Volume 5, Issue 7
July 2025
Persistent Hyperinflammation in Children with Adenovirus Pneumonia Requiring Intensive Support
Salah Alzanbagi, Zaki Alhothli, Mubarak Alazemi, Hamad Alshammy, Sulaiman Alosaimi, Ahmed Alhejalili, Manar Almutairi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50709
Keywords: Adenovirus, Adenovirus Pneumonia, Children, Hyperinflammation. Cytokine Storm
Human adenovirus (HAdV) is one of the most common causes of pneumonia in children. It can lead to severe adenovirus pneumonia, increasing the risk of serious complications, morbidity, and mortality. Both innate and adaptive immunity systems respond to adenovirus infection. However, this immune response may be excessive, causing a pathologic immune condition called ‘hyperinflammation’. Evidence on mechanisms and management of hyperinflammation in children with adenovirus pneumonia is lacking. The aim of this review is to explore current evidence that involves data on persistent hyperinflammation in children with adenovirus pneumonia requiring intensive support. In the early phase, adenovirus pneumonia is characterized by non-specific symptoms such as fever, wheezing, and cough. This infection may induce hyperinflammation that can further worsen the condition, leading to severe adenovirus pneumonia that may require intensive support. Excessive cytokine release may occur, resulting in what’s described “cytokine storm”, leading to hypoxia, vascular leakage, pulmonary edema, and potentially acute respiratory distress syndrome. These cytokines include interleukin-1α (IL-1α), IL-1β, IL-6, IL-8, IL-12, IFN-γ, IFN-α2, and tumor necrosis factor (TNF). Various approaches were introduced to mitigate the effects of hyperinflammation, including blood purification, glucocorticoids, and immunoglobulins. Further research is urgently needed to elucidate the immunopathology of adenovirus-induced hyperinflammation and to establish evidence-based treatment protocols tailored to the pediatric population.
Introduction
Human adenovirus (HAdV) is a common cause of pediatric pneumonia, accounting for 4%–19% of all pediatric pneumonia cases (1), 5%–10% of all lower respiratory tract infections in children, and 2%–5% of all respiratory illnesses in children (2, 3). It commonly occurs in children aged 6 months to 5 years (4). The incidence of severe adenovirus pneumonia is about 32% of all pediatric severe pneumonias (5). Severe adenovirus pneumonia typically manifests dyspnea, high fever, wheezing, hypoxia, and multisystem disorders (1, 5). However, early diagnosis of HAdV through nonspecific clinical symptoms is difficult because children's immune systems, particularly their humoral immunity, are still underdeveloped, and they are more vulnerable to severe infections (6). This immaturity helps explain the higher mortality rates and the increased likelihood of progression to severe disease with potentially serious long-term complications (7).
Both adaptive and innate immunity systems are activated in response to HAdV infection (8). The infection can induce the secretion of IL-1, IL-2, TNF, macrophage inflammatory protein, and macrophage inflammatory protein (9). These cytokines have an antiviral function and limit the amplification and spread of the virus. Natural killer cells are also activated to attack cells infected with virus (10). On the other hand, viral components suppress the transcription of interferon-inducible genes, a process that promotes viral replication (11).
The immune response in some cases of HAdV infection can be pathological in lungs and systemically. This pathological immune response is described as ‘hyperinflammation’ and results in immune-mediated end-organ damage that can compromise gas exchange (12). This abnormal immune response can lead to pneumonia and acute respiratory distress syndrome (ARDS) that requires mechanical ventilation. It also can lead to failure of other organs, contributing to global deaths due to pneumonia (13).
The mechanisms and effects of hyperinflammation in children with adenovirus pneumonia are still unclear. Thus, the aim of this review is to explore current evidence that discusses persistent hyperinflammation in children with adenovirus pneumonia that requires intensive support, highlighting various interventions introduced to manage this condition.
