Volume 5, Issue 7
July 2025
Weight Management Strategies in Menopause: Hormonal and Lifestyle Considerations
Marwah Yaqoub Abdullah, Nojoud Majed Balubaid, Nehad Ali Alhazmi, Raghad Ali Alsufyani, Shahad Ali Alsufyani, Hanan Abdulrahman Alfayyadh, Amani Taher Barnawi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50708
Keywords: Menopause, Weight Gain, Weight Management, Lifestyle interventions, Hormonal Therapy
Menopause is the permanent cessation of menstruation that occurs due to a decline in ovarian hormone production. It is associated with lifestyle and hormonal changes that increase the risk of obesity, diabetes mellitus, and cardiovascular diseases. Weight gain is a common complaint by women during this period, and weight management is a significant challenge for them. Evidence on lifestyle interventions to manage weight addressing this specific population is lacking. Furthermore, the benefits of hormonal therapy in managing weight are controversial. The aim of this review is to discuss lifestyle and hormonal considerations in weight management during menopause. Menopausal hormonal changes alongside increasing age and decreased energy expenditure lead to an increase in women's total body weight, specifically an increase in abdominal subcutaneous and visceral adipose tissue deposition. Physical exercise showed significant improvements in metabolic functions, BMI, body weight, and body fat percentage in postmenopausal women. Furthermore, nutritional changes, such as introducing the Mediterranean diet, can have positive effects on weight management. Although evidence showed measurable positive effects of hormonal replacement therapy (HRT) on weight management, HRT is still not recommended in menopausal weight management strategies due to its high risks. Individualized, evidence-based strategies that consider hormonal, behavioral, and social factors are essential to support women through menopause transition.
Introduction
Menopause is diagnosed retrospectively after 12 months of permanent cessation of menstruation, which is caused by a decline in ovarian hormone production. In the United States, the current age of menopause ranges from 45 to 55 years, with a median of 52 years (1). Typically, women go through a progressive transition starting with the late reproductive years, then the perimenopause, ending with the final menstrual period and the early and late menopause. These stages are marked by vasomotor symptoms, menstrual irregularity, the genitourinary syndrome, and sleep disturbances (2).
Women at this period also experience lifestyle, hormonal, and age-related changes that lead to metabolic changes, increasing the risk of weight gain, diabetes mellitus, osteoporosis, hypertension, and cardiovascular diseases (2). Cardiovascular diseases are the leading cause of death in postmenopausal women (3). Menopausal hormonal changes, particularly estrogen deficiency, along with age-related changes, influence lipid metabolism, insulin resistance, and body fat composition. They also result in reduced physical activity and energy expenditure and an increase in the risk of depression (4). All of which can transform a woman's body from a gynecoid to an android body shape and increase abdominal and visceral fat accumulation (1, 5-7).
Weight gain and an increase in abdominal fat are commonly reported complaints by women at the menstrual transition period (5, 6, 8, 9). Research indicates that 20% of women gain ten pounds or more during this period (10), with an average annual weight gain of 1.5 pounds continuing until roughly two years after the final menstrual period, at which point weight changes tend to stabilize (11).
Weight management has always been a challenge for middle-aged women, even if they achieve a healthy weight (12, 13). Various weight management strategies in menopause have been introduced, including lifestyle interventions, cognitive and behavioral interventions, pharmacotherapy, hormonal therapy, and surgical interventions (4, 14-16).
Lifestyle interventions to manage weight mainly include exercise and healthy nutrition. However, the impact of lifestyle interventions, such as exercise and healthy nutrition, on weight gain, body composition, and body fat distribution during the menopause transition remains unclear. There is a lack of research specifically focused on women undergoing this pivotal menopausal transition. Furthermore, the role of hormonal therapy in weight management in menopause is controversial.
The aim of this review is to explore current evidence for lifestyle and hormonal considerations in weight management in menopause, highlighting the experience of menopausal women with different weight management strategies.
Methods
A comprehensive literature search was conducted in Medline (via PubMed), Scopus, and Web of Science databases up to May 15, 2025. Medical Subject Headings (MeSH) and relevant free-text keywords were used to identify synonyms. Boolean operators (AND, OR) were applied to combine search terms in alignment with guidance from the Cochrane Handbook for Systematic Reviews of Interventions. Key search terms included “menopause” OR “post menopause” OR AND “weight management” AND “lifestyle interventions” OR “lifestyle changes” AND “hormonal therapy” OR “hormonal changes.” Summaries and duplicates of the found studies were exported and removed by EndNoteX8. Any study that discusses lifestyle and hormonal considerations in weight management during menopause and published in peer-reviewed journals was included. All languages are included. Full-text articles, case series, and abstracts with the related topics are included. Case reports, comments, animal studies, and letters were excluded.
