Volume 4, Issue 12
December 2024
Impact of Adherence to Treatment with Inhaled Corticosteroids/Long-Acting β-Agonists on Asthma Outcomes: A Systematic Review
Razan Ali Almalki, Anas Hassan Alzahrani
DOI: http://dx.doi.org/10.52533/JOHS.2024.41259
Keywords: asthma, outcome, impact, adherence, ICS/LABA
Background: The management of asthma primarily involves a continuous regimen of inhaled corticosteroids (ICS) combined with long-acting beta-agonists (LABA). Non-adherence can lead to poorly controlled asthma, resulting in more frequent exacerbations, increased emergency room visits, and higher hospitalization rates. By systematically reviewing existing studies on adherence, this review aims to aggregate and analyze data to elucidate how variations in adherence levels to ICS/LABA impact asthma outcomes.
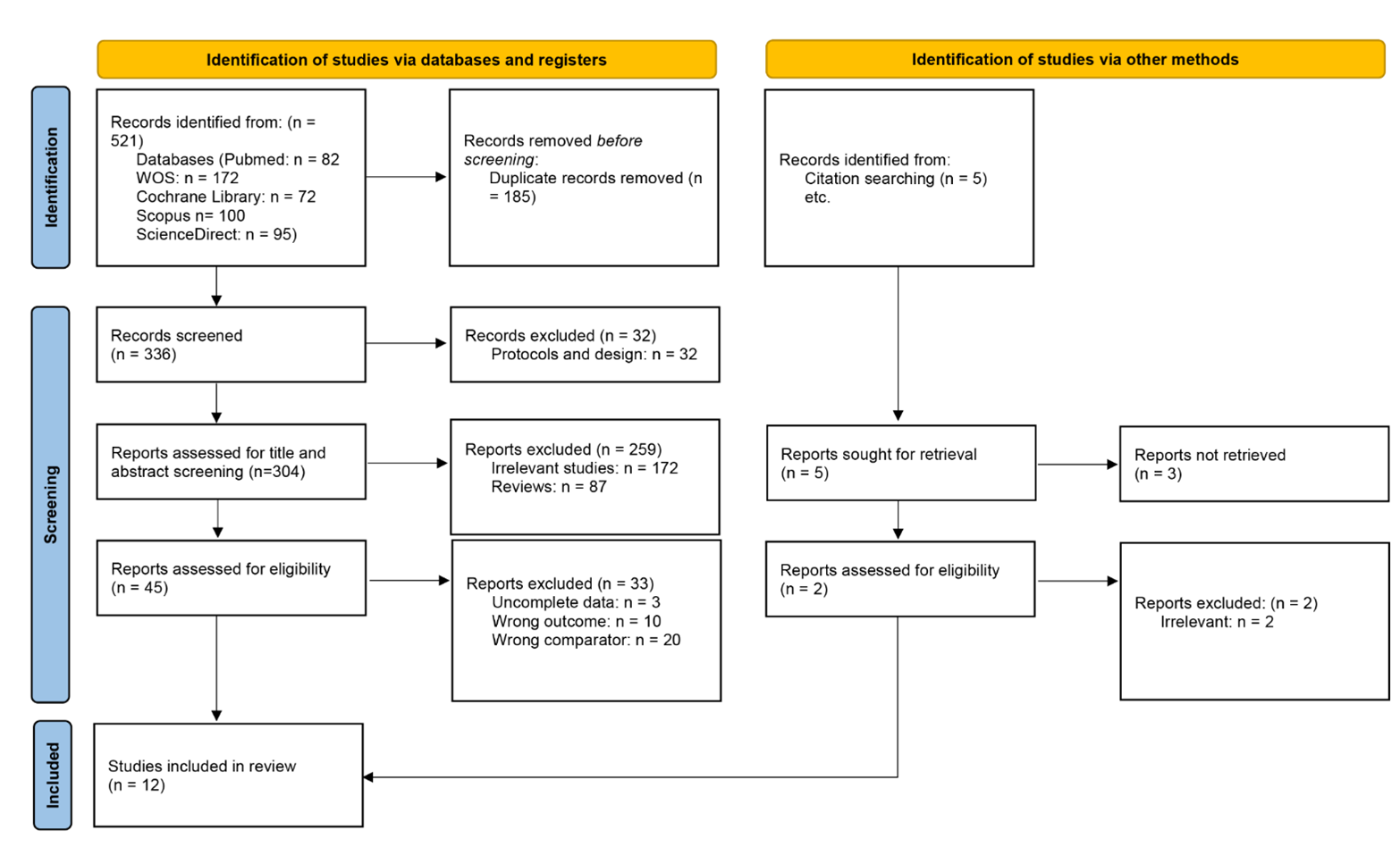
Methods: A comprehensive search was conducted across multiple electronic databases, including PubMed, Scopus, ScienceDirect, Cochrane Library, and Web of Science. Peer-reviewed studies on asthma treatments involving ICS and/or LABAs focusing on assessing how adherence to these medications impact several key outcomes for patients. Screening, data extraction, and quality assessment were performed independently by two reviewers, with discrepancies resolved through discussion.
Results: Findings from the included studies on asthma medication adherence reveal that higher adherence rates are linked to improved asthma management and reduced exacerbations. The adherence rates varied widely, with some studies reporting as high as 85% and others as low as 6%. Better adherence generally led to improved quality of life and fewer asthma-related exacerbations. Healthcare utilization costs also varied, with a range from $521 to $836. Barriers to adherence included fear of side effects and forgetfulness. Interventions such as enhanced education for both patients and providers, along with better medication management, particularly with combination inhalers, were suggested to improve adherence. Overall, consistent adherence to asthma medications is crucial for effective symptom control and reducing exacerbation rates.