Methods
A comprehensive literature search was conducted in Medline (via PubMed), Scopus, and Web of Science databases up to June 1, 2025. Medical Subject Headings (MeSH) and relevant free-text keywords were used to identify synonyms. Boolean operators (AND’, OR’) were applied to combine search terms in alignment with guidance from the Cochrane Handbook for Systematic Reviews of Interventions. Key search terms included: “Adenovirus” OR “Adenovirus Pneumonia” OR “Pneumonia” AND “Hyperinflammation” OR “Persistent Hyperinflammation” OR “Cytokine Storm” OR AND “Children” OR “Pediatrics”. Summaries and duplicates of the found studies were exported and removed by EndNoteX8. Any study that discusses the persistent hyperinflammation in children with adenovirus pneumonia requiring intensive support and published in peer-reviewed journals was included. All languages are included. Full-text articles, case series, and abstracts with the related topics are included. Case reports, comments, animal studies and letters were excluded.
Discussion
Clinical Features of Adenovirus Pneumonia
The most significant predictors of severe HAdV pneumonia in children are wheezing, fever duration >4.5 days, serum ferritin (SF) ≥139.60 ng/mL, and neutrophil percentage (NEUT%) ≥47.60. It is associated with high mortality, morbidity, and long-term complications in 14–60% of cases (14, 15). Thus, it is critical to identify and manage HAdV pneumonia early since there is no specific antiviral treatment, especially for its severe form (16, 17).
There are no statistically significant gender differences in the susceptibility of infection with HAdV, as the male-to-female ratio is 1.15:1(18). Although some studies suggest boys may be more susceptible (19), further large-scale studies are needed. Global reports state that it most commonly affects children under 5 years (84.2%) (18). Notably, 26% of severe cases were reported in children >5 years old, indicating an increased risk of critical illness in older children; however, this finding is inconsistent between studies (20).
The incubation period of HAdV is 3–8 days, manifested with high fever, cough, and wheezing (18). The duration of fever is significantly longer in severe cases, indicating that prolonged fever (≥7 days) is correlated with severity of the disease (18). A recent study further narrowed the risk threshold to >4.5 days. Furthermore, wheezing, especially if persistent, is more common in severe cases (24.76%) and indicates poor prognosis. HAdV may also lead to systemic adverse effects, including coagulation disorders, electrolyte imbalances, and liver injury. These systemic adverse effects are also more prevalent in severe cases, highlighting the need for monitoring for multisystem involvement (21).
The auscultatory findings of HAdV pneumonia may appear after radiographic changes, making imaging a critical tool for early diagnosis. In non-severe cases, X-rays can be useful as they can detect pulmonary texture thickening, while in severe cases (20), CT scans can detect higher rates of consolidation, pleural effusion, and atelectasis. Therefore, CT is recommended for assessing complications or when clinical and imaging findings are discordant (22). Lab findings in severe cases typically show elevated inflammatory markers, including WBC, NEUT%, CRP, IL-6, SF, ESR, IgG, IgA, and IgM.
Pathogenesis of Adenovirus Pneumonia
HAdV infection is typically self-limiting and resolves in 7-10 days without medical treatment and without significant effect on inflammatory markers (16). However, some species such as HAdV-B14p1, HAdV-B7, and HAdV-B3 may lead to severe respiratory diseases, including acute respiratory distress syndrome and pneumonia, and significant immune changes (16). Increased levels of pro-inflammatory cytokines and chemokines were observed in the plasma, serum, and bronchoalveolar lavage fluid of immunocompetent children and adults with pneumonia caused by HAdV-B3 and B7 (23). These cytokines include IL-1α, IL-1β, IL-6, IL-8, IL-12, IFN-γ, IFN-α2, and TNF-α, while chemokines include CCL2, CCL3, and CXCL10 (24-27). These responses are systemic and stereotypic, with prolonged increases of these cytokines in severe cases (>2 weeks), while levels dropped by day 14 in milder infections (25). The severity of HAdV in pediatrics is correlated with the high levels of the pro-inflammatory cytokine levels (25).