Discussion
Menopause Effect on Weight
Menopausal transition is a vital period of physiologic changes, which can last from 4 to 10 years, leading up to the final menstrual period. It is marked by irregular menstruation, fleeting symptoms such as depressive symptoms and hot flashes, and consistent alterations in bone density and lipid profile. It is also marked by accelerated loss and gradual depletion of ovarian follicles, resulting in reduced production of ovarian sex hormones and a compensatory rise in follicle-stimulating hormone (FSH) levels (16). The depletion of ovarian follicles results in a decrease in inhibin B, which is synthesized by the granulosa cells of antral follicles. This leads to a decrease in inhibition of pituitary FSH secretion; thus, FSH levels increase. Initially, elevated FSH leads to sustained or even heightened estradiol levels, but as the number of antral follicles significantly declines, estradiol levels eventually drop (2, 17-20).
It has been reported that these menopausal hormonal changes, alongside increasing age and decreased energy expenditure, lead to an increase in women's total body weight, specifically an increase in abdominal subcutaneous and visceral adipose tissue deposition (5). However, it has been hypothesized that postmenopausal weight gain is related to increasing age and decreased energy expenditure rather than hormonal changes (21, 22). Weight gain average varies, with 20% of women gaining 10 pounds or more during this period, but typically they gain an average of one pound per year during the period of menopausal transition (23).
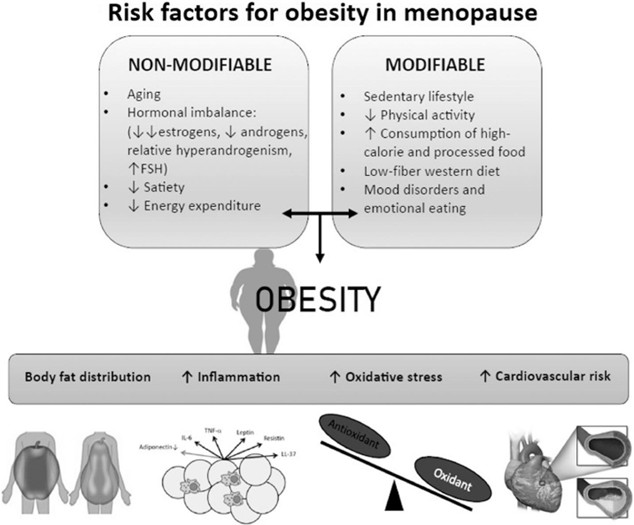
Before menopause, estrogens accumulate subcutaneous adipose tissue deposition in the femoral and gluteal regions. This distribution of adipose tissue has been associated with favorable cardiometabolic effects like decreased insulin resistance. On the other hand, androgens accumulate subcutaneous adipose tissue in a metabolically unfavorable region, which is the abdominal region (23). This central adiposity is linked to elevated risk of metabolic and cardiovascular diseases. It has also been associated with decreased physical activity and poorer quality of life (21). Risk factors of obesity in menopause are shown in Figure 1.
The increase in FSH level, decrease in circulating estradiol, and maintenance of androgen levels during menopause lead to relative hyperandrogenemia (24). Furthermore, the production of sex-hormone-binding globulin decreases during the menopause which also elevates the levels of bioavailable androgens (25). Thus, a change in women's body composition occurs, which is characterized by an accumulation of adipose tissue mainly in the abdominal area, referred to as an android fat distribution. An increase in total visceral adipose tissue also occurs (26).
These patterns of weight gain in postmenopausal women were found in multiple cohorts using waist-to-hip ratio, BMI, dual-energy X-ray absorptiometry, computed tomography, and magnetic resonance imaging measurements (6, 7, 20, 27, 28). Ethnic differences were also identified in the SWAN study (29). White and Black women both have shown similar trajectories in weight and visceral fat gains during the menstrual transition period; however, White women continued to gain visceral fat while Black women do not. On the other hand, Japanese women did not show the increase in visceral fat around the menstrual period but then demonstrated an increase in central adiposity after menopause (1).
Furthermore, it has been reported that the relationship between estrogens and central adiposity in postmenopausal women is bidirectional, since an increase in central adiposity can also result in increased levels of estrogens. This is due to the peripheral conversion of androgens in adipose tissue into estrogens (aromatization) (23).
