Volume 5, Issue 7
July 2025
Targeted Temperature Management for Post- Cardiac Arrest Patients
Mazen Alaadeen Nassar, Abdulmohsen Khlaif Alanazi, Adel Khaled Idris, Hassan Abdullah Mohammed Balkhi, Wajd Ramzi Falemban, Badr Adnan Hassan Banani, Sara Waleed Hefni, Abdulkader Jouma Akil, Mohammed Sulaiman Alaslani, Turki Dubayyan Altowairqi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50710
Keywords: targeted temperature, targeted temperature management, TTM, post-cardiac arrest, hypothermia
Cardiac arrest remains one of the leading causes of sudden death and sustained long-term neurological damage, and despite advancements in the immediate response protocols employed by emergency care providers, survival devoid of any mental impairment remains uncommon. Restoration of spontaneous circulation marks a critical milestone in cardiac arrest management; however, it does not guarantee neurological recovery, as prolonged oxygen deprivation and cerebral ischemia often result in significant cognitive impairment. Healthcare professionals continually inquire about cerebral neuroprotection to maintain the neurological function and outcomes and improve survival rate. Recently, targeted temperature management has become an essential concept in the standard post-cardiac arrest protocol. Reducing body temperature diminishes excessive metabolism, alleviates excitatory neurotransmitters, and mitigates the inflammatory response that arises after the initial shock. Initial investigations suggested a reduction in the frequency of patients experiencing confusion or complete unresponsiveness upon recovery. Additionally, this investigation raises various questions about what the optimal targeted temperature is and its ideal time and duration. This review evaluates the debates and current protocols and focuses on the variability of the primary multicenter trials in comparison, patients’ outcomes, and technology usage. Regarding recommendations, targeted temperature management remains a vital intervention in post-cardiac arrest management. Physicians must accurately use customized protocols according to patient-specific variables in alignment with the standard guidelines for the targeted temperature management procedure. Additional research is critical in refining temperature targets, understanding the ideal strategies, and increasing the neuroprotection in the patient recovery after having cardiac arrest.
Introduction
Cardiac arrest remains the major cause of mortality and neurological impairment worldwide. Annually, more than 350,000 individuals in the United States of America (USA) have out-of-hospital cardiac arrest (1). Typically, in-hospital cardiac arrest presents significantly enhanced survival outcomes; however, it is still clinically concerning due to high morbidity. Despite advances in emergency cardiovascular care, a considerable group of survivors endure different degrees of hypoxic-ischemic brain damage (2). The primary determinants for the long-term prognosis in survivors exhibiting coma, cognitive dysfunction, and persistent vegetative condition are the neurological findings. Thus, effective post-recovery treatment is essential to prevent the elevated number of chronic neurological complications (3).
The neurological impairment detected during the spontaneous circulation restoration is typically attributed to reperfusion injury and cerebral ischemia. The initial cerebral ischemic event following cardiac arrest results in an abrupt cessation of cerebral blood flow, leading to extensive neuronal hypoxia and a shift to anaerobic metabolism (4). This leads to increased acidity of cells and the entrance of calcium ions to the cell and releases the excitotoxic neurotransmitters. After restoring the normal blood flow, the reactive oxygen species (ROS) and pro-inflammatory cytokines resulting from oxygen paradoxically increase the neural damage that leads to immediate cascades of cell apoptosis and necrosis in certain vulnerable cerebral areas such as the cerebral cortex and hippocampus (5). After spontaneous circulation returns, further damage might occur and last for hours to days; thus, the rapid cessation of further neurological damage is essential (6).