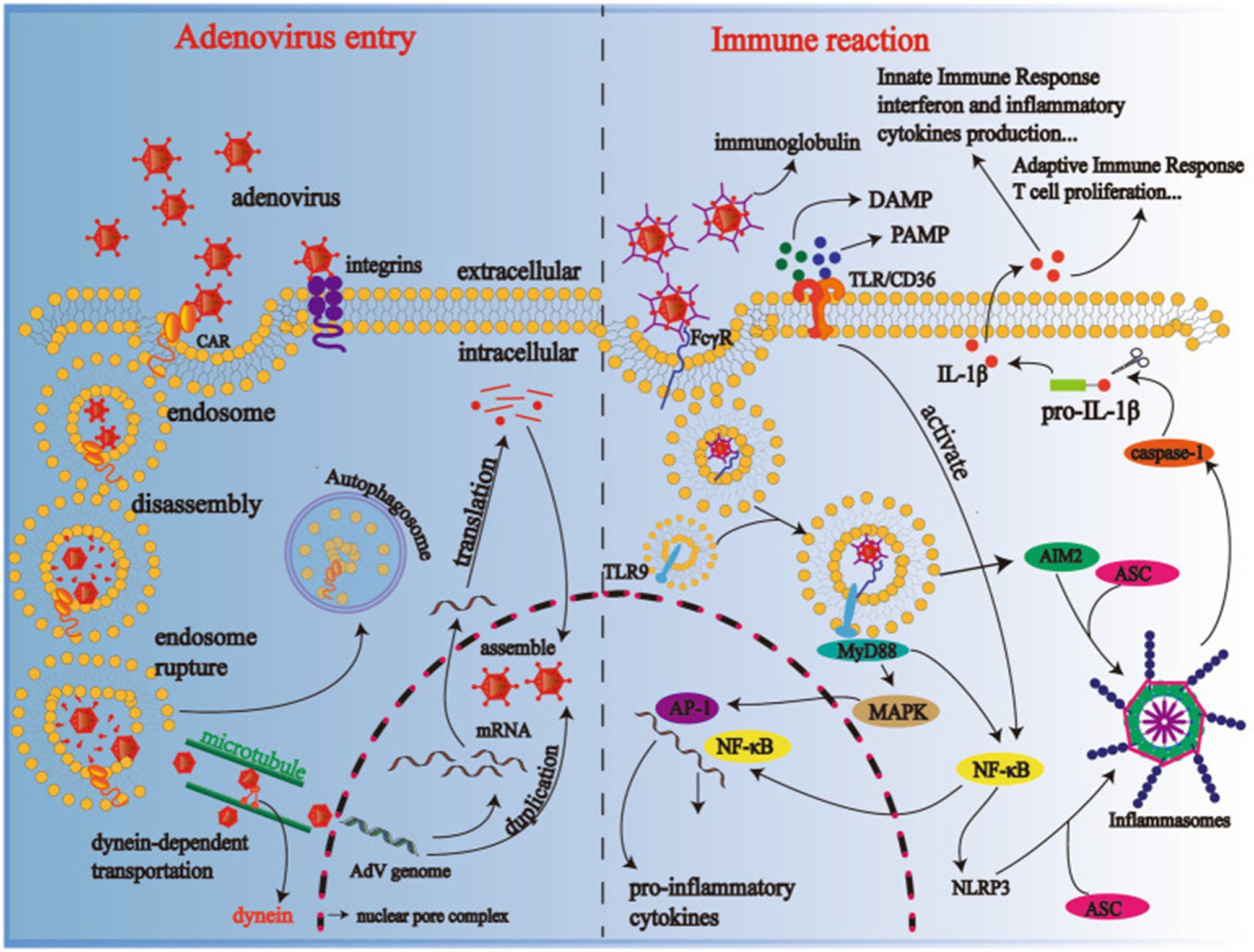
Once the adenovirus enters the body, the Fcy receptors on dendritic cells and macrophages recognize virus-antibody complexes, resulting in endocytosis (6). Then the viral DNA interacts with Toll-like receptor 9 (TLR9) inside the cells, which activates the MyD88-dependent pathway, inducing the release of cytokines via MAPK/AP-1 and NF-κB signaling (28, 29). Scavenger receptor A also activates the immune system through cellular endocytosis (30). Furthermore, danger-associated molecular patterns (DAMPs) and pathogen-associated molecular patterns (PAMPs) bind to receptors, including CD36 and TLR, activating NF-κB, which activates NLRP3 inflammasomes and AIM2. These engage with ASC and caspase-1, converting pro-IL-1β to IL-1β and inducing inflammation (31, 32).