Conclusion: Future research should focus on developing and testing interventions specifically designed to address adherence barriers, additionally, exploring the impact of different inhaler combinations on long-term adherence and asthma outcomes could provide further insights.
Introduction
Asthma is a widespread chronic inflammatory disease of the airways, characterized by airflow obstruction, increased airway responsiveness, and structural changes within the airways. It affects individuals across all age groups and regions. Despite various interventions, the Global Initiative for Asthma reports that asthma remains a significant public health concern, associated with premature mortality, impaired quality of life, and substantial economic burden (1). The prevalence of asthma among children in Saudi Arabia varies across different regions, with the highest rate observed in Alhofuf at 33.7% and the lowest in Abha at 9% (2). The prevalence of bronchial asthma in the southern region of Saudi Arabia was reported as 19.5% at sea level and 6.9% at higher altitudes. Additionally, the prevalence of lifetime wheeze was 25.3%, wheeze during the past 12 months was 18.5%, and physician-diagnosed asthma was 19.6% among male and female students aged 16-18 years in Riyadh (3). Asthma prevalence varies across continents, with rates ranging from 3.44% in Asia to 8.33% in Oceania (4). Specifically, Africa reports a prevalence of 3.67%, South America 4.90%, Europe 5.69%, and North America 8.29% (4). On a global scale, among individuals with asthma, 26.70% experience severe forms, 30.99% have eosinophilic asthma, while 48.95% suffer from allergic rhinitis, and between 7.0% and 25.40% have nasal polyps (4).
The aim of asthma treatment is to achieve optimal control with minimal risk of exacerbations, mortality, loss of lung function, and medication side effects. This goal can be reached through a combination of pharmacological and non-pharmacological interventions, including patient education, physical activity, smoking cessation, and rehabilitation. Pharmacological management primarily involves inhaled corticosteroids (ICS) and bronchodilators. For mild asthma, treatment should be administered as needed, using either a fixed combination of ICS and formoterol or short-acting bronchodilators. For moderate asthma, a continuous regimen of ICS combined with long-acting beta-agonists (LABA) is recommended, potentially with the addition of long-acting anticholinergics. Consideration should be given to allergen immunotherapy, or desensitization, if the asthma has a well-documented allergic component and remains under control. Asthma control should be regularly evaluated, and treatment adjustments should be made as necessary (5). Over the past thirty years, asthma management guidelines have advocated for a stepwise treatment approach, involving the use of controller medications, particularly ICS, along with on-demand rescue medications. Traditionally, short-acting β2-agonists were the standard for rescue therapy. However, recent evidence from Symbicort Maintenance and Reliever Therapy (SMART) has highlighted the benefits of using a combination of budesonide and formoterol; an ICS-LABA as both a maintenance and rescue treatment for moderate to severe asthma (6).
Combination therapy with ICS and LABA has been shown to provide superior control of asthma and chronic obstructive pulmonary disease, including a reduction in severe exacerbations. Clinical studies indicate that the combined use of these agents offers additive and potentially synergistic benefits. Preclinical research supports this, showing that ICS and LABA can have additive, compensatory, complementary, and synergistic effects on inflammation and airway and lung remodeling (7). These effects likely contribute to the enhanced efficacy observed in clinical settings when using ICS/LABA combinations for asthma and COPD. Furthermore, clinical data suggest that adjustable dosing with budesonide/formoterol may offer better asthma control compared to fixed dosing regimens (7). Irrespective of the severity of the underlying disease, individuals who suffer from asthma face exacerbations, which are characterized by amplification of existing inflammatory processes and a loss of disease control. Asthma exacerbations are a major cause of disease morbidity, increased health-care costs, and, in certain instances, lead to a more rapid loss of lung function. Adequate ICS treatment or combination ICS/LABA can minimize the frequency of exacerbations but may not completely avert them. Since asthma exacerbations can occur despite conventional therapeutic regimens, identifying at-risk individuals and developing a management strategy can enhance disease control and patient well-being (8).
Furthermore, despite the availability of effective treatments like ICSs, many individuals still struggle with inadequate asthma control. A major contributor to this issue is poor adherence to prescribed treatments, which is linked to increased rates of asthma exacerbations, hospitalizations, and fatalities. Research indicates that adherence to ICSs typically ranges from 30% to 70%, and improving adherence has been identified as a critical goal for both healthcare providers and patients to enhance asthma management (9). In the United Kingdom, the National Review of Asthma Deaths highlighted that a significant portion of asthma-related deaths could have been prevented, with inadequate medication use due to poor adherence being a key, preventable factor (10).
The World Health Organization defines adherence as the extent to which a person's actions such as taking medication, following a diet, or making lifestyle changes aligned with the recommendations given by a healthcare provider. Non-adherence can occur either intentionally or unintentionally. Intentional non-adherence happens when patients purposefully skip or alter their medication doses to meet their own preferences, which may include avoiding medication or missing medical appointments. Unintentional non-adherence, however, includes errors such as using an inhaler incorrectly or forgetting to take medication as prescribed (11). Medication non-adherence can significantly exacerbate health conditions and lead to higher healthcare expenses. Despite its importance, adherence to asthma medications remains relatively low, with rates around 30%–50% (12). Inadequate adherence to asthma medication is associated with several adverse clinical outcomes, including suboptimal asthma control, increased frequency of exacerbations, more frequent emergency department visits and hospitalizations, persistent eosinophilic inflammation, and a higher usage of oral corticosteroids (13).
