Volume 5, Issue 7
July 2025
Comprehensive Dental Treatment of Pediatric Patient with Celiac Disease in Saudi Arabia. A Case Report.
Ahmed N. Alsharif, Emad A. Albadawi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50702
Keywords: Celiac disease, Gluten, Oral health, Molar-Incisor hypomineralization, Autoimmune disease
Background: Celiac disease (CD) is a chronic autoimmune disorder triggered by gluten, a protein in wheat, barley, rye, and to a lesser extent, oats. It causes damage to the small intestine and an immune response often marked by Immunoglobulin A (IgA) antibodies. CD is linked to multiple systemic conditions and presents with oral signs that may aid in early diagnosis.Common oral signs include molar-incisor hypomineralization, enamel hypoplasia, recurrent aphthous ulcers, and delayed tooth eruption.
Case Presentation: This report examines the oral health of a patient diagnosed with CD. The patient presented with severe molar-incisor hypomineralization, generalized moderate plaque-induced gingivitis, and multiple carious lesions. Caries and periodontal risk assessments both indicated high risk. Additionally, her height and weight were below the 5th percentile for her age. The patient also had growth hormone and vitamin D3 deficiencies. Diagnosis was confirmed via biopsy and serological testing. She is currently receiving growth hormone (0.5 mg daily), vitamin D3 supplementation, and is on a strict gluten-free diet. Following these interventions and adherence to the diet, visible improvements in her overall health were noted.
Conclusion: CD is a multifaceted disorder requiring ongoing research for improved management. Dentists play a critical role in identifying oral signs such as molar-incisor hypomineralization (MIH) and enamel hypoplasia, which may point to underlying CD or related conditions. Early recognition and timely referrals are essential in preventing complications and supporting comprehensive patient care.
Introduction
Celiac disease (CD) is an immune-mediated systemic disorder triggered by the ingestion of gluten and related prolamines in individuals with a genetic predisposition. Gluten is a protein found in wheat, barley, rye, and, to a lesser extent, oats, which, when consumed by susceptible individuals, triggers the immune response and causes tissue damage (1). The disease is characterized by a complex array of clinical manifestations, including varying degrees of small intestinal damage. It is commonly associated with the presence of specific antibodies, such as anti-tissue transglutaminase (tTG) and anti-endomysial antibodies (EMA), as well as the human leukocyte antigen (HLA)-DQ2 or HLA-DQ8 genotypes, which play a critical role in the disease’s pathogenesis. These genetic factors predispose individuals to an inappropriate immune response upon gluten consumption, leading to inflammation and damage in the small intestine. The primary mechanism involved in CD is related to an inappropriate adaptive immune response to gluten-derived peptides. Prolamines contain key epitopes that, when presented by HLA-DQ2 or HLA-DQ8 molecules, trigger a CD4+ T-lymphocyte response. In the pathogenesis of CD, the role of the intestinal epithelial barrier—which normally prevents the passage of large molecules like gliadin—is now well recognized.
In people with a genetic susceptibility to develop CD, gliadin interacts with the intestinal cells to trigger the disassembling of the inter-enterocyte tight junctions (TJs). The impairment of the tight junctions determines the up-regulation of zonulin, a peptide involved in tight junctions regulation and responsible for the increased gut permeability. Gliadin peptides pass through the epithelial barrier and activate T-lymphocytes located in the lamina propria. Activated CD4+ T-lymphocytes produce high levels of pro-inflammatory cytokines, inducing either a T-helper 1 pattern dominated by Interferon-gamma (IFN-γ), and a T-helper 2 pattern, which causes a clonal expansion of B-lymphocytes that subsequently differentiate in plasma-cells secreting anti-gliadin and anti-tissue-transglutaminase antibodies.
