Volume 5, Issue 1
January 2025
Efficacy and Safety of Oral Semaglutide (Rybelsus) for Weight Reduction in Individuals with Obesity and Type 2 Diabetes: A Systematic Review
Azhar M. Al Ibrahem, Fatimah M. Al Ismail, Fatimah M. AlAbd, Huda I. Alsubaie, Zainab A. Al Ghazal, Fatimah A. Alkadi, Fatimah E. AlOmar, Alzahra A. Alahmed, Budur I. Al jasim, Aqilah R. Alkhalifah, Maryam A. Alsaleem, Fatimah M. Albrahim, Fatimah A. Alkhars
DOI: http://dx.doi.org/10.52533/JOHS.2025.50101
Keywords: Oral semaglutide, Obesity, Weight reduction, GLP-1 receptor agonist, Glycemic control
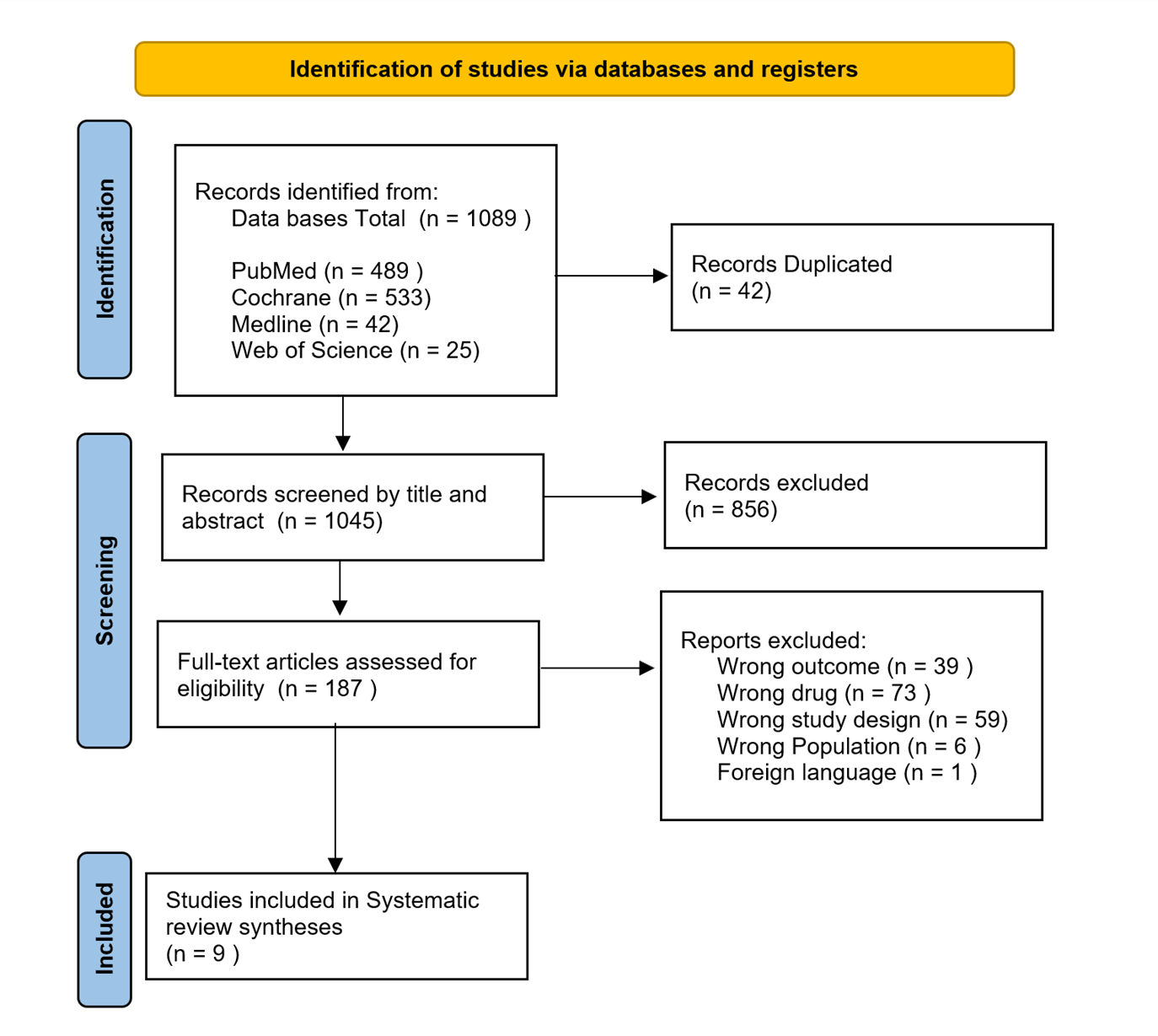
Obesity remains a significant global health issue, increasing the risk of chronic conditions such as diabetes, cardiovascular disease, and certain cancers. Despite the importance of lifestyle interventions, many individuals with obesity require pharmacological support for effective weight management. Oral semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has shown promise due to its ease of oral administration. This systematic review, registered with the International Prospective Register of Systematic Reviews (PROSPERO) and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, evaluated published randomized controlled trials (RCTs). A total of 9 RCTs, published between 2017 and 2020, were selected from an initial pool of 1,089 studies found through PubMed, the Cochrane Database of Systematic Reviews (Cochrane), Web of Science, and the Medical Literature Analysis and Retrieval System Online (MEDLINE). The findings indicate that oral semaglutide significantly reduces body weight, improves glycemic control, enhances satiety, and lowers energy intake compared to placebos and alternative treatments. However, long-term use was associated with a higher incidence of side effects. Overall, oral semaglutide is an effective treatment for obesity, providing significant weight loss and glycemic control. Its convenience as an oral option makes it favorable compared to injectable GLP-1 receptor agonists, though long-term use may warrant monitoring for cost and gastrointestinal side effects.
Introduction