Evidence from research indicates that almost a limited percentage of individuals consistently use their preventer ICS/LABA medication as prescribed. Many patients tend to use their treatment primarily when experiencing symptoms and then discontinue or reduce their use once they feel better. Some may stop using their medication if they perceive it to be ineffective. Clinicians should be vigilant and focus on ensuring that patients adhere to their ICS/LABA therapy, particularly if the anticipated improvements in disease management are not achieved. Suspected poor adherence should be treated as a significant clinical concern and warrants thorough investigation. It is particularly important to consider poor adherence in patients with asthma or chronic obstructive pulmonary disease who exhibit frequent use of reliever medications and experience recurrent exacerbations (14).
ICS and LABAs are pivotal in managing asthma by controlling inflammation and preventing bronchoconstriction, but their benefits are only fully realized when patients use them consistently and as directed. By systematically reviewing existing studies on adherence, this review aims to aggregate and analyze data to elucidate how variations in adherence levels impact asthma outcomes. This evidence can then inform strategies to improve adherence, such as patient education, simplified medication regimens, and interventions to address barriers to consistent use. Ultimately, enhancing adherence can lead to better asthma control, fewer complications, and more efficient use of healthcare resources, thereby improving patient outcomes and reducing the overall burden of asthma.
Material and methods
The systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Definition of outcomes and inclusion criteria
This systematic review included peer-reviewed studies on asthma treatments involving ICS and/or LABAs focusing on assessing how adherence to these medications impact several key outcomes for patients. The included studies evaluated how well ICS and/or LABAs control asthma symptoms, and whether they reduce the frequency of asthma exacerbations. Additionally, studies were included if they assessed the effect of these treatments on patients' overall quality of life, healthcare utilization, barriers to adherence and interventions to improve adherence. To ensure relevance and timeliness, only studies published between 2008 and 2024 were considered. Studies defining other respiratory disorders were excluded moreover studies were excluded if they were case reports, letters to the editor, opinion pieces, or non-peer-reviewed articles, as these sources did not provide the rigorous evidence needed for this review.
Search Strategy
We conducted a comprehensive search across electronic databases, including PubMed, ScienceDirect, Scopus, Web of Science, and Cochrane Library for publication. The search utilized a combination of specific keywords and phrases to ensure a comprehensive and targeted retrieval of relevant studies. The keywords used include "asthma," "adherence," "inhaled corticosteroids," "ICS," "long-acting β2-agonists," "LABAs," "treatment outcomes," "exacerbations," and "quality of life." Additional sources, such as reference lists of relevant articles and reviews, were also examined to identify any additional studies that met the inclusion criteria.
Screening and extraction
Articles with irrelevant titles were excluded from consideration. In the subsequent phase, both the full text and abstracts of the papers were meticulously reviewed to determine their compliance with the inclusion criteria. To streamline the process, titles and abstracts were organized, assessed, and scrutinized for any duplicate entries using reference management software (Endnote X8). To ensure the highest quality of selection, a dual screening approach was adopted, involving one screening for the evaluation of titles and abstracts, and another for the comprehensive examination of the entire texts. Once all relevant articles were identified, a structured extraction sheet was created to capture pertinent information aligned with our specific objectives. Two separate researchers conducted the data extraction process independently. The gathered information included various study attributes like the author's name, publication year, country of origin, study design, sample size, participants age and gender, adherence rates, symptom control, asthma exacerbations, healthcare costs.
Quality assessment
In our systematic review, we employed the Newcastle-Ottawa Scale (NOS) as a critical tool for assessing the quality of non-randomized studies included in our analysis. The NOS is widely recognized for its utility in evaluating the methodological quality and risk of bias in observational studies, including cohort and case-control studies. It provides a structured framework for evaluating key aspects of study design, including selection of study groups, comparability, and ascertainment of outcomes. By using the NOS, we were able to systematically appraise the included studies and ensure that only high-quality evidence contributed to our analysis, thereby enhancing the robustness and reliability of our findings. To evaluate the quality of randomized clinical trial Cochrane risk of bias tool.
Results
Search results
We executed the search methodologies outlined previously, resulting in the identification of a total of 521 citations, subsequently reduced to 336 following the removal of duplicates. Upon screening titles and abstracts, only 45 citations met the eligibility criteria for further consideration. Through full-text screening, this number was further refined to 12 articles aligning with our inclusion and exclusion criteria (15-26). Figure 1 provides an in-depth depiction of the search strategy and screening process.