Typically, healthcare professionals refer to this approach as targeted temperature management (TTM) or therapeutic hypothermia. The fundamental concept is to intentionally reduce the patient’s core temperature (7). Reducing the temperature alleviates energy requirements and allows affected cerebral tissue to stabilize. In major procedures, the temperature remains between 33°C and 36°C (8), a range sufficiently mild to prevent frostbite while effectively mitigating issues such as neuroinflammation, oxidative stress, and excitotoxicity (9). Cell membranes stabilize, uncontrolled apoptosis diminishes, and brain autoregulation receives an opportunity for recovery. All of these mechanisms act collaboratively to preserve neuronal viability and prevent cerebral edema (9). Clinical trials consistently demonstrated that patients with previous cardiac events who had immediate TTM after recovery have superior neurological outcomes and a higher rate of discharge from the ICU. Particularly in patients with initial shockable rhythms (10). Regulating temperature has become a standard procedure in post-myocardial infarction therapy (11).
The concept of targeted temperature control gained significant interest in 2002 as a result of the findings that various studies demonstrated that applying therapeutic hypothermia to patients who survived out-of-hospital cardiac arrest to a temperature range of 32°C to 34°C could preserve superior brain function (12). Consequently, both the AHA and the European Resuscitation Council promptly incorporated the TTM procedure into their guidelines. The recent studies about TTM and its continuation, TTM2, have begun to challenge the universal applicability of the 33°C guideline (13). These studies raised questions about what the optimal target temperature, duration, and time of therapy are. Significantly, the findings of these studies indicate no difference between the outcomes from the patients maintained at 36°C and those maintained at 33°C, thus promoting tailored targeted temperature strategies designed to prevent hyperthermia rather than hypothermia (14).
This review aims to evaluate the evidence regarding targeted temperature management in adult patients post-cardiac arrest. And it will examine the pathophysiological basis of TTM, summarize contemporary clinical trials, assess the efficacy of various temperature targets, and evaluate practical considerations in the execution of TTM. Additionally, this article will discuss guideline advancements, issues, and future research to improve neuroprotection and enhance the clinical outcomes in the high-risk groups.
Methodology
A comprehensive literature search in the PubMed, Web of Science, ScienceDirect, and Cochrane databases on June 10, 2025. The search utilized medical topic headings (MeSH) and relevant keywords such as ‘targeted temperature’, targeted temperature management’, ‘TTM’, ‘post-cardiac arrest’, ‘hypothermia’, and a combination of all available related terms. Peer-reviewed articles involving human subjects and available in the English language were included. Reference lists of studies included were screened to identify additional relevant publications. There were no limitations on date, publication type, or participant age.
Discussion
Pathophysiological basis for targeted temperature management
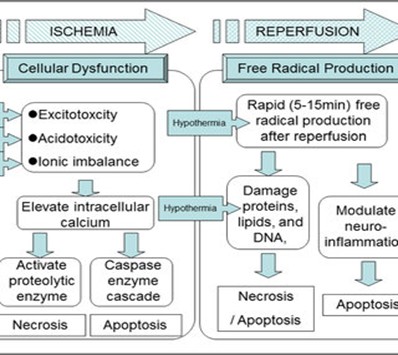
Addressing the mechanisms of cerebral ischemia-reperfusion damage contributes to improvement in the control of neurologic recovery in post-cardiac arrest patients. In the cardiac arrest condition, the blood flow to the brain is reduced and neurons rapidly become hypoxic (15). The absence of perfusion leads to anaerobic metabolism and intracellular acidosis and ATP depletion, which exacerbates several other damage mechanisms of cytotoxic edema, calcium influx, and excitotoxicity via excessive glutamate (16). Upon hemodynamic resuscitation, reoxygenation contributes to both an early resuscitation-recovery function of oxygen and a recovery-associated oxygen damage, this latter being primarily due to oxidative stress, with increased free radical formation, mitochondrial dysfunction, and inflammation upregulation (Figure 1) (17). All these processes impair the blood-brain barrier, allowing apoptosis and neurodegeneration. Furthermore, hyperthermia exacerbates brain damage following cardiac arrest (18). Elevated temperature increases metabolic consumption, increases free radical production, and augments the inflammatory response, which collectively increases neuronal damage and worsens neurological outcomes. It is well established that the clinical database about post-recovery hypothermia is consistently limited (19). Targeted temperature management provides neuroprotection by decreasing cerebral metabolic rate, which leads to the preservation of intracellular energy stores and stabilization of mitochondrial function (20). Furthermore, hypothermia prevents excitotoxicity through reduction of glutamate release and inhibits inflammatory cytokine expression, decreasing secondary brain damage. These cellular processes support the theoretical strategy about early TTM for post-cardiac arrest patients, aiming to attenuate irreversible brain damage and enhance long-term neurological recovery (21).
