Volume 5, Issue 7
July 2025
Postoperative Hypoparathyroidism Following Thyroidectomy: Risk Factors and Management Strategies
Meshari Turki Alturki, Ahlam Yahya Alyami, Faten Saeed Bin Milhah, Madhawi Fahad Alduosari, Ahmad Abdul Qader Alenezi, Amal Abdullah Albuqaisi, Omar Abdullah Alahmari, Mohammed Saeed Kadash
DOI: http://dx.doi.org/10.52533/JOHS.2025.50704
Keywords: hypoparathyroidism, parathyroid, thyroidectomy, thyroid, risk factors, management
Postoperative hypoparathyroidism is a common endocrine complication following thyroid surgery, particularly total thyroidectomy. This disorder arises from decreased calcium levels in the blood caused by insufficient parathyroid hormone induced by the parathyroid glands. That can subsequently lead to a wide spectrum of issues, including long-term health impacts, cardiovascular disorders, and muscular cramps. After surgery, several factors can raise the risk of hypoparathyroidism. Among this extent of the thyroidectomy, the inclusion of central neck dissection is performed, whether incidental damage or parathyroid thyroidectomy outcomes, and surgeon experience. A patient's age, gender, present thyroid condition, and variations in anatomical features can additionally exert a significant role. Preoperative blood tests assessing calcium and vitamin D levels as well as alterations in parathyroid hormone levels during the surgery facilitate identifying those who might be at elevated risk for hypoparathyroidism. Typically, direct damage or absence of blood supply to the parathyroid glands leads to this condition, thus upsetting the body's capacity to control calcium and phosphate. Immediate identification and management hypoparathyroidism demand intimate observation of symptoms and continuous blood tests to check hormone and calcium levels. Healthcare centers maintain stable calcium levels and assist in parathyroid gland recovery. This condition could be temporary by receiving long-term oral calcium and vitamin D supplements and calcium given IV. Patients typically respond effectively with immediate therapy. If this condition lasts, though, managing it becomes a long-term issue that might seriously jeopardize the patients' well-being. Therefore, it is rather essential to have a qualified surgeon, use careful techniques during operation, and closely check patients afterward. Investigating emergent surgical methods and potential regenerative therapies seeks to help reduce the potential of this complication and alleviate its effects.
Introduction
Thyroidectomy is an essential surgical intervention for both benign and malignant thyroid diseases, including differentiated thyroid carcinoma, Graves' disease, and multinodular goiter. Patient outcomes have been much improved by recent enhancements in surgical methods, anesthesia control, and perioperative care (1, 2). However, thyroidectomy presents a significant risk for complications; among them, postoperative hypoparathyroidism is the most common and clinically relevant one. This condition seriously reduces both long-term quality of life and instantaneous recovery. Postoperative hypoparathyroidism is defined as a decrease in parathyroid hormone (PTH) secretion by direct trauma, loss of blood supply, inadvertent removal, or ischemia of the parathyroid glands during thyroid surgery (3). Either acutely with symptoms including perioral numbness, muscle cramps, and neuromuscular excitability, or chronically with neuropsychiatric diseases, cataracts, and calcifications in the basal ganglia, it causes hypocalcemia. If parathyroid function recovers within six to twelve months after surgery, this disorder is defined as temporary; if hypoparathyroidism lasts longer, it is defined as permanent and necessitates lifetime supplementation and monitoring (4). Variations in expressed postoperative hypoparathyroidism rates mostly depend on the institution and surgical population. Although permanent hypoparathyroidism affects 1% to 25% of cases, temporary hypoparathyroidism affects 14% to 43% of all cases. Among the several factors affecting this variation are several definitions, surgical experience, the degree of thyroidectomy, intraoperative management of parathyroid tissue, and anatomical variations among patients (5). Moreover, generating differences in reported rates are changes in postoperative monitoring techniques and hypocalcemia diagnosis standards. The demand for surgical experience and institutional knowledge is emphasized by the fact that high-volume centers specialized in endocrine surgery consistently demonstrate reduced complication rates in comparison to low-volume centers (6).