Previous evidence has been focused on canonical inflammasomes like AIM2 and NLRP3 (28, 33, 34). A recent study investigated the activation of noncanonical inflammasomes during HAdV infection, particularly caspase-4 and caspase-5 (35). The study performed an analysis of GEO datasets and found increased expression of caspase-4 and caspase-5 in pediatric patients with adenovirus pneumonia, which correlates with disease severity. The study also used THP-1-derived macrophages as an in vitro model and found that HAdV-3 infection activated intracellular caspase-4 and caspase-5, induced GSDMD cleavage and macrophage pyroptosis, and silenced caspase-4/5 reduced GSDMD cleavage and virus release, without affecting viral entry or replication, suggesting pyroptosis facilitates virion egress (35).
The study also explored the signaling pathways and showed that STING signaling contributed to canonical inflammasome activation but not to noncanonical caspase-4/5 activation. The NF-κB and TLR9 pathways have been shown to play a key role in triggering the expression and cleavage of caspase-4/5 (35). This was confirmed by NF-κB inhibitor experiments. Thus, the study suggested that TLR9-NF-κB signaling, not STING, is the primary driver of noncanonical inflammasome activation in HAdV infection.
Although the canonical and noncanonical inflammasomes independently induce pyroptosis, both can act synergistically in some infections. This occurs when caspases-4/5/11 induce K+ efflux, which activates NLRP3 (31). In contrast, caspase-1 can activate IL-18, which primes caspase-11 via IFN-γ (36). Notably, caspase-11 is not necessarily essential for caspase-1 activation, as it depends on the pathogen (37). Therefore, the study stated that HAdV-3 infection activates noncanonical inflammasomes, including caspase-4 and caspase-5, causing macrophage pyroptosis and enhanced virus release. Silencing these caspases decreased virus titers in vitro, highlighting their role in viral dissemination. Furthermore, clinical severity of infection is correlated with high caspase-4/5 expression, making them potential biomarkers for adenovirus pneumonia prognosis (35). Mechanisms of adenovirus entry to human cells and body immune response are shown in Figure 1.
Hyperinflammation in Adenovirus Infection
Adenovirus pneumonia in pediatrics may lead to persistent hyperinflammation, causing indirect tissue damage primarily by activating the host immune system. Cytokines play a pivotal role in regulating immune response against different viruses, including adenovirus; however, an abnormal excessive activation of cytokines “cytokine storm” can lead to serious harm to the human body (6). This cytokine storm may result in apoptosis of alveolar endothelial and epithelial cells and disruption of the alveolar-capillary barrier, leading to hypoxia, vascular leakage, pulmonary edema, and potentially acute respiratory distress syndrome (38). The lungs start to repair in the late phase of adenovirus infection through the accumulation of macrophages secreting growth factors, including transforming growth factor-beta (TGF-β) and epidermal growth factor (39).
TGF-β has a role in fibroblast-to-myofibroblast differentiation, epithelial–mesenchymal transition (40), and apoptosis of type II alveolar epithelial cells (41). The consequences of these actions are fibroblast proliferation, extracellular matrix deposition, and reduction of surfactant, leading to airway fibrosis and possibly post-infectious bronchiolitis obliterans (PIBO).
