consistent and reliable forces, reducing the need for active patient involvement. This aspect makes distalization particularly suitable for adolescent and adult patients with limited motivation for appliance wear (19).
Incorporating patient-specific factors, such as skeletal maturity, is crucial for optimal treatment outcomes. Younger patients with ongoing growth potential are often ideal candidates for maxillary distalization, as their skeletal response can enhance the effectiveness of the procedure. In contrast, adult patients require more meticulous planning due to the reduced adaptability of their periodontal and skeletal structures. Advances in biomechanics, such as force modulation and custom appliance design, have improved the predictability of distalization in these populations, allowing for safe and effective treatment in non-growing patients.
Outcomes, Limitations, and Future Perspectives
The outcomes of molar and mandibular distalization have been widely studied, demonstrating significant potential in achieving orthodontic objectives without resorting to extractions. Clinical success depends on the effective management of both biomechanical challenges and patient-specific anatomical factors. Reports highlight the effectiveness of molar distalization in correcting Class II malocclusions, with significant improvements in molar and canine relationships, reduction in overjet, and anterior crowding alleviation. However, treatment success often relies on the ability to maintain the distalized position of the molars during and after treatment. Relapse remains a common concern, necessitating long-term retention protocols to ensure stability (20, 21).
Mandibular distalization, while historically limited by anatomical constraints, has shown encouraging outcomes with the advent of skeletal anchorage systems. Precise distal movement of mandibular molars, achieved without excessive tipping, has proven effective in addressing specific Class III cases and borderline extraction scenarios. The integration of miniscrew anchorage has reduced dependence on reciprocal forces, enhancing the predictability of outcomes. Yet, clinical variability in response to treatment, particularly in adult patients with denser cortical bone, underscores the need for careful case selection and customized biomechanical planning (11, 22).
Despite these promising results, limitations persist in both maxillary and mandibular distalization. The extent of achievable molar movement is inherently restricted by anatomical boundaries, such as the maxillary tuberosity and mandibular ramus. These limitations often necessitate compromises in treatment goals or alternative approaches, such as selective extractions or arch expansion. Moreover, undesired effects like molar tipping, loss of anchorage in the anterior region, or gingival recession can arise when biomechanical forces are not adequately controlled. Studies emphasize the importance of balancing force magnitude and direction to minimize such risks and optimize efficiency (23).
Technological advancements have significantly contributed to addressing these challenges. Digital tools, including three-dimensional imaging and treatment simulation software, have enabled more precise planning and execution of distalization protocols. The ability to visualize anatomical structures in three dimensions facilitates the accurate placement of miniscrews and determination of optimal force vectors. Furthermore, innovations in appliance design, such as the use of custom CAD/CAM aligners integrated with skeletal anchorage, have enhanced the precision of distalization while improving patient comfort and compliance. These developments suggest a shift towards a more individualized and technology-driven approach in future clinical practice (24, 25).
Future perspectives in the field focus on refining existing techniques and exploring novel approaches to overcome current limitations. Research into bioadaptive materials and force systems aims to optimize the biomechanical response of distalizing appliances, reducing unwanted side effects while improving efficiency. Additionally, the integration of artificial intelligence in treatment planning holds promise for further personalization of orthodontic care. Artificial intelligence-driven algorithms capable of predicting individual treatment outcomes based on patient-specific data could revolutionize the decision-making process, ensuring optimal results with minimal intervention.
Conclusion
Molar and mandibular distalization techniques offer effective, non-extraction solutions for managing malocclusions and space discrepancies, with significant advancements enhancing their precision and applicability. While challenges such as anatomical constraints and relapse persist, innovations in skeletal anchorage, digital tools, and customized appliances continue to improve outcomes. Long-term stability remains a critical consideration, requiring robust retention strategies. Ongoing research into biomechanics and technology integration promises to further optimize these techniques for individualized orthodontic care.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical consideration
Non applicable.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.