Surgical hypoparathyroidism has clinical significance independent of its physiological impacts. Extended hospital stays, more demands for comprehensive monitoring, and continuous reliance on calcium and vitamin D supplements all add to the significant challenges experienced by patients (7). Chronic hypoparathyroidism is associated with impaired quality of life, renal calcifications, cardiovascular disease, and elevated susceptibility to infections (8). Moreover, the management of hypoparathyroidism necessitates constant healthcare resources, including frequent biochemical tests and multidisciplinary follow-up, raising healthcare expenses (9). The demand for effective perioperative management strategies and preventative policies is highlighted by the continuous nature and complexity of treatment for afflicted people (10).
Notwithstanding substantial advances in surgical techniques, postoperative hypoparathyroidism is still a common and clinically significant complication following thyroidectomy. Its frequency affects not only immediate postoperative healing but furthermore, notably long-term patient well-being and healthcare outcomes (11). Effective prevention of this complicated disorder depends on total awareness of risk factors. Understanding modifiable intraoperative and patient-related risk factors will assist in enhanced surgical planning, raise intraoperative awareness, and enhance perioperative counseling (12). Reducing morbidity associated with hypoparathyroidism and enhancing patient outcomes depends on the development and implementation of evidence-based therapeutic approaches. Emphasizing the identification of recognized and unusual risk factors as well as the evaluation of present therapy approaches, this review attempts to consolidate the present knowledge of postoperative hypoparathyroidism (13). This review article aims to create a structured framework for risk classification, early detection, effective treatment and guideline recommendations. Eventually, by increasing awareness and following best practices, postoperative hypoparathyroidism and related issues can be uncommon, so improving surgical results and long-term quality of life for patients having a thyroidectomy (14).
Methodology
A comprehensive literature search was conducted in PubMed, Science Direct, Web of Science, and Cochrane databases using Medical Subject Headings (MeSH) and relevant keywords. The search strategy included Boolean operators as follows: ("hypoparathyroidism" OR "parathyroid") AND ("thyroidectomy" OR "thyroid") AND ("risk factors" OR "management"). The search, including combinations of all related terms, was performed on April 28, 2025. All relevant peer-reviewed articles involving human subjects and those available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, or participant age.
Discussion
Risk factors for postoperative hypoparathyroidism
Postoperative risk factors reducing the incidence of postoperative hypoparathyroidism and improving surgical outcomes depend on an awareness of the risk factors associated with it. One can divide the risk factors into surgical factors, patient-related factors, and laboratory or histology predictors (15). In surgical contests, the risk of hypoparathyroidism is significantly impacted by the extent of thyroidectomy performed. Because of increased manipulation and possible compromise of parathyroid blood supply, a complete thyroidectomy consistently presents an elevated risk than a partial thyroidectomy. Often performed in cases of thyroid cancer, central neck dissection and lymphadenectomy significantly elevate the risk of unintentional parathyroid gland excision or devascularization (16). Predominant causes of postoperative hypocalcemia are unintentional parathyroidectomy, either by direct excision or ischemic damage. Furthermore, the surgeon and the volume of operations are subjects of concern; doctors with substantial caseloads and specialized endocrine surgery facilities routinely demonstrate decreased rates of postoperative hypoparathyroidism, thus emphasizing the demand for surgical accuracy and expertise (17). The factors impacting patients' risk vary depending on several patient-related variables. Age has been correlated; younger patients exhibit a somewhat elevated incidence, maybe related to increased aggressive disease manifestation (18). Although female patients exhibit significant sensitivity, gender-related variations have been observed; the fundamental causes of these differences remain unknown. Because of the related inflammatory milieu, fibrosis, and demand for enhanced surgical dissection, pre-existing thyroid disorders—especially Graves' disease and thyroid cancer—increase the risk of hypoparathyroidism (19). The complexity of preservation during surgical operations is much influenced by anatomical differences in the quantity, orientation, and vascularization of parathyroid glands (20). Histological and laboratory findings have indicated deficiency in calcium, vitamin D, and postoperative hypocalcaemia preoperatively, that associated with compromised parathyroid recovery (21). PTH kinetics intraoperative monitoring provides significant prognostic insights, considering the rapid decreases suggest an elevated risk of hypoparathyroidism. Outcomes following parathyroid autotransplantation vary; although this approach may preserve function, graft failure is a major concern (22).