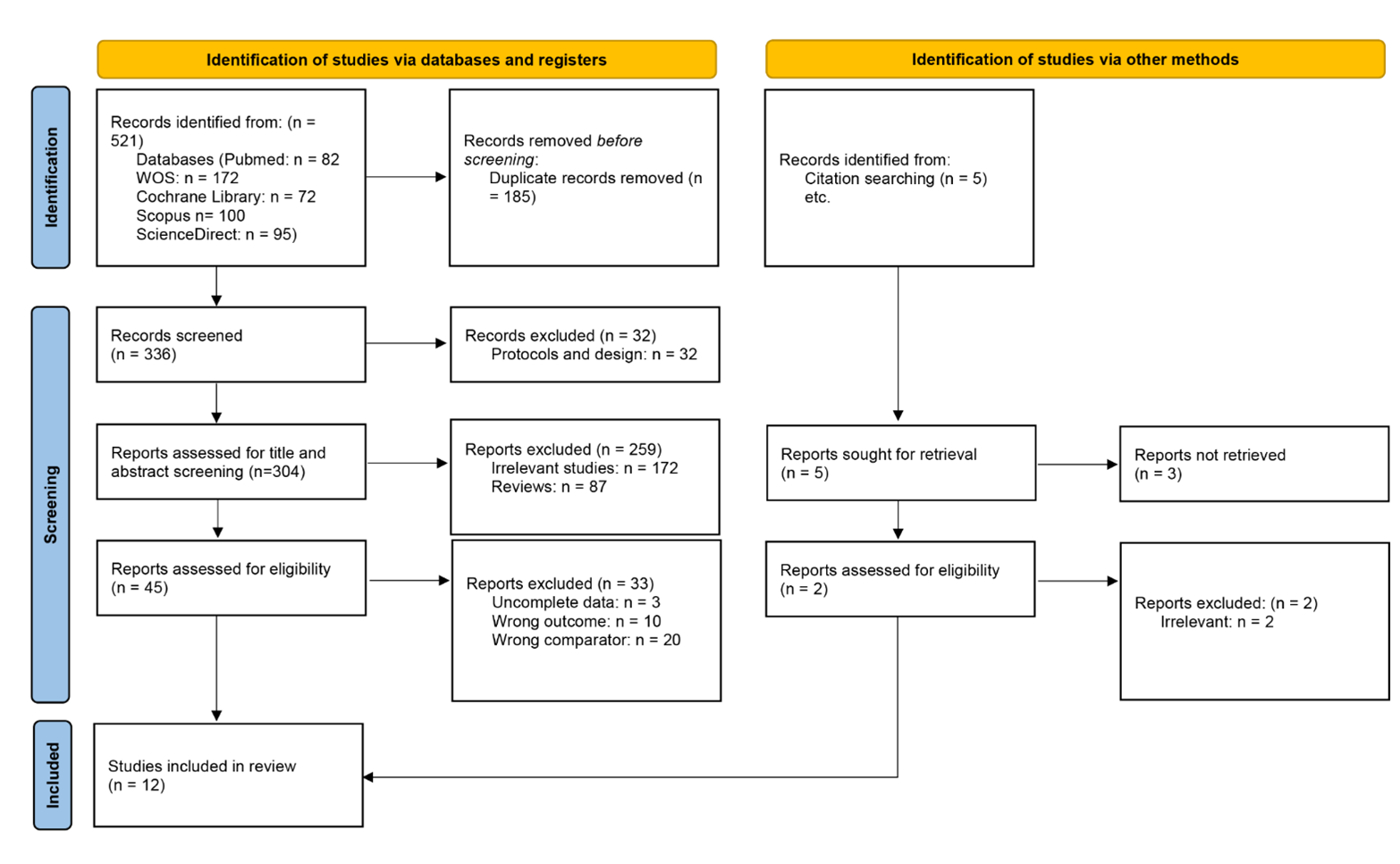
Figure 1: PRISMA flow chart
Results of Quality Assessment
The quality assessment of 11 included studies using the NOS reveals that most of the research is of high quality, with the majority scoring 9 out of 9. These scores reflect strong adherence to criteria such as cohort representativeness, control group selection, exposure ascertainment, and adequacy of follow-up. For one of the included randomized clinical trial analyses, from the Cochrane risk of bias, demonstrated good quality and low risk of bias. Overall, these results suggest that the studies included are generally robust (Table 1&2).
Characteristics of the included studies
This review encompassed 365550 participants with the mean age range of 10.5±3.6 to 49.2 ±11.2 and 42.87% of the study population comprised of males. Among the included studies, most of the studies were observational in nature except only one randomized control study. Regarding the geographical distribution of the studies, a majority were from United States of America, followed by three multicenter studies further followed by each from France, New Zealand, United Kingdom and Australia. The sample sizes varied among the included studies due to intrinsic characteristics of each study (Table 3).
Study outcome measures
Included studies evaluated rate of adherence and its impact on asthma symptom control and exacerbations. Additionally, quality of life, healthcare utilization cost, barriers and interventions to improve adherence were also assessed. The highest adherence rate of 85% was reported by Foster et al. however it’s noteworthy here that this is self-reported adherence while lowest adherence rate of 6% was observed by Lee Tac et al. (16, 17). Quality of life was assessed by two of the included studies and findings suggested that it improved with the therapy and adherence (17, 21). In terms of asthma exacerbations, Lee Tac et al. noted 18% of the study population experienced a total of 6705 asthma-related exacerbations while Foster et al. observed 10% reduction in severe exacerbations, Parimi et al. reported 11.07% and 11.01% rate of exacerbation respectively among fluticasone furoate / vilanterol versus budesonide / formoterol and fluticasone furoate / vilanterol versus beclomethasone dipropionate / formoterol groups (16, 17, 20). In a study by Bassam et al. 66.3% had a history of mild exacerbations (21). Moreover, one study by Averell reported an overall exacerbation rate of 27.50% while another indicated 20.0% (23, 24). The healthcare utilization costs varied among studies and was reported in a range of $521 ± 61,809 to $836. Only one of the included studies assessed barriers and reported that fear of side effects of ICS and forgetfulness prevented them to adhere to medication (17).