After menopause, higher levels of estrogens in obese women have been observed when compared with nonobese women, though lower overall than premenopausal women (23). Notably, estrogens resulting from peripheral aromatization have been associated with unfavorable cardiometabolic effects (24, 26). This relationship also changes throughout the menopausal transition, with estradiol levels tending to be higher in the later stages of menopause compared to earlier stages (30). Besides all these physiological hormonal changes, postmenopausal weight gain can result from medications used to overcome the physical and hormonal changes of menopause in women, such as serotonin and norepinephrine reuptake inhibitors, antidepressants like selective serotonin reuptake inhibitors, and hormone treatments (31-33).
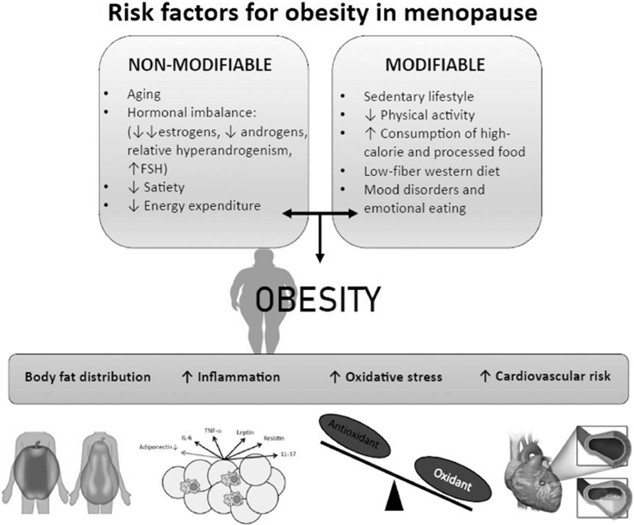
Figure 1: Risk factors of obesity in menopause (34).
Lifestyle Considerations
Lifestyle changes, including nutrition and physical activity, have been reported to be beneficial in health and prevention of chronic diseases. The lifestyle interventions focused on weight loss have been shown to reduce hot flushes in menopause (35-37). A 5-year randomized clinical trial evaluated the effects of a lifestyle changes intervention on the body composition of middle-aged premenopausal women. The intervention program included diet management, physical activity, cooking sessions, and motivational sessions to ensure adherence to the program. Following 4.5 years of the intervention, 55% of participants in the intervention group were at or below their baseline weight, compared to just 26% in the control group who maintained or lost weight. Furthermore, regular weight was associated with improvements in systolic blood pressure, LDL-C level, and triglyceride level. This study demonstrated that lifestyle changes may have positive effects on body composition during the menstrual transition period (38).
Physical Exercise
Regular physical exercise was found to be associated with less age-related declines in resting energy expenditure among postmenopausal women. It was also found that increased physical activity in both humans and rodents plays a key role in protecting against metabolic dysfunction after ovarian hormone loss. Thus, physical inactivity is considered a critical modifiable risk factor that may prevent or mitigate adverse metabolic changes during menopause (16, 20, 35). A systematic review and meta-analysis evaluated the effects of walking intervention studies on peri- and postmenopausal women. Intervention groups showed significant improvements in BMI, body weight, and body fat percentage compared with the control groups (37).
Nutrition
Nutrition is an essential component of any weight management plan. Typically, exercise with caloric restriction is recommended in weight management plans for peri- and postmenopausal women (39). Although caloric restriction proved effective in weight loss, no established universal approach for weight loss and metabolic health for this population is available. Tailored nutritional approaches should be developed for each individual and should account for food preferences, nutritional accessibility, and health history, among other factors (4). Hormonal changes should also be accounted for since the combination of an increase in FSH and a decrease in estrogen during the menopause transition enhances the breakdown of lean tissue, hence increasing protein needs (40).
Furthermore, the decline in estrogen levels leads to a decrease in insulin sensitivity, resulting in changes in carbohydrate metabolism during the menopause transition. In normal status, the dietary reference intake for carbohydrates is 130 g/day; however, this recommendation was not specifically developed with consideration for the hormonal and metabolic changes that occur during the menopause transition (41). Therefore, elements such as decreased insulin sensitivity, physical activity levels, risk for prediabetes and type 2 diabetes mellitus (T2DM), and the patient’s resources and preferences should be accounted for when recommending carbohydrate intake.
Recently, different diet recommendations have been introduced, most importantly the Mediterranean diet. The Mediterranean diet is mainly based on plant foods and unsaturated fats and is devoid of processed foods and saturated fats. It has shown positive effects on metabolic markers and reduced the risk of chronic disease, with or without weight loss (34, 39). A Mediterranean diet can be appropriate for the specific hormone changes linked to menopause since it provides a structured approach to increase lean protein, fiber rich carbohydrates, and antioxidant intake. It also decreases the intake of simple sugars and saturated fats. These adjustments may reduce the adverse effects of metabolism during the menopause transition. Greater adherence to a Mediterranean eating pattern among peri- and postmenopausal women may also contribute to improved metabolic health and weight loss outcomes (34).