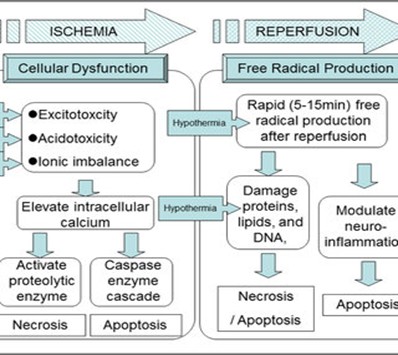
Figure 1: Traumatic brain injury (17).
Historical development and clinical trials
The justification for therapeutic hypothermia as a neuroprotective approach emerged from animal studies demonstrating enhanced neurological recovery and decreased infarct volume following induced hypothermia after brain ischemia. Initial animal research informed human trials on post-cardiac arrest care that employed different degrees of temperature regulation (21). In 2002, two pivotal randomized controlled trials published by the Hypothermia After Cardiac Arrest (HACA) study group and Bernard et al. established the clinical importance of targeted temperature management (22). Both studies demonstrated improved survival and neurological outcomes for patients who were comatose after out-of-hospital cardiac arrest (OHCA) and treated hypothermia at 32°C to 34°C. As a clinical practice, TTM became a widely recommended intervention for OHCA in international resuscitation guidelines (23). This consensus was challenged by subsequent trials in recent years, including the TTM and TTM2 studies, where hypothermia at 33°C did not demonstrate a significant benefit over normothermia at 36°C in terms of neurologically intact survival (24). The subsequent TTM2 trials called into question the efficacy of active hypothermic temperature management by demonstrating that normothermia with active fever prevention was not inferior to active hypothermia with fever prevention. A renewed emphasis emerged to reassess the therapeutic efficacy of TTM, as the focus shifted from fixed hypothermia targets to individualized temperature modulation strategies to personalized temperature management (25). Current evidence suggests that preventing hyperthermia may be more critical than inducing hypothermia; however, the optimal temperature remains ambiguous (26).
Techniques of inducing and maintaining targeted temperature management
Targeted temperature management (TTM) is a structured therapeutic protocol that includes induction, maintenance, and controlled rewarming phases. Many different methods, Both invasive and non-invasive methods are available for inducing and maintaining core body temperature across various clinical settings. Non-invasive surface cooling methods—such as cooling blankets, pads, or gel-coated wraps—can be readily applied and offer user-friendly temperature modulation (Figure 2) (27). These devices typically include automated feedback mechanisms for temperature regulation, although their precision may be limited in certain clinical scenarios compared to invasive methods (28). Invasive techniques, such as endovascular cooling catheters, offer more precise core temperature control by circulating cooled saline through a closed-loop system placed in a central vein (29). While effective, this approach requires central venous access and carries associated procedural risks. Although previously used during the induction phase to expedite cooling, the rapid infusion of cold intravenous fluids is now less favored due to emerging evidence highlighting risks of hemodynamic instability (29). Temperature monitoring is crucial in all aspects of TTM. Core temperature is usually measured with esophageal, bladder, or intravascular probes to avoid complications. The rewarming process should be gradual, not the instructed recommended rate of 0.25–0.5°C per hour. Too rapid a rewarming phase can result in rebound hyperthermia, electrolyte/intravascular fluid disturbances, and hemodynamic instability, all of which can elucidate the neuroprotective effects of TTM (30).
Figure 2: Cooling techniques for targeted temperature management (27).