Obesity is a global health issue, affecting millions worldwide and contributing significantly to the burden of chronic diseases, including Type 2 Diabetes Mellitus (T2DM) (1). According to the World Health Organization (WHO), over 1 billion individuals are affected by obesity, significantly increasing their risk of numerous serious health conditions (2–4). Obesity can be categorized into different classes. Class 1 (Body Mass Index (BMI) 30–34.9 kg/m²), Class 2 (BMI 35–39.9 kg/m²), and Class 3 or severe obesity (BMI ≥40 kg/m²) (5). Common polygenic obesity stems from the overconsumption of energy-dense, highly palatable foods and a sedentary lifestyle. These two environmental factors significantly contribute to a positive energy balance, leading to excess energy being stored as body fat. However, genetic predisposition plays a crucial role in how individuals respond to such an “obesogenic” environment. In certain individuals, this excess fat primarily accumulates in the intra-abdominal region and can extend to other visceral organs, increasing cardiometabolic risks. Importantly, adipose tissue is not merely a storage site for excess fat but functions as an active endocrine and paracrine organ. It releases various hormones, adipokines, and inflammatory cytokines that are integral to regulating energy balance, immune function, and inflammatory responses (5, 6).
Despite being largely preventable and treatable, excess weight and obesity require effective management strategies. Clinically significant weight loss is generally defined as a reduction of at least 5% of body weight from baseline over three months (7, 8). The Endocrine Society emphasizes the importance of incorporating diet, exercise, and behavioral modifications into all obesity management strategies (7). In addition to these foundational elements, weight loss medications and bariatric surgery may be utilized alongside behavioral changes to enhance food intake reduction and promote increased physical activity. For individuals with a BMI greater than 30 or those with a BMI between 27 and 30 who have at least one obesity-related complication—such as diabetes, hypertension, dyslipidemia, coronary artery disease, or stroke—pharmacotherapy should be considered in conjunction with lifestyle changes. For patients who struggle to achieve and sustain weight loss, prescription medications may be appropriate if they meet specific criteria outlined in the drug's label. It is recommended that if a patient successfully loses 5% or more of their body weight after three months of using a weight loss medication, they should continue the treatment (7). Conversely, if the medication proves ineffective or leads to adverse side effects, it is advisable to discontinue it and explore alternative options or strategies (9, 10).