Pathophysiology of postoperative hypoparathyroidism
The pathophysiology of postoperative hypoparathyroidism results from disturbance of the complex parathyroid gland functional integrity and vascular supply for parathyroid glands after thyroid surgery (23). Because of the glands' elevated metabolic demands and limited ischemia tolerance, preservation of parathyroid viability is essentially dependent on the maintenance of intact artery input and venous drainage. Parathyroid tissue loss or nonviable residual glands can follow from mechanical trauma during gland dissection, inadvertent excision, or thermal damage from energy equipment (24). However, the primary mechanism remains vascular compromise. Ischemia, infarction, and consequent hypoparathyroidism might be induced by even minor disturbance of the inferior thyroid artery branches supplying the parathyroid glands. Although the condition's transient character can be explained by partial vascular damage, which causes transitory hypofunction, complete devascularization typically leads to permanent glandular failure (5). In particular conditions, specifically in those with autoimmune thyroid disorders such as Graves' disease, immune-mediated pathways are involved. The inflammatory milieu defined by lymphocyte invasion and fibrosis makes it challenging to find and preserve the parathyroid glands. Moreover, inflammatory cytokines can directly interfere with parathyroid cell functioning, so aggravating surgical hypocalcemia even in cases of significant glandular damage (25). The parathyroid glands demonstrate a limited capacity for regeneration. The degree and length of vascular damage will determine the recovery following ischemic injury. The common occurrence of delayed parathyroid recovery is clarified by partial ischemia assisting in explaining a delayed return of function over weeks to months (26). On the other hand, total necrosis inhibits regeneration, thus causing permanent hypoparathyroidism. When devascularization is unavoidable, parathyroid auto transplantation provides a possibility for functional restoration; nevertheless, successful graft revascularization is not guaranteed, and outcomes depend on graft management and recipient site properties. Understanding the cellular and vascular causes of parathyroid damage directs both preventive surgical techniques and postoperative treatment strategies to maximize gland preservation and enhance long-term endocrine outcomes following thyroidectomy (27).