|
Table 1: Summary of the results of bias assessment of the included studies using the modified Newcastle-Ottawa scale (NOS) for observational study |
|||||||||||
|
S. No |
Author |
Year |
Selection |
Comparability |
Outcome |
Total score (out of 9) |
|||||
|
Representativeness of exposed cohort (Maximum: *) |
Selection of nonexposed cohort (Maximum: *) |
Ascertainment of the Exposure (Maximum: *) |
Outcome is not present at the start of study (Maximum: *) |
The Subjects in Different Outcomes Groups are Comparable (Maximum: **) |
Assessment of outcome (Maximum: *) |
Length of follow-up (Maximum: *) |
Adequacy of follow-up (Maximum: *) |
||||
|
1 |
Latry P, et al., (15) |
2008 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
2 |
Lee TAC, et al., (16) |
2010 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
3 |
Foster et al., (17) |
2012 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
4 |
Wu AC, et al., (18) |
2015 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
5 |
Feehan et al., (19) |
2015 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
6 |
Parimi et al., (20) |
2020 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
7 |
Bassam et al., (21) |
2021 |
* |
* |
* |
* |
** |
* |
* |
******** |
|
|
8 |
Averell CM, et al., (22) |
2021 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
9 |
Averell CML, F. et al., (23) |
2022 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
10 |
Averell CM, et al., (24) |
2022 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
11 |
Sousa-Pinto B, et al., (26) |
2023 |
* |
* |
* |
* |
** |
* |
* |
* |
********* |
|
Table 2: Cochrane Risk of Bias tool for RCTs |
|||||||
|
Study |
Random sequence generation |
Allocation concealment |
Blinding of participants and personnel |
Blinding of outcome assessment |
Incomplete outcome data |
Selective reporting |
Other bias |
|
Perrin K, et al., (25) |
low |
low |
low |
Low |
Low |
Low |
Low |
|
Table 3: Baseline characteristics of included studies |
|||||||
|
Author |
Country |
Year |
Study design |
Study period |
Total participants |
Total participants of Mean age(years) |
Gender (M/F) |
|
Latry P, et al., (15) |
France |
2008 |
Observational Cohort |
2003-2005 |
12502 |
32.0± 8.9 |
41.7%/58.3% |
|
Lee TAC, et al., (16) |
US |
2010 |
Observational |
2004-2009 |
28074 |
39.0 |
39%/61.0% |
|
Perrin K, et al., (25) |
New Zealand |
2010 |
Rct |
2007 |
111 |
49.2 ±11.2 /45.5 ±13.8 |
45.05%/54.95% |
|
Foster et al., (17) |
Australia |
2012 |
Prospective Cross Sectional |
NR |
99 |
47.6 ±15.8 |
42%/58% |
|
Wu AC, et al., (18) |
Multicenter |
2015 |
Retrospective Cohort |
2004-2010 |
69652 |
37 |
42%/58% |
|
Feehan et al., (19) |
US |
2015 |
Observational Cohort |
2012-2013 |
2193 |
NR |
46%/54% |
|
Parimi et al., (20) |
UK |
2020 |
Retrospective Cohort |
NR |
4217 |
48.3 ±18.4 |
40.15%/59.85% |
|
Bassam et al., (21) |
Multicenter (Algeria, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Qatar, Saudi Arabia, Tunisia, and the UAE) |
2021 |
Cross Sectional |
2014-2015 |
7203 |
45.4 ±14.7 |
42.8%/ 57.2% |
|
Averell CM, et al., (22) |
NR |
2021 |
Retrospective Cohort |
2014-2016 |
3973 |
NR |
NR |
|
Averell CML, F. et al., (23) |
US |
2022 |
Retrospective Observational |
2014-2019 |
50037 |
45.3 |
35.9%/64.1% |
|
Averell CM, et al., (24) |
US |
2022 |
Observational |
2012-2017 |
186868 |
10.5±3.6 |
59.6%/40.4% |
|
Sousa-Pinto B, et al., (26) |
Multicenter (27 countries) |
2023 |
Observational |
2015-2022 |
621 |
44.7 ± 16.5 |
38.2%/61.8% |
NR= Not Reported.
Latry et al. highlighted the necessity for enhanced education for both prescribers and patients regarding asthma control (15). Lee TAC et al. observed that while adherence and outcomes improved with leukotriene modifiers therapy, this came with higher pharmacy costs (16). Perrin K et al. found that using a combination ICS/LABA inhaler did not significantly boost adherence compared to using separate inhalers (25). On the other hand, Foster et al. demonstrated that better adherence notably improved symptom control (p=0.01) (17). Both Wu AC et al. and Feehan et al. reported generally poor adherence to controller medications (18, 19). Parimi et al. found that patients starting on FF/VI were less likely to discontinue treatment and showed higher adherence compared to those on BUD/FM or BDP/FM (20). Bassam et al. recommended improving treatment access, follow-up care, and education for healthcare providers and patients (21). Sousa-Pinto et al. reported that patients using ICS plus another LABA had better adherence than those using ICS plus F. Additionally, three separate studies by Averell et al. showed that patients starting FF/VI had better adherence and a lower risk of treatment discontinuation compared to those on B/F or FP/SAL (22-24). Overall, adherence to ICS/LABA medications is linked to fewer asthma-related exacerbations, highlighting the impact of medication adherence on asthma management. These results in detail are presented in (Table 4).