The clinical presentation of CD is highly variable and can range from gastrointestinal symptoms to extra-intestinal manifestations (2). It has been suggested that gastrointestinal infections, such as rotavirus, may increase the risk of developing CD. Therefore, the rotavirus vaccine may significantly reduce the risk of CD, particularly in infants who are introduced to gluten before 6 months of age (3). Dental enamel defects are among the most common oral manifestations of CD, especially in children, often presenting as symmetrical hypoplasia on incisors and molars. Enamel defects are found in a high proportion of children with CD, with some reports indicating rates as high as 73% (4), A strong association also exists between CD and enamel hypoplasia (5). In contrast, the association between enamel defects and CD in adults is less pronounced, indicating that such signs are more useful for early diagnosis in children. Recurrent aphthous stomatitis is also frequently observed, though findings on its prevalence vary between studies. Recurrent aphthous stomatitis appears more frequently in some individuals with CD compared to healthy controls, though findings on its statistical significance vary. Additional oral signs such as delayed tooth eruption, dry mouth, glossitis, and angular cheilitis are commonly reported and are often related to the nutritional deficiencies seen in untreated CD (6,7). To manage CD, the patient should adhere to a strict gluten free diet forever. The aim of this case report is to investigate the effects of CD on oral health and to highlight the important role of dentists in the early diagnosis of CD and related conditions.
Case Presentation
The patient had a history of CD diagnosed two years ago. She has no known drug allergies and no food allergies. Her vaccinations are complete and up to date. She was born full term via natural delivery and has had three hospitalizations to date. Her medical problems include general weakness, fatigue, growth hormone deficiency, short stature (height below the 5th percentile for her age), weight at the 5th percentile according to CDC 2000 growth charts (8), and vitamin D3 deficiency. She is currently taking growth hormone (0.5 mg daily) and vitamin D3, as shown in Table 1. On oral examination, the buccal and labial mucosa were within normal limits, except for a fistula associated with tooth #75. The gingiva showed generalized moderate marginal gingivitis induced by dental biofilm, with physiologic pigmentation (9). The Plaque Index, based on the Simplified Greene and Vermillion Index (10), was 12/6 = 2, indicating poor oral hygiene. The tongue, floor of the mouth, soft and hard palate, and oropharynx were all within normal limits. Dentition examination revealed early mixed dentition, multiple occlusal and proximal carious lesions, and according to the classification outlined in American Academy of Pediatric Dentistry, the patient has severe molar-incisor hypomineralization (MIH) (11), as outlined in Table 2. The treatment plan began with the behavior management phase, which included behavior classification and appropriate management strategies. According to the Frankl Behavior Rating Scale, the patient scored 2 (Negative), and her personality was described as fearful. Based on Wright’s classification, she was potentially cooperative but tense, with a short tolerance span of 10–15 minutes. Behavioral management techniques included Tell-Show-Do, positive reinforcement, and reward-based methods (12). The preventive phase followed and included oral hygiene instructions, oral prophylaxis, topical fluoride application, and dietary counseling. The restorative phase was performed under general anesthesia (as detailed in Figures 1–10). In the space management phase, a lower lingual holding arch space maintainer was constructed. Finally, in the recall and maintenance phase, the patient was scheduled for radiographs every 6 months and recall visits every 3 months due to her high caries risk. These visits are intended to evaluate restorations and crowns, monitor caries activity, assess growth and eruption of permanent teeth, perform oral prophylaxis and topical fluoride applications, and reinforce oral hygiene and dietary instructions. The procedure was completed successfully without any complications. The patient returned for follow-up appointments at 3 and 6 months, during which no abnormalities or signs of treatment failure were observed. Psychologically, the patient showed significant improvement, as all sources of pain and discomfort had been eliminated.
|
Table 1: This table presents the list of medical problems identified in the patient. |
|
Medical Findings |
|
|
Table 2: This table presents the list of dental problems identified in the patient. |
|
Dental Findings |
|

Figure 1: Pre-Operative Records – This figure presents the clinical documentation and diagnostic images collected prior to the initiation of treatment. These records typically include intraoral and serving as a baseline for planning and evaluating treatment outcomes.
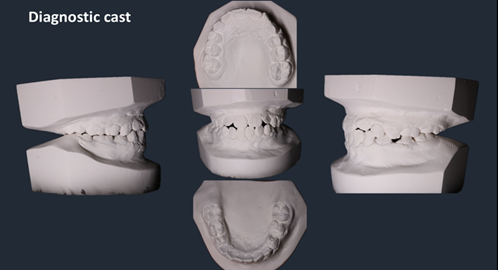
Figure 2: Diagnostic Cast. Moyer’s Mixed Dentition Space Analysis reveals mild crowding in both arches—2.2 mm in the lower arch and 2.4 mm in the upper arch.