Diagnosis and monitoring of postoperative hypoparathyroidism
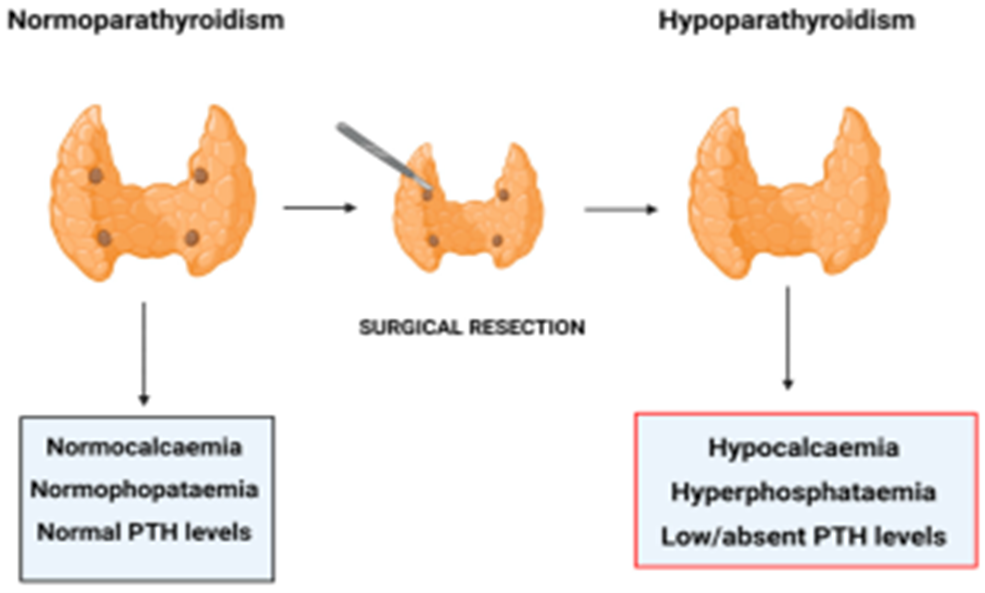
Accurate diagnosis and prompt monitoring of surgical hypoparathyroidism depend on early intervention, prevention of symptomatic hypocalcemia, and minimization of long-term impacts. The diagnosis depends on a synthesis of clinical symptoms, biochemical tests, and continuous PTH concentration monitoring (4). Patients could exhibit neuromuscular symptoms including perioral paresthesia, carpopedal spasms, muscle cramps, and in severe cases, tetany or seizures (2). A physical examination reveals Chvostek's and Trousseau's indications; however, they demonstrate reduced sensitivity and specificity (28). Thus, diagnosis depends on biochemical evaluation in great measure. For high-risk patients, serum calcium levels must be evaluated within the first 24 hours following surgery and tracked daily for a minimum of 48 to 72 hours (29). Hypocalcaemia is indicated by a blood calcium level either below 8.0mg/dL or ionized calcium below 1.1 mmol/L. However, depending just on calcium may delay diagnosis since hypocalcemia may not manifest immediately after surgery. A highly sensitive and timely indication of postoperative hypocalcemia is evaluating intact PTH levels soon following thyroidectomy. Consistently associated with a higher risk of hypoparathyroidism is a rapid drop in PTH levels (Figure 1) (30) following surgery or shortly thereafter. PTH values between 10 and 15 pg/mL within 1 to 6 hours postoperatively indicate a high risk of significant hypocalcemia that would necessitate supplementation (31). Monitoring calcium and PTH dynamics assists in distinguishing between transitory and progressive permanent hypoparathyroidism. Patients demonstrating modest PTH recovery in the first weeks typically reach hypocalcemia clearance, but regularly reduced PTH levels above six months point to irreversible glandular malfunction (32). Serum magnesium and phosphate are among the supplementary measures that have to be evaluated since concurrent electrolyte abnormalities could aggravate hypocalcemia. Standardized and comprehensive monitoring techniques assist in quickly identifying hypoparathyroidism, risk assessment, and management of this condition, thus enhancing postoperative outcomes and reducing morbidity connected with a delayed diagnosis (32).
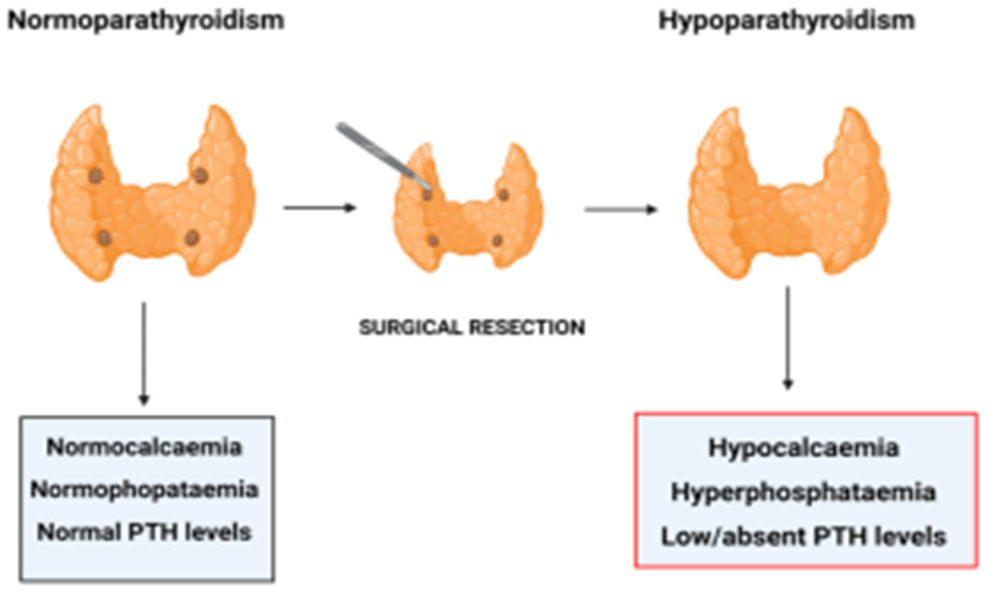
Figure 1: Post-surgical Hypoparathyroidism (30).