|
Table 4: Asthma control outcomes in relation to adherence levels to ICS/LABA of included studies |
||||||||
|
Study |
Adherence Measure |
Symptom Control (Asthma Control Tests, ACT Scores) |
Exacerbations (Frequency & Severity) |
Quality of Life (QOL) (Questionnaire Results) |
Healthcare Utilization (Costs, ER visits, Hospitalizations) |
Barriers to Adherence (Patient Factors, Treatment Factors) |
Interventions for Improving Adherence (Types, Results) |
Key Findings |
|
Latry P, et al., (15) |
≤44% adherence |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
There is a need for improved prescriber and patient education about asthma control |
|
Lee TA, et al., (16) |
6% adherence |
N/A |
18% of the study population experienced a total of 6705 asthma-related exacerbations |
N/A |
Overall: $836 (SD $998). |
N/A |
N/A |
Greater adherence and improved outcomes were observed with LM therapy, albeit with increased pharmacy costs. |
|
Perrin K, et al., (25) |
The mean (SD) percent adherence was 73.7% (36.0) for FP, 76.7% (30.5) for salmeterol, and 82.4% (24.5) for FP/salmeterol |
ACQ Single inhaler 1.3±0.7, combination inhaler 1.2±0.7 |
AEQ Score: Single inhaler (85.2%), combination inhaler (75.4%) |
N/A |
N/A |
N/A |
N/A |
Use of a combination ICS/LABA inhaler does not markedly increase adherence above that observed with separate inhaler use |
|
Foster et al., (17) |
Self-reported: 85% adherence |
ACT score: 19.9 ± 3.8 |
10% reduction in severe exacerbations |
SGRQ score: improvement by 4 points |
N/A |
Concerns about ICS side effects; forgetfulness |
SMS reminders improved adherence by 15% in 6 months |
Adherence significantly improved symptom control (p=0.01) |
|
Wu AC, et al., (18) |
ICSs: 86%; 82%, ICS/LABA; and 80%, LTRA |
N/A |
N/A |
N/A |
History of hospitalization: ICS:4%, ICS/LABA:9%, LTRA:4% History of ED visit; ICS:12%, ICS/LABA:13%, LTRA:11% |
N/A |
N/A |
Adherence to controller medications is poor |
|
Feehan et al., (19) |
14–16% of patients had ‘satisfactory’ adherence |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
Adherence was low |
|
Parimi et al., (20) |
Mean adherence was higher for FF/VI compared with BUD/FM (77.7 vs 72.4; p\0.0001), And BDP/FM(78.2vs71.0;p\0.0001) |
N/A |
Exacerbations Absence: Overall: 3750 (88.93%) (FF/VI): 842 (89.10%) (BUD/FM): 2908 (88.88%) Exacerbations Presence: Overall: 467 (11.07%) (FF/VI): 103 (10.90%) (BUD/FM): 364 (11.12%) |
N/A |
Hospitalization: FF/VI versus BUD/FM: 27,32%, FF/VI versus BDP/FM: 25.76% |
N/A |
N/A |
Patients who initiated FF/VI were less likely to discontinue treatment and showed greater treatment adherence versus patients who initiated BUD/FM or BDP/FM |
|
Bassam et al., (21) |
Good adherence was observed in 23.6% (p < 0.001). |
Completely controlled: 37.1% |
66.3% had a history of Mild exacerbations |
SF-8 Physical: 47.3 ±9.7 versus 44.7 ± 9.8, SF-8 Mental: 49.5 ± 9.6 versus 45.9 ±10.3 |
N/A |
N/A |
N/A |
Need to improve access to treatment, ensure better control follow-up and improved education among healthcare providers and patients. |
|
Averell CM, et al., (22) |
FF/VI vs B/F: 0.453±0.300 vs 0.345±0.252 and FF/VI vs FP/SAL: 0.446±0.300 vs 0.341 ± 0.257 |
N/A |
FF/VI vs B/F: 0.24±0.55 vs 0.24±0.55 and FF/VI vs FP/SAL: 0.22±0.53 vs 0.24 ± 0.52 |
N/A |
Total cost ($) FF/VI vs B/F: 940±4603 vs 953±5207 and FF/VI vs FP/SAL: 895±4621 vs 1024 ± 6252 |
N/A |
N/A |
Patients initiating FF/VI had better adherence and lower risk of discontinuing treatment versus B/F or FP/SAL |
|
Averell CML, F. et al., (23) |
30% adherence |
N/A |
Overall exacerbation 27.50 % |
N/A |
Total medical cost: $581 ± 4940, Hospitalization: 0.02 ± 0.13 |
N/A |
N/A |
Adherence to ICS/LABA medications is associated with reduced asthma-related exacerbations |
|
Averell CM, et al., (24) |
Twice-daily ICS vs Twice-daily ICS/LABA: PDC ≥0.5: 19.4% vs 26.7%, PDC ≥0.8: 4.3% vs 6.1% |
N/A |
Overall exacerbation 20.0 % |
N/A |
Inpatient visit: 2.2%, ED visit: 11.1%, Outpatient visit: 81.7%, Total cost: $521 ± 61,809 |
N/A |
N/A |
Low use of, and poor adherence to, ICS-containing medication, |
|
Sousa-Pinto B, et al., (26) |
Higher adherence was observed for ICS+LABA 75.1% vs ICS+F:59.3% |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
Users under ICS+other LABA displayed higher adherence than those under ICS+F |
LM: leukotriene modifiers; FP: fluticasone dipropionate; ACQ: Asthma Control Questionnaire; AEQ, Asthma Exacerbation Questionnaire; ICS = inhaled corticosteroid; LABA = long-acting β-agonist; LTRA = leukotriene antagonist; BDP: beclomethasone dipropionate; FM: formoterol. BUD: budesonide; FF: fluticasone furoate; VI: vilanterol; FP/SAL, fluticasone propionate; SAL: Salmeterol
Discussion
This review evaluated the incidence of adherence to asthma medications, specifically ICS and LABA, and assessed the impact of adherence to these medications. Findings from the included studies on asthma medication adherence reveal that higher adherence rates are linked to improved asthma management and reduced exacerbations. The adherence rates varied widely, with some studies reporting as high as 85% and others as low as 6%. Better adherence generally led to improved quality of life and fewer asthma-related exacerbations. Healthcare utilization costs also varied, with a range from $521 to $836. Barriers to adherence included fear of side effects and forgetfulness. Interventions such as enhanced education for both patients and providers, along with better medication management (particularly with combination inhalers), were suggested to improve adherence. Overall, consistent adherence to asthma medications is crucial for effective symptom control and reducing exacerbation rates.