Clinical indications and patient selection
Targeted temperature management is often indicated for comatose adult patients after out-of-hospital cardiac arrest (OHCA) and is considered the optimal technique for patients with shockable rhythms such as ventricular fibrillation or pulseless ventricular tachycardia, who have demonstrated the maximum benefit from TTM therapy in studies (31). TTM may subsequently be tolerated in patients with non-shockable rhythms and some patients with in-hospital cardiac arrest (IHCA) circumstances; prognostically, both IHCA and non-shockable rhythms have worse outcomes compared to OHCA (32). Clinical experience and judgment are imperative to employ for patients with IHCA, as OHCA and IHCA involve important differences in terms of etiology and baseline comorbidities. It is essential for healthcare providers to be cognizant of the potential need for neurological assessment prior to starting TTM (33). Comatose status definition typically involves a Glasgow Coma Scale (GCS) of ≤ 8 after a return of spontaneous circulation (ROSC) (34). While some early prognostication is possible in the patients' first 72 hours post-cardiac arrest, it is particularly challenging to adhere to protocols to conduct neurological assessment in patients receiving TTM because of the confounding effects sedatives and hypothermia have on assessment and classification of comatose (35). Exclusion criteria will include active bleeding, severe coagulopathy, terminal advanced malignancy, intracranial hemorrhage, or pre-existing terminal illness. Risk-adjusted exclusion criteria should account for age, time to ROSC, initial rhythm, and pre-arrest functional status (36). These dimensions will allow practitioners to risk stratify patients and identify those most likely to derive benefit from TTM and optimize exposure for patients with limited recovery potential.
TTM complication and management
Targeted temperature management can have substantial neuroprotective effects; however, TTM can have complications that require cautious observation and intervention. Coagulopathy can occur because cold-induced platelet dysfunction and suppression of the hemostatic effects of the coagulation cascade can lead to vasodilation and an increased tendency to bleed (37). Electrolyte derangements can occur when implementing the TTM-hypothermia phase and the TTM-rewarming phase and will need regular laboratory surveillance and correction. Examples of electrolyte derangements include, but are not limited to, hypokalemia, hypomagnesemia, and hypophosphatemia (38). Substantial cooling can suppress immune function and can increase the risk for various infectious disease complications, such as pneumonia and sepsis, and in patients with prolonged mechanical ventilation (39). Finally, TTM-Cooling and TTM-Rewarming may lead to arrhythmias (e.g., bradyarrhythmias). Clinically significant arrhythmias were observed to be infrequent in patients placed in mild hypothermia protocols. TTM requires intense management, with a high dependence on supportive care (40, 41). Effective TTM depends on continuous monitoring of core temperature, accomplished by placement of an esophageal, bladder, or intravascular probe. However, hemodynamic measurements, electrolytes, and coagulation measures must be monitored (42). Shivering is a physiological response to hypothermia that is metabolically expensive and unproductive. Consequently, it is necessary to actively suppress shivering pharmacologically with at least one of the following agents; however, sedatives are preferred: either sedatives (e.g., propofol, midazolam) or neuromuscular relaxants (43). Although non-pharmacological techniques, such as external counter-warming techniques, may provide an avenue to enhancing comfort, utilizing sedatives is necessary to maintain comfort, reduce shivering, and harness the biggest potential neuroprotection effects of therapeutic temperature management (TTM) (44).
