Volume 5, Issue 7
July 2025
The Role of Minimal Residual Disease (MRD) in Predicting Relapse in Acute Leukemia
Noor Adel Merwass, Yasser Abdulrhman Alnaeem, Zahra Malik Alsadiq, Walaa Saleh Alnakhlie, Ahmed Khaled Alhaifi, Esraa Saeed Bahttab, Rahaf Abdulmoniem Alhujili, Ibrahem Hamad Alwashmi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50711
Keywords: minimal residual disease, MRD, relapse, acute leukemia, acute lymphoblastic leukemia, ALL, acute myeloid leukemia, AML
Minimal residual disease (MRD) is a relatively newly established biomarker that enables clinicians to clinically assess and manage acute leukemia. Induction therapy eradicates leukemia cells in the peripheral blood; nonetheless, a considerable proportion of patients with acute lymphoblastic leukemia or acute myeloid leukemia persist in harboring leukemia cells that remain undetectable by standard microscopy. Real-time quantitative polymerase chain reaction, multiparameter flow cytometry, and next-generation sequencing are approaches utilized for assessing MRD. Although the declaration of MRD can vary depending on detection methodologies, MRD status has shown a significant association to relapse risk and overall survival, outperforming any standard risk factor. Evaluating MRD status at key timepoints (post-induction therapy, post-consolidation therapy, and pre-transplant) provides the basis for risk-adapted therapies, the timing of further consolidative therapies, and guiding decisions for hematopoietic stem cell transplant. Though many clinical centers routinely assess MRD status in the acute leukemia clinical setting, there are various challenges, such as variability between assays, technical aspects of certain MRD assessments, and no clear standard for MRD assessment and reporting. Despite these challenges, recent advancements in technology have improved performance and standardization of assays. recently, a number of clinical trials have involved MRD in supporting response-adapted treatment regimens. With an increased focus on genetic and immunologic risk both from MRD and other markers of disease response, MRD can guide us toward a more generalized approach to leukemia management. This review outlines the biological basis and clinical significance of MRD in the context of leukemia management and highlights the future innovations in MRD assessment.
Introduction
Acute leukemia is a type of blood malignancy that arises when undifferentiated blood cells multiply abnormally and rapidly. Acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) are aggressive hematologic malignancies that require prompt initiation of therapy—such as chemotherapy or hematopoietic stem cell transplantation (HSCT)—to prevent disease progression and improve the chance of remission (1). However, relapse is the main reason for treatment failure. Due to the limitations of morphologic assessment, more sensitive techniques for detecting minimal residual disease (MRD) are now essential for evaluating treatment efficacy in acute leukemia (2). There are various emerging methods that may be applied in the detection of this cell, including subsequent-generation DNA sequencing (NGS), real-time quantitative polymerase chain reactions (qPCR), and multiparameter flow cytometry (MFC) (3). Depending on the leukemia subtype and the applied approach, these techniques may identify leukemic cells in as low as 1 in 104 to 1 in 106 normal cells. Monitoring MRD enables the analysis of its development and the measurement of therapeutic efficacy. Additionally, this signifies the progression of residual leukemic cell amounts over time (4).
An expanding corpus of clinical research has demonstrated that the presence of MRD during or after therapy is a significant indicator of recurrence and worse survival outcomes. Consequently, MRD monitoring is necessary (5). MRD status has been identified as a more accurate predictor of recurrence than conventional risk factors, including cytogenetics and the initial white blood cell count. This renders MRD a superior diagnostic for risk stratification that is tailored to individual needs (6). In this context, MRD is not merely a method for predicting future events; additionally, it is a method for determining the appropriate course of treatment based on the severity of the condition at the time. The addition of MRD to therapy options is a component of a broader trend in cancer treatment that is moving toward more personalized care (2). According to MRD-guided procedures, physicians are permitted to modify their treatment strategies in accordance with the patient's response, rather than adhering to predetermined protocols (7). In the event that a patient tests positive for MRD after entering remission, they may require HSCT sooner if they are at high risk, or they may need to attempt alternative therapies such as immunotherapy or targeted therapy (8). In contrast, patients who were negative for MRD may be advised to reduce the intensity of their treatment in low-risk individuals. This approach would reduce toxicity without compromising efficacy. Despite the fact that these are positive developments, there are still some issues that must be resolved (9). For instance, there is no uniformity in the standardization of assays across institutions, the MRD levels employed to identify risk may differ, and the frequency and timing of assessments are unclear (10).