Currently, the US Food and Drug Administration (FDA) has approved several anti-obesity medications (AOMs) for long-term use, which include lipase inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and drugs that act as neurotransmitter agonists, antagonists, or reuptake inhibitors. While GLP-1 receptor agonists are primarily recognized for their effectiveness in managing type 2 diabetes, they have also shown significant efficacy in treating obesity (11, 12).
GLP-1 receptor agonists are known to delay gastric emptying and increase feelings of fullness, contributing to weight loss. These agents also enhance insulin secretion and reduce glucagon release in response to glucose, making them effective for glycemic control in type 2 diabetes patients while minimizing the risk of hypoglycemia (13). Cardiovascular outcome studies have confirmed the safety of these agents, with certain GLP-1 receptor agonists, such as liraglutide and subcutaneous semaglutide, also providing cardiovascular and renal benefits. Liraglutide and dulaglutide also provide renal benefits by slowing the progression of albuminuria (14, 15). However, a major limitation of current GLP-1 receptor agonists is their requirement for subcutaneous injection (16–19).
Oral semaglutide, a newly approved GLP-1 receptor agonist available in pill form, provides a more convenient alternative to injectable versions and has proven effective for weight loss. Although oral semaglutide has a different absorption profile compared to its injectable counterpart, once absorbed, the pharmacokinetic and pharmacodynamic properties of the drug remain similar, regardless of the method of administration (20).
Although individual randomized controlled trials (RCTs) have assessed oral semaglutide's effectiveness in reducing body weight among obese individuals, to our knowledge, a comprehensive review of the evidence on oral semaglutide's effectiveness in reducing body weight among obese individuals is still lacking. This systematic review aims to fill the gap by evaluating the efficacy and safety of oral semaglutide for improve glycemic control and weight reduction in both diabetic and non-diabetic individuals, providing a clearer understanding of its role in obesity management across different patient populations.
Methodology
Study Design
This systematic review was conducted according to the PRISMA guidelines and registered in PROSPERO (Registration Number: CRD42024539868) (21, 22). A comprehensive literature search was executed in May 2024 across databases including PubMed, Cochrane Library, Web of Science, and MEDLINE. The search strategy employed Medical Subject Headings (MeSH) terms combined with relevant keywords "Obesity" OR "Overweight" AND "Semaglutide" OR "Rybelsus" AND "Weight Loss" OR "Body Mass Index" OR "BMI Reduction" OR "Weight Management" AND "Type 2 Diabetes Mellitus" OR "Non-Diabetic.", with no restrictions on publication dates.
Inclusion Criteria
The review included RCTs that evaluated the efficacy and safety of oral semaglutide for weight reduction in adults aged 18 and older. Studies had to administer oral semaglutide at any dose and duration, with comparators including placebo or other active weight management treatments. Outcomes had to include changes in body weight, BMI, waist circumference, adverse events, and discontinuations due to adverse events. Only full-text articles published in English were included.
Exclusion Criteria
Encompassed non-randomized studies, observational studies, reviews, case reports, animal studies, and trials with participants under 18 years of age. Studies focusing solely on other GLP-1 receptor agonists without evaluating oral semaglutide were also excluded, as well as articles not published in English, conference abstracts, and trials lacking relevant weight-related outcomes.
Study Selection
Records were imported into Mendeley for duplicate removal, followed by screening in Rayyan based on titles and abstracts. Two authors independently assessed the studies against inclusion and exclusion criteria, with full-text review for final inclusion decisions.
Data Extraction and Analysis
Data extraction involved study identification, publication year, country of origin, study design, sample size, follow-up duration, and criteria for inclusion/exclusion. Participant demographics, including age, sex distribution, medical history, and medication use, were documented. Intervention details included dosage of oral semaglutide and comparator treatments. Outcome measures recorded were pre- and post-intervention body weight, HbA1c levels, fasting blood sugar, and any reported adverse effects.