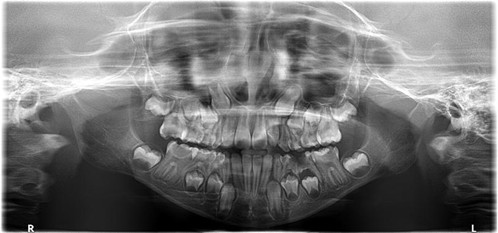
Figure 3: OPG. According to AAPD Guidelines For Prescribing Dental Radiographs for a new patient being evaluated for dental diseases and dental development and the child is in mixed dentition. Individualized radiographic exam consisting of panoramic x-ray and posterior bitewings (BW) and/or selected periapical (PA) images. The patient has straight nasal septum and normal nasal passages, her maxillary sinuses are intact, right & left condyles are symmetrical, the inferior border of the mandible is intact, the bone trabeculations are normal and her dental age is approximately similar to her chronological age. She has a normal complete count of dentition with no supernumerary teeth. No pathologies nor abnormalities were detected.
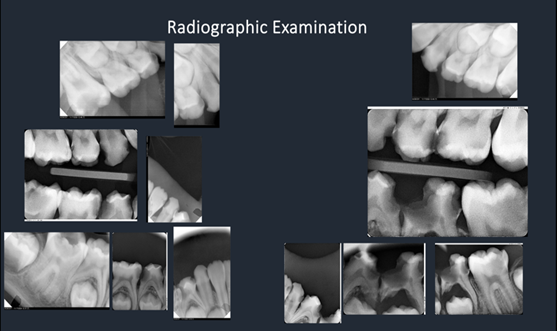
Figure 4: BWs and Selected Pas according to AAPD Guidelines For Prescribing Dental Radiographs for a new patient being evaluated for dental diseases and dental development and the child is in mixed dentition. Individualized radiographic exam consisting of panoramic x-ray and posterior bitewings (BW) and/or selected periapical (PA) images.
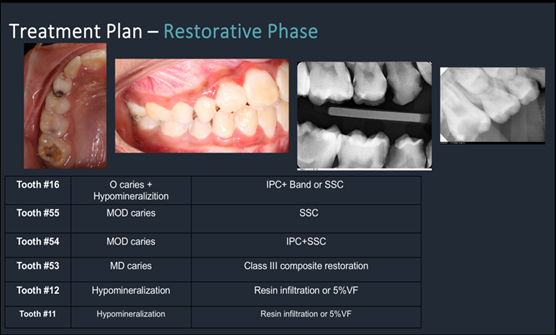
Figure 5: Treatment Plan – This figure shows the restorative procedures completed in Quadrant 5, including the management of severely affected teeth diagnosed with MIH.
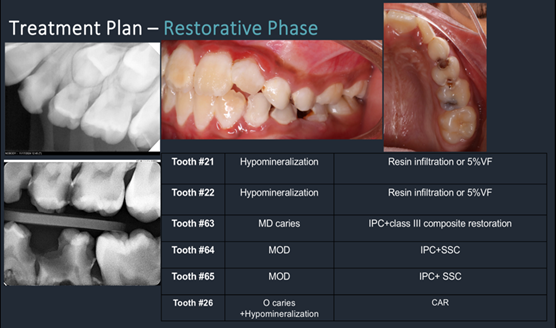
Figure 6: Treatment Plan – This figure shows the restorative procedures completed in Quadrant 6, including the management of severely affected teeth diagnosed with MIH.
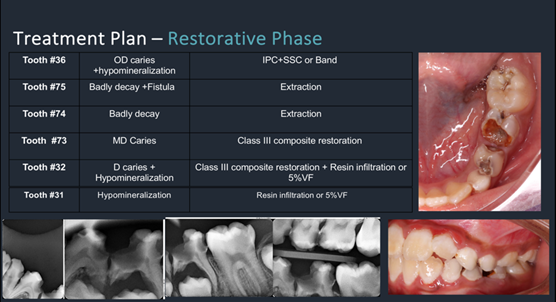
Figure 7: Treatment Plan – This figure shows the restorative procedures completed in Quadrant 7, including the management of severely affected teeth diagnosed with MIH.