The purpose of this article is to compile available evidence on the potential of MRD to predict prognosis in acute leukemia. It examines the biological basis of residual disease, critically evaluates the methodologies used to detect MRD, and assesses their sensitivity, specificity, and clinical utility. The article also explores the integration of MRD assessment into treatment plans to improve outcomes and reduce the risk of relapse. By identifying gaps in the literature and consolidating existing knowledge, this review aims to enhance future clinical practice and research. Ultimately, the goal is to support the development of more personalized and effective care for individuals diagnosed with acute leukemia.
Methodology
A comprehensive literature search in the PubMed, Web of Science, ScienceDirect, and Cochrane databases on June 29, 2025. The search utilized medical topic headings (MeSH) and relevant keywords such as ‘minimal residual disease’, ‘MRD’, ‘relapse’, ‘acute leukemia’, ‘acute lymphoblastic leukemia’, ‘ALL’, ‘acute myeloid leukemia’, ‘AML’, and a combination of all available related terms. Peer-reviewed articles involving human subjects and available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, or participant age.
Discussion
Overview of acute Leukemia and relapse patterns
In both AML and ALL, hematopoietic progenitor cells have over-proliferation. Normal hematopoiesis results in uncontrolled over-proliferation or inability to enter apoptosis (11). In AML, the mutational events happen in myeloid progenitor cells (12). In ALL, the mutational events occur in lymphoid progenitor cells (13). The two general types of leukemia- AML and ALL- have specific cytogenetic and molecular aberrations (FLT3-ITD, NPM1; BCR-ABL1) that are relevant to risk stratification, diagnosis, and therapy (14). The first significant goal of therapy is complete remission (CR). CR is defined by the absence of morphologically detectable blasts in the bone marrow and evidence of hematopoietic recovery (15). There remain subclinical leukemic clones that may evade immune surveillance or are resistant to chemotherapy, and their subclones continue to promote relapse (16). The complexity of the relapse is complicated by MRD, which is the persistence of leukemic stem cells, more resistant to chemotherapy, within and around the blast and blast microenvironment. Relapsed disease is more chemo-resistant and has a worse prognostic outcome (17). Understanding the biology of relapse and using multiple competitive sensitive methods to track disease progression will be crucial to improving long-term outcomes and the development of MRD-guided, risk-adapted treatment strategies in acute leukemia, AML, and ALL in particular (18).
Definition and biological basis of MRD
Minimal residual disease refers to leukemic cells that persist at levels undetectable by conventional light microscopy. This level presumably represents a population of leukemic cells comprised of 5% or fewer blasts in the bone marrow (19). The assessment of MRD again utilizing sensitive measures like multiparameter flow cytometry, quantitative polymerase chain reaction (qPCR), or next-generation sequencing (NGS) describes the residual leukemic burden and can identify one leukemic cell in a background of as many as 104 to 106 normal cells (20). The biology of MRD utilizes the existence of one or more leukemic clones that are in some way resistant to treatment and may possess a specific genetic or epigenetic mark associated with the ability to evade the sterility of chemotherapy (21). Residual leukemic clones may contain stem-like properties which could include self-renewal and quiescence as mechanisms to resist agents that primarily work on rapidly dividing cells. The leukemic clones can also utilize the bona-fide marrow microenvironmental factors associated with the ability to evade the immune system and/or survive therapeutic clearance (22). Regarding MRD, the presence of this clearly suggested subclinical disease activity and serves as a reservoir for relapse. As such, MRD has become an important measure of therapeutic failure, accepted as a biologically and clinically meaningful surrogate for relapse prediction in patients with acute leukemia (3).