Treatment of Adenovirus Pneumonia
As mentioned above, it is critical to early identification and management of adenovirus infection. In the early phase, general treatment is recommended, including isolation to prevent cross-infection, fever reduction, and organ function monitoring (heart, liver, kidneys) (6). Cidofovir is a broad-spectrum antiviral that should also be administered, as it inhibits viral DNA polymerase; however, it is nephrotoxic and suppresses bone marrow (16, 42). Ribavirin has shown some efficacy, but it lacks strong clinical support (43, 44). Brincidofovir is a lipid-conjugated cidofovir with lower toxicity; it is more effective in hematopoietic stem cell transplantation patients (45). In vitro experiments showed that heparin and derivatives inhibit viral entry and cytokine activity (IL-6, IFN-γ), but risks like bleeding require further trials (46, 47).
These patients may also need respiratory support and bronchoalveolar lavage (BAL); choosing whether noninvasive or invasive ventilation is more appropriate depends on severity. High-flow nasal cannula can provide humidified oxygen with fewer complications compared to invasive ventilation (48). Bronchoscopy and BAL are typically used to remove mucus plugs, thus improving diagnosis and recovery; however, benefits in mild versus severe cases remain debatable (49). Extracorporeal membrane oxygenation (ECMO) is always an option for refractory cases unresponsive to ventilation. Its survival rate in newborns is 13.6% and 51% in children. Notably, delayed ECMO is associated with increased mortality (50).
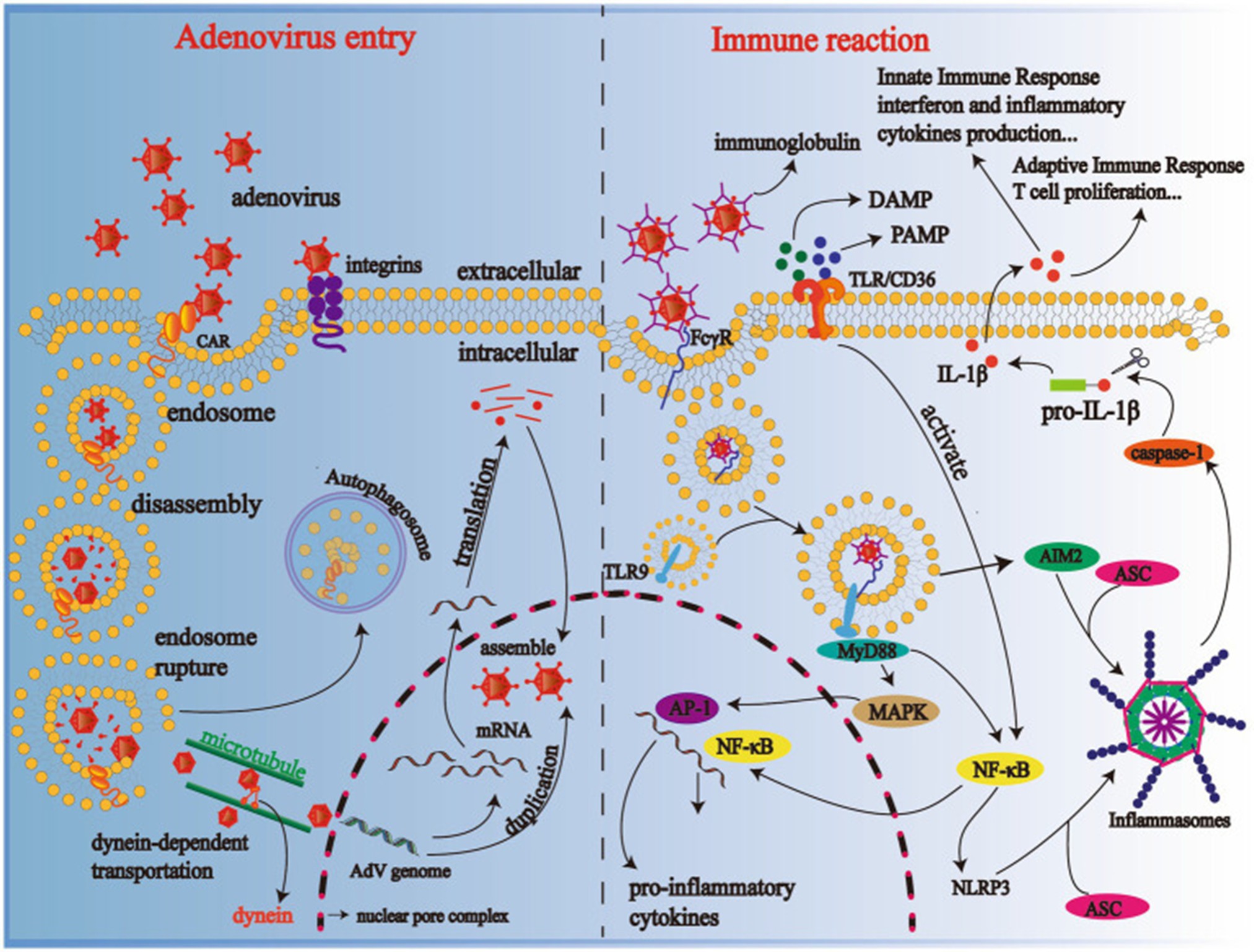
Figure 1: Mechanism of adenovirus entry to human cells and body immune response (6).