Management strategies for postoperative hypoparathyroidism
The therapy for postoperative hypoparathyroidism necessitates the quick management of hypocalcemia, the prevention of symptoms, and the facilitation of parathyroid recovery. Therapeutic approaches are tailored based on expected glandular impairment duration and degree of hypocalcemia. The immediate management of symptomatic cases or severe hypocalcemia necessitates an expedited response. The recommended intervention is intravenous calcium gluconate, delivered carefully to avoid cardiac arrhythmias (33). Magnesium repletion must be simultaneous since hypomagnesemia reduces parathyroid hormone (PTH) secretion and action. Particularly in cases of significant calcium boluses, patients must be carefully watched in a setting appropriate for cardiac monitoring (34). Once the patient becomes stabilized, he must start oral calcium supplements, typically using calcium carbonate or calcium citrate. Calcium absorption is enhanced by active vitamin D analogs including calcitriol and alfacalcidol, particularly in cases of low PTH activity. Sequential serum calcium tests guide dosage changes to maintain marginal calcium levels, thus reducing the risk of hypercalciuria and nephrocalcinosis. Extended Monitoring and Surveillance Over weeks to months, a gradual decrease in calcium and vitamin D supplementation is suspected in patients with temporary hypoparathyroidism as parathyroid function recovers (35). Permanent hypoparathyroidism is confirmed when hypoparathyroidism persists longer than six months. Long-term management necessitates constant observation of urine calcium excretion, serum calcium, phosphate, magnesium, and renal function (36). Novel treatments, including recombinant human PTH (rhPTH 1–84), are assessed for particular individuals with poorly controlled diseases or issues resulting from current treatment and provide physiological replacement alternatives. However, patients must carefully consider cost, availability, and possible long-term risks (Figure 2) (37). Enhancing outcomes and reducing the issues associated with chronic hypocalcemia and hypercalcemia depend on proactive patient education on symptom assessment and drug adherence (38).
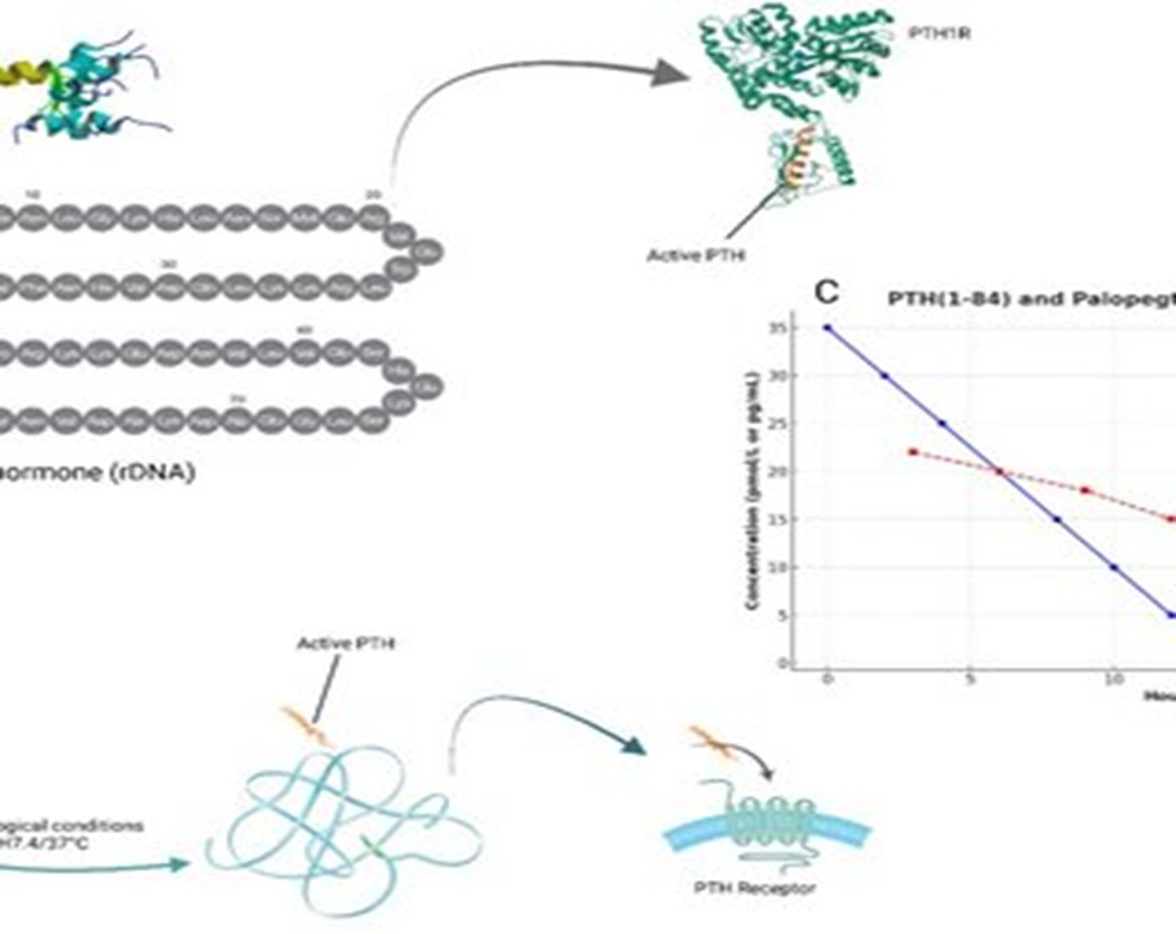
Figure 2: PTH Substitution Therapy for Chronic Hypoparathyroidism: PTH 1–84 and Palopegteriparatide (37).