Similarly, a random-effects meta-analysis of studies involving asthma patients aged 15-30 years who were prescribed ICS reported an overall adherence rate of 28% (95% CI: 20-38%, k=16) in studies providing quantitative adherence data. Adherence rates were notably higher in studies with a mean age under 18 years, reaching 36% (95% CI: 36-37%, k=4). Additionally, studies relying on self-reported adherence data reported higher adherence rates (35%; 95% CI: 28-42%, k=10) compared to those using pharmacy refill records (20%; 95% CI: 9-38%, k=6) (27). In this review, we also observed that self-reported adherence rates were the highest. Results of another meta-analysis indicated that in studies that defined nonadherence as obtaining 50% or less of the prescribed medication, the overall rate of nonadherence was 42.9%. For studies assessing nonadherence on a continuous scale, the weighted average nonadherence was also 42.9% (95% CI 28.2–49.5) (28). Meta-analysis of factors influencing adherence revealed that male patients had a higher likelihood of adherence, with an odds ratio of 2.25. Additionally, higher scores on the Asthma Quality of Life Questionnaire were associated with adherence, showing a mean difference of 0.47 points in adherent patients. Other factors, such as older age, greater knowledge about asthma, and simpler medication regimens, were also linked to better adherence, though these associations were derived from individual studies (28). However, it is noteworthy to mention here that although our incidence of adherence aligns well with these two meta-analyses, the predictors of adherence vary, which may be attributable to differences in intrinsic characteristics of the studies. For instance, differences in study population age, as the majority of our study population were middle-aged.
Furthermore, an analysis of 323 individuals revealed that 40.9% adhered to ICS. Good ICS adherence was associated with perception of asthma as a chronic disease (OR=1.22; 95% CI=1.10-1.35; p<0.001), belief of ICS as an essential medicine (2.67; 1.76-4.06; p<0.001), and fewer concerns about its use (0.39; 0.26-0.60; p<0.001). Patients on combined ICS-LABA medication exhibited a greater adherence rate (2.50; 1.41-4.44; p=0.02) than those on ICS alone (29). Findings from another observational study showed patients with poorly managed asthma had a lower proportion of excellent adherence (FDC ICS/LABA medication possession ratio [MPR] ≥0.8) compared to those with controlled asthma (35.6% [n = 21] vs 46.7% [n = 126]) (30). Additionally, findings from a multi-centre study concluded that treatment with a fixed-dose combination of budesonide/formoterol delivered via the Elpenhaler device was associated with improvements in asthma-related quality of life and lung function over 6 months, which were more pronounced in patients with higher adherence (31). Several studies have demonstrated that low adherence to controller medication is associated with an increase in the incidence of hospitalizations and emergency room visits (32). However, a database study by Vervloet et al. concluded that ICS adherence was not associated with exacerbations, whereas poor adherence (≤50%) has been linked to uncontrolled asthma (33). The most frequently recommended combination of medications to treat asthma, ICS-LABA, has been demonstrated to be the best option for preventing asthma exacerbation. Continuous use of asthma prescription drugs results in a consistent clinical outcome (34). All this evidence from the current literature supports the findings of this review and highlights the significance of adherence, which is associated with reduced exacerbations and improved quality of life, as reported by our results.
Previous research indicates that medication adherence rates among asthma patients typically range from 30% to 40% in real-world settings and can reach up to 70% in well-monitored clinical trials, though adherence often declines over time. Significant reductions in asthma exacerbations were only observed in patients who adhered to more than 75% of their prescribed medication. The challenges patients face in maintaining adherence are multifaceted, and interventions that are effective for one group may not yield the same results in different populations. Recent interventions aimed at improving adherence in asthma patients can be categorized into three main types: patient education programs, strategies to enhance communication between healthcare providers and patients, and the implementation of remote wireless technologies (35). A narrative review highlighted that personality traits, illness perceptions, and beliefs about treatment might play significant roles in predicting adherence (27).
A recent review highlighted that poor adherence is an independent predictor of future asthma exacerbations and persistent airflow limitation. A broad range of factors influence medication adherence, including multiple devices, a complicated treatment schedule i.e. several times per day, forgetfulness, cost, and concerns about adverse effects (36). Similarly, in this review we observed that one study reported fear of side effects and forgetfulness to be associated with medication non-adherence therefore, a study by Brooks et al. suggested that by embedding medication use into established daily activities can effectively address issues of forgetfulness as they noted that older asthma patients who stored their ICS in the bathroom or incorporated their use into a daily routine were more likely to adhere to their medication compared to those who employed different strategies (37). Additionally, Zhang et al. described that patient adherence to medication is heavily influenced by their understanding and beliefs about their condition and the prescribed treatments. This includes their assessment of the treatment’s necessity based on the severity of their illness and their concerns about potential medication side effects. Research indicates that patients who perceive a lower need for their medication or have limited confidence in its effectiveness are more likely to be non-adherent. Addressing these factors is crucial for improving adherence rates. Additionally, factors such as low health literacy, family dynamics, and cultural considerations have been shown to affect the use of asthma controller medications. Therefore, it is important to incorporate an individual's health literacy and cultural background into the development of educational programs and self-management strategies to ensure they are personalized and effective (38). Similarly, authors from the included studies in this review recommended to enhance medication adherence, interventions including comprehensive education for both patients and healthcare providers, along with improved medication management especially with combination inhalers.