Quality and Bias Assessment
The risk of bias in the included studies was assessed using Cochrane's risk of bias tool for RCTs. Studies were excluded if they had a high risk of bias, based on criteria such as sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other potential sources of bias. The studies included were determined to have a low risk of bias.
Results
Study Selection
From an initial pool of 1,089 articles, 9 studies were identified as meeting the inclusion criteria after duplicates were eliminated and abstracts and full texts were evaluated, refer to (Figure 1). These studies, published between 2017 and 2020, comprised both diabetic and non-diabetic participants, and are summarized in (Table 1) (23–31).
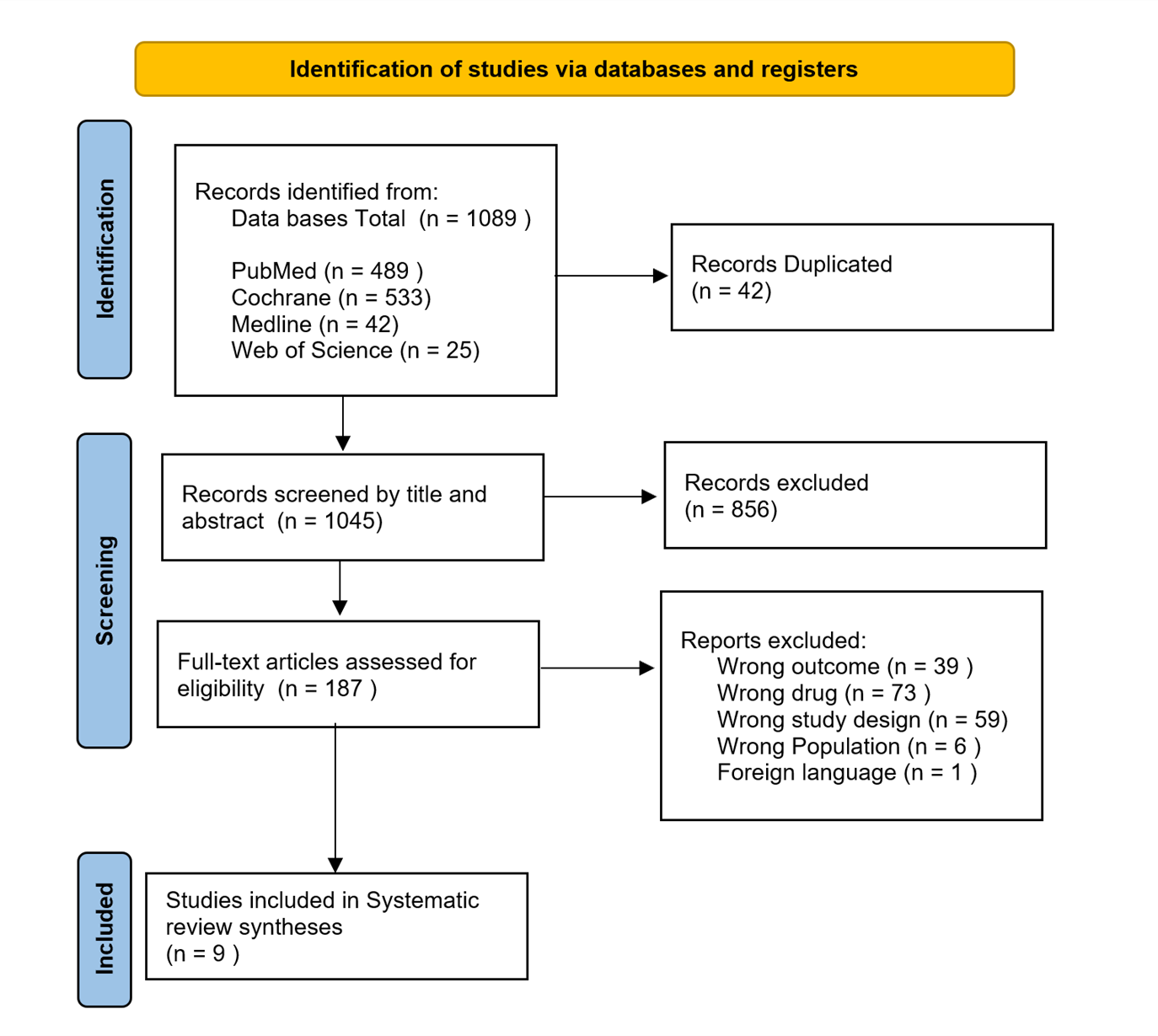
Figure 1: Flow Diagram of PRISMA
Quality Assessment Results
All selected studies were RCTs, reflecting robust methodologies that contribute to high-quality evidence. Nevertheless, a few studies lacked blinding, which could lead to potential biases in performance and detection. Despite these limitations, the overall quality of the studies was considered strong due to their consistent methodologies and dependable results, refer to (Figure 2, 3).