Intermittent fasting and time-restricted eating are other approaches that showed promise as a therapeutic strategy for managing menopausal symptoms and weight gain and improving overall health (23, 42).
Sleep
During menopausal transition, 40–48% of women experience sleep disturbance (43), and chronic sleep disturbance can have metabolic effects through increasing the risk for weight gain (44). Multiple factors contribute to sleep disturbance in peri- and postmenopausal women, including age, hormonal changes, sleep apnea, vasomotor symptoms, anxiety, and stress, among other factors (45). Care for postmenopausal women should involve a thorough physical examination, sleep history, and referral for a sleep study. Based on the outcomes of the evaluation, behavioral interventions like cognitive behavioral therapy for insomnia, physical activity, and mindfulness or relaxation techniques can be effective treatments for peri- and postmenopausal women (46).
Hormonal Considerations
The most effective treatment for menopausal vasomotor symptoms is hormone replacement therapy (HRT), as it achieves a 75% reduction in frequency and severity (47). It also can improve quality of life in symptomatic women (48). Its use in healthy women younger than 60 years and menopausal women within 10 years of menopause is supported by current research (36, 49).
Obese perimenopausal women have a higher risk of developing menopausal vasomotor symptoms, thus more require HRT. However, HRT is associated with increased risks of breast and endometrial cancers, venous thromboembolism, and cardiovascular complications, especially in women with obesity (Opoku). Given that, the European Menopause and Andropause Society provided guidelines for the management of obese postmenopausal women, highlighting the importance of carefully weighing the risks and benefits before starting HRT (49). If indicated, estrogen patches with micronized progesterone should be used with the lowest dose for a short duration (49, 50).
The effects of HRT itself in postmenopausal weight management were examined by multiple studies. Evidence on the role of HRT in postmenopausal weight management, particularly muscle strength and mass, is inconsistent. Some studies reported a potential benefit, while others showed insignificant change (4). Hormonal therapy can lead to small but measurable prevention of losing muscle strength and mass in postmenopausal women (51). Currently, there is no definitive evidence that HRT leads to greater weight gain than aging itself; however, its use appears to help preserve muscle mass (52). In both human and animal studies, estrogen therapy has been shown to overcome estrogen depletion associated with weight gain and body fat redistribution that occur in menopause (17, 20, 27). Furthermore, HRT has shown effectiveness in reducing central adiposity and preserving lean body mass in postmenopausal women (16, 22, 53). The inconsistency in research is attributed to the difficulty controlling all factors that can affect muscle mass and strength, such as HRT administration, age, nutrition, physical activity, and treatment duration (52). Notably, hormone replacement therapy was found to be associated with a lower diagnosis of new-onset T2DM; however, it is not approved by the Food and Drug Administration (FDA) for this indication (53).
At present, there is insufficient strong evidence to confirm that HRT independently reduces abdominal fat gain, as isolating this effect in studies is challenging. Current guidelines advise against using menopausal HRT to prevent or treat weight gain and visceral fat accumulation associated with the menopausal transition, as the potential risks outweigh the benefits (36, 49).
Women's Experiences during Menopause
A recent qualitative study investigated personal experiences of menopause among Black women (8). It also explored their interest in lifestyle programs for weight management, and the enablers and barriers to healthy life during this transition. Most participants in this study described menopause as a pivotal life event influencing both physical and mental health. They also mentioned receiving minimal support and showed interest in integrating a weight management lifestyle program into their daily life. Women spoke about their previous exercise habits rather than their current exercise habits, attributing decreased physical activity to increased life demands such as work and caregiving. Diet and exercise were considered motivating and enjoyable when associated with social support; however, social support is still lacking (54).
Another study explored the experience of menopause among postmenopausal women in Taiwan (55). It found strong motivation to participate in weight reduction programs among obese and overweight postmenopausal women. The most effective reported motivators were supportive environments, such as health messages provided by healthcare providers and the government and informative posters in gynecology outpatient departments. Participants in this study considered weight management as a health necessity that can improve self-image, make them feel younger and more attractive, and gain a sense of control over their lives.
Conclusion
Menopause is a critical life stage characterized by physiological, hormonal, and lifestyle changes that can remarkably influence metabolic health, weight, and body composition. Lifestyle interventions, including physical activity and nutrition, show promising benefits in managing weight and improving overall health, though more targeted research is needed. Hormone replacement therapy may aid in maintaining lean body mass and reducing central adiposity but remains controversial due to associated risks. Ultimately, individualized, evidence-based strategies that consider hormonal, behavioral, and social factors are essential to support women through this pivotal transition.
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Non-applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.