Treatment of hyperinflammation
Various interventions have been introduced to manage hyperinflammation in children with adenovirus pneumonia, such as blood purification and immunoregulation therapy. Blood purification can selectively get rid of inflammatory cytokines and mitigate the harm to the body. Therefore, it can prevent excessive immunity and achieve therapeutic purposes (51). Blood purification can also manage fluid overload associated with adenovirus-induced organ dysfunction (52). Avoiding this in early stages can reduce the duration of mechanical ventilation, morbidity, and mortality (53). However, evidence supporting blood purification effectiveness is still lacking, particularly in children with adenovirus pneumonia.
Various immunoregulation therapies are available, including glucocorticoids, intravenous immunoglobulin, and monoclonal antibodies (6). Immunoglobulin is a group of immune proteins produced by B lymphocytes, mainly composed of IgG. These proteins can bind and inactivate inflammatory factors like IL-1 and TNF-α, achieving an anti-inflammation purpose. They also block intercellular interactions mediated by cell surface receptors, achieving an important immunoregulatory function; however, their exact effect and mechanisms still need further clarification (54).
On the other hand, glucocorticoids are known to have immunoregulatory, anti-inflammatory, and antishock effects. Early administration of glucocorticoids in these cases has been shown to enhance the success rate of treatment (55), decrease the requirement for invasive ventilation, reduce the incidence of ARDS, and reduce inpatient mortality (56). However, the associated side effects, including water and sodium retention and infection, make the decision of whether and how to administer glucocorticoids in clinical practice require comprehensive judgment (56). Furthermore, clinical trials on using virus-specific T lymphocyte transplantation have shown positive results in children infected with adenovirus after hematopoietic stem cell transplantation (57).
As previously mentioned, cytokine storms are a key mechanism underlying severe adenovirus pneumonia. Therefore, monoclonal antibodies targeting pro-inflammatory cytokines, such as TNF-α and IL-6, have been proposed as potential therapeutic options (6). During the COVID-19 pandemic, some studies observed that patients who received TNF inhibitors tended to have improved outcomes (58, 59). However, the use of these agents in viral infections remains controversial. One major concern is that TNF-α inhibition may increase the risk of secondary bacterial or fungal infections, and the full range of side effects in the context of viral illnesses is not yet well understood (60).
Conclusion
Adenovirus pneumonia in children is often complicated by a hyperinflammatory response that contributes to significant morbidity, mortality, and long-term respiratory sequelae. While various immune pathways, including canonical and noncanonical inflammasome activation, have been implicated, the precise mechanisms underlying persistent hyperinflammation remain poorly understood. Current therapeutic strategies such as blood purification, immunoglobulin therapy, and cytokine-targeted monoclonal antibodies show promise but lack robust pediatric-specific clinical evidence. Therefore, further research is urgently needed to elucidate the immunopathology of adenovirus-induced hyperinflammation and to establish evidence-based treatment protocols tailored to the pediatric population.
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Non-applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.