Moreover, in this study we observed that one of the studies included reported that reminders through SMS helped in achieving 15% increase in adherence rate. Similarly, a systematic review from the present time concluded that electronic approaches have repeatedly demonstrated an effective impact on monitoring adherence to inhaled treatments in asthma patients. Adherence improvement was linked to minor clinical improvements and asthma-related quality of life. Digital health helps to monitor adherence in a way that is highly customizable, low cost, and conveniently accessible (39). Similarly, another systematic review supports this finding as results revealed that text-messaging interventions were beneficial for reducing forgetfulness by reminding patients to take their medications. Even though there is limited data from studies to support the usefulness of text message reminders, such technology is an important tool for achieving optimal medication adherence among asthmatics (40).
Pharmacological insights
A considerable amount of evidence from randomized controlled trials shows that adding LABA to an existing ICS regimen is more effective than simply increasing the ICS dose alone, even when accounting for variations in individual responses to asthma medications. LABA use as a standalone treatment for asthma is not recommended due to its lower efficacy compared to ICS and potential safety concerns. Consequently, combining ICS with LABA therapy remains the preferred approach for patients needing a step-up from ICS monotherapy (41).
ICS effectively manages chronic inflammation and reduces airway hyperreactivity in asthma, usually at low doses. LABAs contribute by targeting additional aspects of asthma's pathophysiology. Besides their primary function as bronchodilators, LABAs also help inhibit mast cell mediator release, decrease plasma leakage, and may reduce sensory nerve activation. Therefore, the combination of ICS and LABAs provides a broader therapeutic approach, addressing different facets of asthma that neither medication class can fully address on its own (42). Corticosteroids influence β2-receptor-mediated signaling and can up-regulate β2-receptor gene expression in response to glucocorticoids. Long-term use of LABAs can lead to β2-receptor down-regulation and tolerance to β-agonists; however, corticosteroids help mitigate this down-regulation and preserve receptor function during β-agonist therapy (41). Studies indicate that ICS/LABA combination inhalers are more effective than using separate inhalers for each medication. Additionally, combination inhalers tend to improve adherence to the treatment regimen in real-world settings (41).
This study boasts several notable strengths. It provides a comprehensive analysis by integrating evidence from high-quality, robust studies conducted across various geographical locations, which enhances the generalizability and reliability of its findings. The review employs a systematic search methodology to identify and include relevant studies, ensuring a comprehensive and unbiased collection of data. This evidence-based approach thoroughly examines how adherence to ICS/LABA therapy impacts asthma outcomes, identifying critical patterns that influence treatment effectiveness. The review’s insights are highly relevant to clinical practice, aiding healthcare professionals in optimizing treatment strategies and patient education. The review's strengths lie in its broad scope, practical implications, and the inclusion of diverse, high-quality evidence.
Limitations and future research directions
Despite these strengths this study has several limitations. One notable limitation is the inclusion of studies with varying participant populations, including one study that focused specifically on paediatric patients (24). Although this study had paediatric-specific limitations, it was included to ensure that no potentially valuable information was overlooked. Additionally, not all studies assessed barriers to adherence, and only one study provided detailed insights into these barriers. This lack of comprehensive assessment across studies reflects that the review may not fully capture all factors affecting adherence. These limitations suggest the need for further research with more consistent approaches and broader barrier assessments to provide a more complete understanding of adherence to ICS/LABA therapy. Despite these limitations, publishing this review remains important as it provides valuable insights and in-depth analysis of the existing literature in this regard.
Future research on the impact of adherence to ICS and LABAs on asthma outcomes should delve into several critical areas to enhance understanding and improve patient care. Longitudinal studies are essential to assess the long-term effects of adherence on asthma control and disease progression. These studies can reveal how consistent use of ICS/LABA therapy influences asthma outcomes over extended periods and help identify any delayed effects of adherence. Barrier assessment is another crucial area for research. Detailed investigations into the psychological, socioeconomic, and logistical barriers to medication adherence can provide a clearer picture of why patients may struggle with their treatment regimens. Understanding these barriers will facilitate the development of targeted interventions to address specific issues affecting adherence.
Additionally, age-specific research should be prioritized to address the unique challenges faced by different patient populations. For example, pediatric studies are needed to explore adherence issues in children with asthma, while research on adult populations can identify age-related factors influencing adherence. Tailoring interventions to these age-specific needs can improve outcomes across the lifespan. Adherence-enhancing interventions should be evaluated rigorously. This includes testing new digital health tools, such as mobile apps and reminders, and assessing the effectiveness of patient education programs, simplified medication regimens, and support systems. Identifying which interventions are most effective can guide the implementation of strategies that improve adherence.
Moreover, real-world evidence is necessary to understand how adherence impacts asthma management in everyday settings outside clinical trials. Research should focus on diverse patient populations and various healthcare contexts to gather insights on adherence patterns and their practical implications. Comparative effectiveness studies should investigate the benefits of different ICS/LABA combination therapies formulations. This research will help determine which formulations are most effective in enhancing adherence and managing asthma symptoms. Furthermore, personalized medicine approaches should be explored to tailor treatment plans based on individual patient characteristics, preferences, and responses. This can include customizing medication regimens and adherence strategies to better suit each patient, thereby improving adherence and overall asthma control. These research directions aim to address existing gaps in literature, provide a more comprehensive understanding of adherence dynamics, and ultimately lead to more effective treatment strategies and improved patient outcomes in asthma management.
Conclusion
This systematic review highlights the significant impact of adherence to ICS/LABAs on asthma outcomes. Findings emphasized that higher adherence rates are consistently associated with improved asthma management, reduced exacerbations, and improved quality of life. Future research should focus on developing and testing interventions specifically designed to address adherence barriers, such as personalized education programs and reminders. Additionally, exploring the impact of different inhaler combinations on long-term adherence and asthma outcomes could provide further insights.
Disclosures
Author Contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable.
Consent for publications
Not applicable.
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.