|
Table 1: Characteristics of Studies included in the Review |
||||||
|
Study ID |
Year of publication |
Intervention Drug (dose) |
Comparator (dose) |
Follow Up Period (Weeks) |
Change from baseline in Alc (%) (Oral Semaglutide 14 mg) Vs (Comparator) (Oral Semaglutide 14 mg) Vs (Comparator) |
Change from baseline in weight (KG) (Oral Semaglutide 14 mg) Vs (Comparator) (Oral Semaglutide 14 mg) Vs (Comparator) |
|
Davies, 2017 (27) |
2017 |
Oral semaglutide (3,7, or 14 mg od) |
Placebo |
26 - weeks |
(- 1.6%) Vs (- 0.3%) |
(- 6.9) Vs (-1.2) |
|
Pieber, 2019 (23) |
2019 |
Oral semaglutide (3,7, or 14 mg od) |
Sitagliptin 100 mg OD |
52 -weeks |
(- 1.4%) Vs (- 0.7%) |
(-2.9) Vs (- 0.8) |
|
Pratley, 2019 (24) |
2019 |
Oral semaglutide (3,7, 14 mg od) |
SC. Liraglutide 1.8 mg OD Placebo OD |
52 - weeks |
(- 1.2%) Vs (- 1.1 %) Vs (- 0.2 %) |
(- 4.4) Vs (- 3.1) Vs (- 1.2) |
|
Zinman, 2019 (25) |
2019 |
Oral semaglutide (3,7, or 14 mg od) |
Placebo |
52 - weeks |
(- 1.2%) Vs (- 0.1%) |
(- 3.3) Vs (- 0.4) |
|
Aroda, 2019 (26) |
2019 |
Oral semaglutide (3,7, or 14 mg od) |
Placebo |
26 - weeks |
(- 1.4%) Vs (- 0.6%) |
(- 2.6) Vs (- 0.2) |
|
Rosenstock, 2019 (28) |
2019 |
Oral semaglutide (3,7, or 14 mg od) |
Sitagliptin 100 mg OD |
78 - weeks |
(-1.4%) Vs (-0.8%) |
(-3.7) Vs (- 1.0) |
|
Rodbard, 2019 (31) |
2019 |
Oral semaglutide 14 mg OD |
Empagliflozin 25 mg OD |
52 - weeks |
(- 1.4%) Vs (- 0.9%) |
(- 4.2) Vs (- 3.8) |
|
Gibbons, 2020 (29) |
2020 |
Oral semaglutide (3,7, or 14 mg od) |
Placebo |
12 - weeks |
NA |
(- 2.7) Vs (- 0.1) |
|
Buse, 2020 (30) |
2020 |
Oral semaglutide (3, 7, or 14 mg OD) |
Sitagliptin 100 mg OD |
104 - weeks |
(- 1.5%) Vs (- 1.0%) |
(- 3.7) Vs (- 0.9) |
OD: Once Daily, SC: Subcutaneous
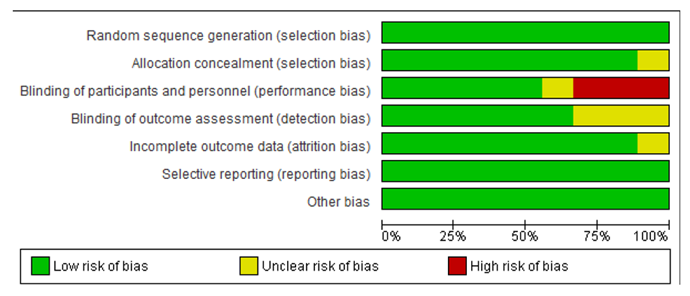
Figure 2: Results of the risk of bias analysis.