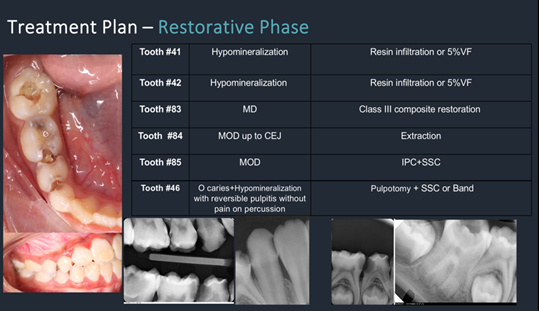
Figure 8: Treatment Plan – This figure shows the restorative procedures completed in Quadrant 8, including the management of severely affected teeth diagnosed with MIH.

Figure 9: Immediate Post-Operative Records – Intraoral photographs showing the clinical outcome shortly after completion of treatment.
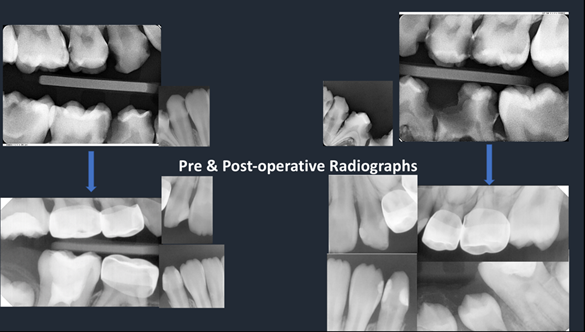
Figure 10: Pre and Post-Operative Records – Radiographs comparing the dental condition before and after treatment.

Figure 11: Pre- and Post-Operative Records – Intraoral photographs from lateral and frontal views comparing the clinical condition before and after treatment.
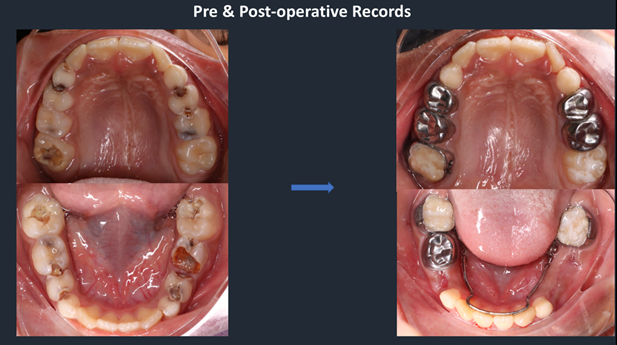
Figure 12: Pre- and Post-Operative Records – Intraoral photographs from occlusal view comparing the clinical condition before and after treatment.
Discussion
The seroprevalence of CD worldwide is 1.4%, while the biopsy-proven prevalence is 0.7%. The prevalence of CD varies based on geographical location and ethnic factors. The biopsy-proven prevalence of CD is 1.5 times higher in women than in men, and approximately twice as high in children compared to adults (13). In the Kingdom of Saudi Arabia, CD is relatively common, with a biopsy-proven prevalence of 1.4% and a seroprevalence of 2.7% in the general population (14) Gastrointestinal symptoms of CD are diarrhea, nausea, vomiting, abdominal pain, distension, weight loss, and constipation, may occur in older children, depending on the amount of gluten consumed (15). Extra-intestinal manifestations of CD include short stature, delayed puberty, anemia, osteopenia or osteoporosis, and elevated liver enzymes. Dermatologic features such as dermatitis herpetiformis and alopecia are also reported. Oral signs include dental enamel defects and recurrent aphthous stomatitis. Neurological symptoms may present as peripheral neuropathy, epilepsy, ataxia, and headache. Musculoskeletal complaints such as arthritis and arthralgia are common. Reproductive disorders include infertility and amenorrhea. Psychiatric conditions such as anxiety and depression are frequently associated. In our patient, only short stature and dental enamel defects are observed among these extra-intestinal manifestations. CD, an autoimmune disorder, is driven by key factors including genetic susceptibility (human leukocyte antigen HLA-DQ2 and HLA-DQ8 genotypes), environmental triggers such as gluten intake, and the autoantigen tissue transglutaminase (tTG), all of which play a crucial role in its pathogenesis. In addition to these factors, the loss of intestinal barrier function, a gluten-induced proinflammatory innate immune response, an inappropriate adaptive immune response, and an imbalanced gut microbiome all appear to contribute to the development of CD autoimmunity. The risk of developing CD is higher in individuals with first- and second-degree relatives affected by CD, as well as in those with conditions such as Down syndrome, type 1 diabetes mellitus (DM), selective immunoglobulin A (IgA) deficiency, autoimmune thyroiditis, Turner syndrome, and Williams syndrome (16-21).