Outcomes and prognostic factors
The two principal outcomes for targeted temperature management are survival and neurologic recovery. Neurologic recovery is typically assessed with neuroscience-administered scales like the modified Rankin Scale (mRS) and the Cerebral Performance Category (CPC), with CPC scores of 1-2 and mRS scores recognized as optimal indicators of enhanced function (45). There is a wealth of evidence, including randomized controlled trials and meta-analyses, that supports the utilization of TTM as a strategy to enhance the potential for effective neurologic recovery in comatose patients who survived an out-of-hospital cardiac arrest. This is particularly effective if the presenting rhythm is shockable and TTM is applied early (24). TTM impacts overall survival, prior literature highlighted the effects of TTM on survival rates; however, more contemporary investigations, most notably TTM and TTM2, showed there to be no definitive mortality benefit associated with a targeted temperature aim (33°C versus 36°C or normothermia) (46). However, we should steer clear of hyperthermia, as studies have linked it to negative consequences. The most supportive predictors of favorable prognosis are short time from arrest to return of spontaneous circulation (ROSC), initial shockable rhythm, younger age, and absence of significant comorbidities (47). Adverse prognosis is associated with long downtime, unreactive pupils, serum neuron-specific enolase (NSE) level stroke, and prolonged burst suppression on EEG. While neuroprognostication can be informative, it should not be applied prior to at least 72 hours out from the arrest for all patients, and especially in TTM patients, to consider the possible confounding effects of sedation and hypothermia on clinical and electroencephalography (EEG) assessments (48).
Guidelines and recommendations
According to the recent international guidelines, targeted temperature management is an essential aspect of post-cardiac arrest care. The European Resuscitation Council (ERC), the American Heart Association (AHA), and the International Liaison Committee on Resuscitation (ILCOR) unanimously agree that TTM is indicated for comatose adults who have experienced an out-of-hospital cardiac arrest irrespective of their initial rhythm. Aiming to minimize hyperthermia, hypothermia should be targeted to between 32ºC and 36ºC for at least 24h after cardiac arrest (48, 49). The procedure should be completed within 72 hours of the event (24). Although the recommendations are standardized, their implementation at an institutional level can be complex for a variety of reasons, including inability to dedicate resources, staff lacking training with protocols, variability in clinical compliance with protocols, and variability in clinician knowledge about recent literature. Some centers use surface cooling because of costs or financial limitations, which may limit performance and outcomes (50).
Future direction and research requirements
According to the changing paradigm of targeted temperature management, further research should focus on personalized treatment approaches based on patient-related variables. Such individualized TTM regimens, relying on factors such as arrest etiology, initial neurological status, and comorbidity, could optimize the benefit-harm ratio through improved effectiveness and risk limitation (51). Improvement of patient selection using validated clinical decision tools is mandatory as part of the precision therapy of the post-recovery care. Promising emerging biomarkers, such as neuron-specific enolase (NSE), S100B, and glial fibrillary acidic protein (GFAP), are expected to facilitate the projection of neurological recovery and inform TTM responsiveness (52). Nevertheless, optimal timing, thresholds, and interpretation are still major research challenges (53). Advanced neuroimaging modalities, including diffusion-weighted MRI and functional connectivity mapping, provide critical information on cerebral injury patterns and prognostication. Such biomarkers might facilitate the early identification of patients who would derive benefit from TTM and thereby serve as an aid to more efficient decision-making (54). Ultimately, incorporation of TTM in the expanded setting of post-CA care, which should include adjustment of hemodynamics, treatment of seizures, and early mobilization, may eventually lead to enhanced outcomes. Prospective studies are required to assess the additive effect of post-recovery bundles (53). Large-scale, multicenter collaborative research, implemented within strong frameworks, will be essential to optimize TTM interventions and improve neurological outcomes following cardiac arrest.
Conclusion
TTM has been a standard therapy after post-cardiac arrest recovery, validated by extensive evidence of its ability to enhance neurological recovery among comatose survivors. In randomized trials and international guidelines, it was advocated that to reduce the impact of cerebral ischemia-reperfusion injury, the continuation of controlled hypothermia or normothermia has clinical benefit. Although there is some recent debate about the optimal temperature targets, the prevention of hyperthermia remains a universally accepted concept. Personalized treatment according to the clinical and prognostic characteristics of the patient and the resources available at the institution are important to achieve the optimal treatment benefits and minimize treatment-related risks. Ongoing studies of biomarkers, neuroimaging, and individualized strategies will further optimize the use of TTM. Strict compliance with recent guidelines and individualized care perspectives are crucial for enhancing long-term neurologic outcomes in cardiac arrest survivors
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Non-applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.