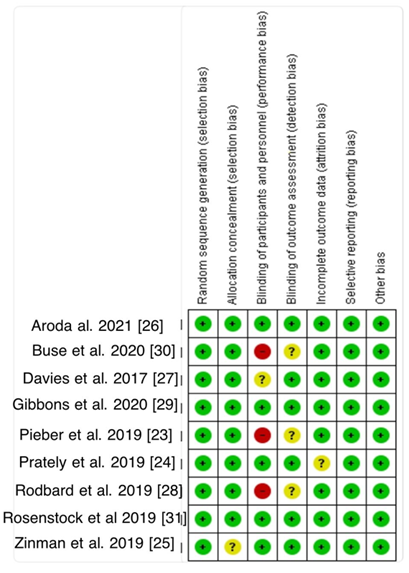
Figure 3: Summary of the risk of bias.
Main Clinical Findings of Included Articles
The efficacy of oral semaglutide was evaluated in a study by Pieber et al. (2019), where 253 participants received oral semaglutide and 251 were treated with sitagliptin. The doses of 3, 7, or 14 mg once daily demonstrated that oral semaglutide was more effective than sitagliptin in lowering both HbA1c levels and body weight over a 52-week period, including participants with T2DM and non-diabetic individuals (23).
In another study by Pratley et al. (2019), oral semaglutide, subcutaneous liraglutide, and placebo were compared among 285, 284, and 142 participants, respectively, over a duration of 52 weeks. Results indicated that oral semaglutide, across doses of 3, 7, or 14 mg daily, was as effective as liraglutide in reducing HbA1c and outperformed placebo in weight reduction. The safety profile was comparable to that of liraglutide, offering a viable option for those who prefer not to use injections (24).
Zinman et al. (2019) conducted research with groups of 184, 182, and 181 participants receiving doses of oral semaglutide (3, 7, or 14 mg) versus 184 participants on placebo. Notable, dose-dependent reductions in HbA1c and body weight were observed over 52 weeks, with over 54% of participants reaching an HbA1c level of ≤7.0% (53 mmol/mol) by week 52 (25).
Aroda et al. (2019) involved 525 participants on oral semaglutide and 178 on placebo over a duration of 26 weeks. The findings indicated that oral semaglutide, especially at the 14 mg dose, led to greater improvements in HbA1c and significant weight loss compared to placebo, with a safety profile in line with other GLP-1 receptor agonists (26).
Davies et al. (2017) investigated the effects of oral semaglutide (3 mg, 7 mg, or 14 mg once daily) in 559 participants, with 71 receiving a placebo. The study found that oral semaglutide resulted in better glycemic control compared to placebo over a 26-week period, demonstrating its effectiveness for long-term T2DM management, including in non-diabetic individuals. Body weight reductions were more pronounced with oral semaglutide (−2.1 kg to −6.9 kg) and subcutaneous semaglutide (−6.4 kg) compared to placebo (−1.2 kg). Significant weight loss was noted with oral semaglutide doses of 10 mg or higher (−0.9 kg to −5.7 kg; P < .001) (27).