Dental enamel defects and aphthous ulcers are the most prevalent and extensively documented oral manifestations of CD. Various extra-intestinal manifestations have been documented in both children and adults with celiac disease. However, in this patient, only severe MIH is present. (11). For a more comprehensive overview, refer to a recent review by Pastore and colleagues (22). The patient has severe molar hypomineralization based on the criteria outlined in the American Academy of Pediatric Dentistry guidelines (AAPD 2025), which define the severe type as having rapid posteruptive breakdown, widespread caries, dental sensitivity, and esthetic concerns. The AAPD (2025) outlines various management strategies for severe molar hypomineralization based on the severity and extent of post-eruptive breakdown (PEB), presence of caries, level of tooth sensitivity, and patient compliance. As a short-term approach, intracoronal restorations reinforced with orthodontic bands were used on the permanent first molars to limit removal of tooth structure and support the weakened enamel. Bonding to dentin in composite restorations is not compromised in affected teeth; however, the altered enamel lacks a microretentive etch pattern. To enhance microadhesion to the weakened enamel, it is recommended to remove approximately 1.5 mm of enamel, place restoration margins in unaffected areas, and use adhesive stabilization with a dentin bonding agent. Beveling the margins to extend into sound enamel has also been suggested. Additionally, glass ionomer cement (GIC) may be used as a dentin replacement. Glass hybrid and reinforced composite restorations used in managing severe MIH have shown 24-month survival rates of 77% and 93%, respectively; however, their longevity decreases over time. The primary goals of molar hypomineralization are to prevent hypersensitivity, post-eruptive breakdown (PEB), and the development of dental caries, while also enhancing the esthetics of the affected teeth. The application of fluorides—such as toothpaste, mouthwash, varnish, and silver diamine fluoride (SDF)—along with remineralizing agents and resin infiltration, has proven effective in preserving structural integrity and preventing post-eruptive breakdown in mild cases. Additionally, SDF has shown efficacy in both prevention and pretreatment by helping to reduce sensitivity (11).
This case report provides a detailed and multidisciplinary evaluation of the oral health implications of CD, highlighting the important role dentists play in early diagnosis and management. The comprehensive assessment, including clinical, serological, and histological confirmation of CD, alongside a thorough dental examination, strengthens the reliability of the findings. Additionally, the report addresses related systemic conditions such as growth hormone and vitamin D3 deficiencies, offering a holistic view of the patient’s health. However, as a single case report, the findings cannot be generalized to the broader population. The absence of long-term follow-up limits insight into the sustained impact of the interventions and the progression of oral manifestations. Furthermore, the report lacks a control comparison, and potential confounding factors influencing oral health outcomes are not fully explored. Future studies with larger samples and longitudinal design are needed to validate and expand upon these observations.
Conclusion
CD is a complex and controversial disorder, requiring further research and clinical trials for better management. Many questions remain about its links to other conditions and the role of environmental factors in its development. Dentists should be aware of all oral manifestations that may indicate CD aiding early diagnosis through symptom inquiry and serologic tests. Early referral to specialists can prevent complications, and sometimes dentists may notice signs through a patient's smile.
Acknowledgments
The authors would like to acknowledge and thank Dr. Roaa Dmeati, supervisor at East Jeddah General Hospital, during general anesthesia. In addition, the authors would like to thank and acknowledge the Department of Pediatric Dentistry, North Jeddah Specialized Dental Center, Jeddah, Saudi Arabia.
Disclosure
Statement
All authors have declared that no financial support was received from any organization for the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Funding
All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Ethical consideration
Consent for treatment and open access publication was obtained or waived by all participants in this study.
Data availability
All the data is presented within the paper.
Author contribution
Ahmed N. Alsharif and Emad A. Albadawi contributed to conceptualizing and data drafting. Ahmed N. Alsharif was responsible for drafting the manuscript.