Prognosis and outcomes of postoperative hypoparathyroidism
The degree of parathyroid damage, the quality of the surgical technique, and the success of initial therapeutic approaches will all impact the outcome of postoperative hypoparathyroidism. The predominant cases are temporary; parathyroid function typically returns in a few weeks to months following surgery (14). Most of the impacted individuals have transient hypoparathyroidism, which is marked by remission within six months. Early detection, strong calcium and vitamin D intake, and lessening of additional metabolic load on the parathyroid glands all necessitate rapid recovery. Based on sequential assessment of serum calcium and PTH levels, progressive reduction of supplements facilitates glandular recuperation and reduces overtreatment risks (35). Impacting a small population, permanent hypoparathyroidism is defined by persistent biochemical indicators of hypocalcemia and insufficiently reduced PTH levels for greater than six months. With estimates between 0.5% and 2%, depending on surgical skill and patient complexity, the incidence of lifelong hypoparathyroidism varies (39). People with chronic diseases demand constant supplements and exhibit possible risks including nephrolithiasis, nephrocalcinosis, basal ganglia calcifications, cataracts, and reduced quality of life. Enhanced functional outcomes in patients undergoing high-volume endocrine surgery highlight the demand for surgeon experience (40). Early postoperative PTH measurements reveal significant prognostic information since those with measured. However, reduced PTH levels had a higher chance of ultimate recovery than those with undetectable levels. Emergent medications, including recombinant human PTH replacement, provide patients with challenging diseases renewed hope since they enhance biochemical stability and reduce long-term renal impacts. However, financial considerations limit access even now. Early diagnosis, customized treatment, and careful long-term monitoring taken into consideration will assist in giving surgical hypoparathyroidism a positive outcome. Advancement of outcomes in this patient population depends on constant efforts to enhance surgical techniques and investigate creative treatment approaches (41).
Future directions
After thyroidectomy, postoperative hypoparathyroidism management appears increasingly promising and there are expected to be some interesting developments. A significant domain of advancement is intraoperative imaging and monitoring. Continually enhancing technologies include intraoperative PTH tests and near-infrared autofluorescence. These developments assist the surgeon in precisely identifying and protecting parathyroid glands, thus reducing the possibility of postoperative hypoparathyroidism (42). Moreover, continuous monitoring of calcium and PTH levels during surgery could provide rapid management, thus enhancing patient outcomes. Stem cell therapy and parathyroid regeneration present interesting fields of research. For those with lifetime hypoparathyroidism, parathyroid tissue engineering—especially with stem cells applied to repair damaged glands—provides great hope (43). Initial studies have indicated that stem cells could be utilized to generate functional parathyroid tissue, thus perhaps negating the demand for lifetime supplementation. Although continuous research may provide practical clinical applications immediately, this regenerative technique remains young and provides promising outcomes for effective treatments (44). Furthermore, the development of customized risk prediction models represents a significant advancement in the control of postoperative hypoparathyroidism. Risk assessment nowadays typically relies on surgeon experience and broad criteria; however, tailored models including genetic, clinical, and intraoperative data could significantly enhance outcomes (45). Personalized prediction systems driven by artificial intelligence and machine learning could assist doctors in precisely identifying those at high risk for hypoparathyroidism and modifying treatments. These models would enhance postoperative care and increase surgical planning accuracy, optimizing management and patient recovery. Driven by advances in intraoperative monitoring, regenerative therapies, and tailored risk assessment—which promise positive patient outcomes—managing surgical hypoparathyroidism is poised for revolution (46).
Conclusion
Postoperative hypoparathyroidism remains a key challenge after thyroidectomy. Risk factors include surgical technique, patient factors, and biochemical indicators. Early diagnosis using calcium and PTH levels supports prompt treatment. Individualized therapy helps manage symptoms and maintain renal and bone health. Temporary cases usually have good outcomes, but chronic cases show higher morbidity. Surgeon skill and careful postoperative care improve results. Future research may reduce incidence through biologics, surgical innovations, and regenerative approaches.
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Non-applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.