Rosenstock et al. (2019) conducted a study involving 1,864 participants treated with oral semaglutide and 467 with sitagliptin, demonstrating that oral semaglutide at doses of 3, 7, or 14 mg daily achieved significantly greater HbA1c reductions compared to sitagliptin over 26 weeks. Notably, the 3 mg dose showed minimal benefits, suggesting the need for additional research. Furthermore, semaglutide at doses of 7 mg/day and 14 mg/day was associated with significantly greater weight reductions compared to sitagliptin, with weight differences of −1.6 kg (95% CI, −2.0 to −1.1 kg) and −2.5 kg (95% CI, −3.0 to −2.0 kg), respectively (P < .001). These findings highlight the superior efficacy of higher doses of semaglutide for glycemic control and weight loss (28).
In a short-term investigation by Gibbons et al. (2020), 13 participants received oral semaglutide in doses of 3 mg, 7 mg, or 14 mg once daily, while 14 were on placebo over a 12-week period. Results showed that oral semaglutide led to reduced energy intake, decreased body fat mass, and improved satiety after a fat-rich breakfast (29).
Buse et al. (2020) studied 253 participants on oral semaglutide over the first 104 weeks, with 100 participants continuing from weeks 52 to 104, and 98 participants on sitagliptin. The long-term use of oral semaglutide resulted in sustained improvements in glycemic control and continued weight loss. Transitioning from sitagliptin to oral semaglutide maintained HbA1c reductions, requiring fewer treatment intensifications but was associated with an increase in gastrointestinal events (30).
Rodbard et al. (2019) compared 411 participants on oral semaglutide with 410 on empagliflozin. The findings indicated that oral semaglutide, particularly at the 14 mg dose, was superior to empagliflozin in lowering HbA1c levels. Although body weight reduction was similar at 26 weeks, significant benefits of oral semaglutide emerged by week 52, with a safety profile consistent with other GLP-1 receptor agonists (31).
Overall, the findings of this review confirm that oral semaglutide (Rybelsus) is effective for improving glycemic control and reducing body weight in obese individuals, both with and without T2DM. Across the reviewed studies, oral semaglutide consistently achieved superior outcomes compared to various control groups or placebos, enhancing satiety and reducing energy intake. While effective, long-term administration of oral semaglutide was linked to a higher incidence of gastrointestinal adverse events.
Discussion
Obesity is a complex health issue that presents significant challenges to healthcare systems worldwide. Although there are various medications available, many have notable side effects and restrictions that limit their use among specific patient groups. In this context, GLP-1 receptor agonists like oral semaglutide have emerged as promising options for promoting weight loss and improving blood sugar control, especially in individuals with T2DM (32, 33). This review aims to summarize the current evidence regarding the effectiveness of oral semaglutide, comparing it to other treatments and providing insights into its clinical applications.
The study by Pieber et al. is a key contribution to the literature, showing that patients taking oral semaglutide experienced an average weight loss of 8.3 kg and a decrease in HbA1c levels by 1.5% over 52 weeks. Importantly, higher doses of 7 mg and 14 mg led to more significant results. This finding contrasts with earlier studies on traditional weight-loss medications, which often reported less impressive weight loss outcomes. The results of this review are consistent with those of Rosenstock et al., who found that patients lost an average of 6.5 kg and experienced a 1.2% reduction in HbA1c over 26 weeks (23, 28, 34). However, the Rosenstock study noted that the 3 mg dose did not offer meaningful benefits, highlighting the need for optimal dosing—a theme echoed in our findings that stress the importance of individualized dosing for achieving the best results (28).
Buse et al. conducted a long-term study revealing that patients maintained an average weight loss of 9.3 kg and continued to show improvements in blood sugar levels for up to 104 weeks. This extended period highlights the potential for long-term use of oral semaglutide, which is a significant advantage over other weight-loss medications that often show reduced effectiveness over time. Unlike many existing studies that focus mainly on short-term outcomes, this study emphasizes the sustained benefits of oral semaglutide in both the short and long term, suggesting it may be a viable option for ongoing management of obesity and T2DM (30).
In a comparative study by Pratley et al., oral semaglutide was found to be equally effective as subcutaneous liraglutide, with average HbA1c reductions of 1.5% and significant weight loss of 6.4 kg. This finding confirms its effectiveness as an alternative treatment. Additionally, the safety profile of oral semaglutide was similar to that of liraglutide, making it a suitable choice for patients who prefer oral medication over injections. This comparison is essential, as liraglutide has been a standard treatment for obesity, and showing that oral semaglutide is equally effective increases its clinical significance (24, 35–37).
Rodbard et al. provided an important comparison between oral semaglutide and empagliflozin. They found that while both treatments resulted in similar weight loss (around 2.8 kg by the 26-week mark), oral semaglutide was more effective in lowering HbA1c levels by 1.1%. By the 52-week endpoint, patients on oral semaglutide lost an average of 6.5 kg, emphasizing its long-term effectiveness. This finding contrasts with previous literature where empagliflozin often showed slightly better results for blood sugar control, further establishing oral semaglutide's role in comprehensive obesity management (31, 38, 39).
Furthermore, studies by Zinman et al., Aroda et al., and Davies et al. consistently demonstrated that oral semaglutide led to significant improvements in both HbA1c and body weight compared to placebo. Notably, Zinman’s study reported that by week 52, over 50% of participants achieved an HbA1c of ≤7.0% (53 mmol/mol), supporting our findings that oral semaglutide is effective in managing T2DM (25-27, 40-42).
Beyond its role in weight loss and glycemic management, the potential cardiovascular advantages of oral semaglutide are noteworthy. GLP-1 receptor agonists have been linked to a reduction in cardiovascular risk factors, with ongoing research investigating their long-term impacts on cardiovascular outcomes among patients with obesity. Future studies should concentrate on these enduring cardiovascular benefits, as well as the sustainability of both weight loss and glycemic control across diverse populations (43-46).
In reviewing the adverse effects linked to oral semaglutide, gastrointestinal complications, emerged as the most commonly reported issues (28). While these side effects were generally classified as mild to moderate, they resulted in treatment discontinuation for some individuals. The gastrointestinal side effects may be connected to the mechanism of action of GLP-1 receptor agonists, which delay gastric emptying and influence appetite regulation. This underlines the critical need for patient education regarding potential adverse effects and emphasizes the importance of clinicians closely monitoring patients during the initial stages of treatment to effectively manage these reactions (30).
Despite these encouraging findings, our review acknowledges several limitations. Other comorbidities of obesity, such as hypertension, dyslipidemia, and cardiovascular diseases, were not discussed, which limits the comprehensiveness of our assessment. Many of the studies we analyzed primarily focused on T2DM populations, which may limit the generalizability of our results to non-diabetic individuals. Additionally, the fact that many trials were sponsored by pharmaceutical companies may introduce bias. The relatively short duration of several studies (26-52 weeks) also limits our understanding of the long-term safety and effectiveness of oral semaglutide.
Conclusion
Oral semaglutide is an effective treatment for obesity, significantly reducing weight and improving glycemic control. It outperforms alternatives like sitagliptin and empagliflozin, with results comparable to subcutaneous liraglutide. Its benefits extend to both diabetic and non-diabetic individuals, with effectiveness influenced by dosage, and additional advantages such as reduced calorie intake and improved satiety.
Disclosure
Statement
The authors have no conflicts of interest to declare.
Funding
There was no funding for this study.
Financial Support
None.
Ethical Considerations
Ethical approval was not required for this study due to its nature.
Data Availability
Data supporting the findings of this study are available from the corresponding author upon request.
Author Contributions
AM and FM led the development of the systematic review protocol, designed the data extraction sheet, and managed manuscript submission. FE, BI, FM, and AR were responsible for data extraction. FB and HA evaluated the risk of bias and contributed to the discussion section. ZA and MA assisted in writing the introduction. BI prepared the methods section and organized the references. AM, FK, and FM authored the results section. AR took the lead in drafting the conclusion. FA and AA helped with the abstract formulation. AM supervised the entire project. All authors reviewed the full texts of eligible studies, proofread, and contributed to the final manuscript.