Techniques for MRD detection
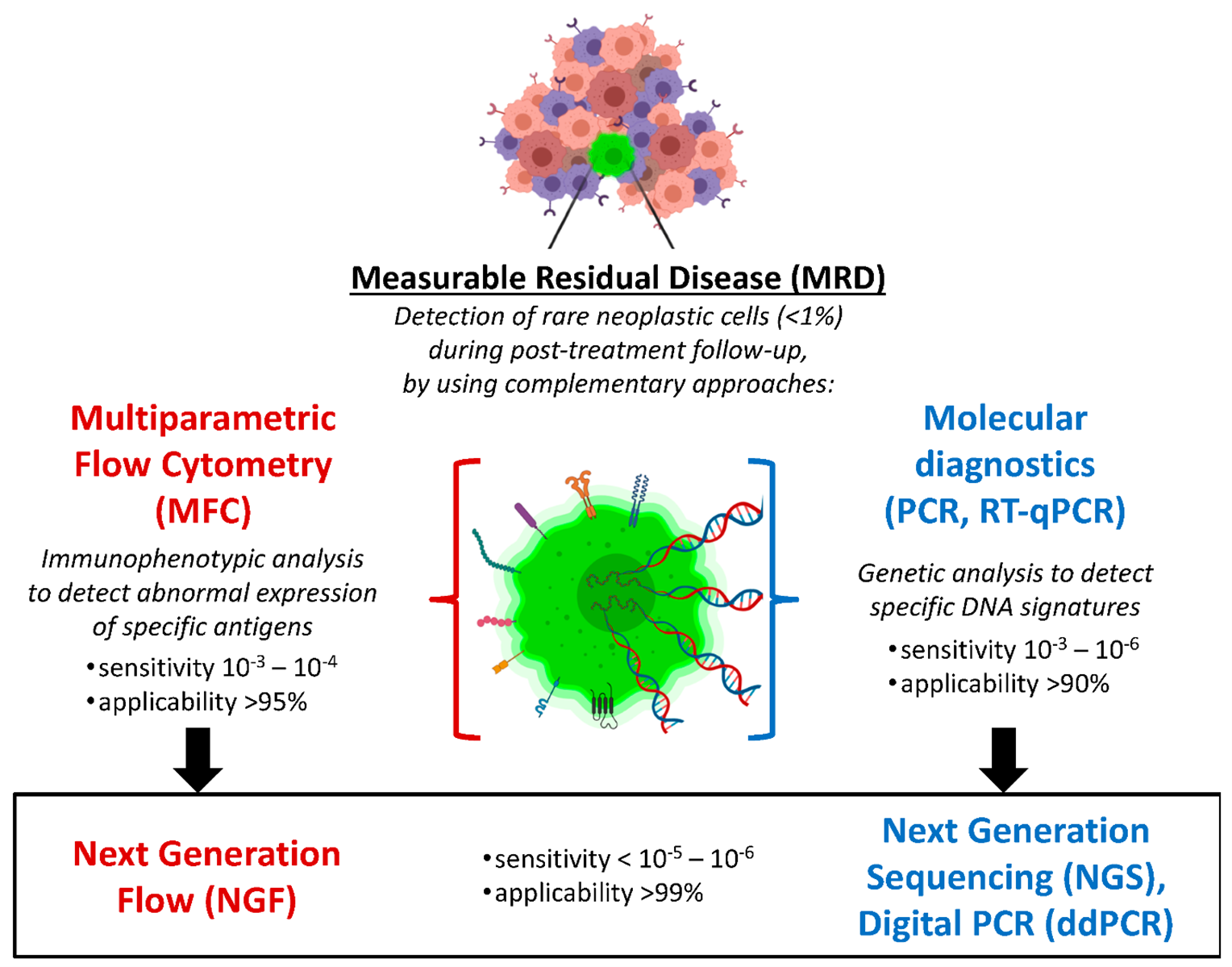
MRD detection in acute leukemia has transitioned from traditional morphology-based assessments to more sensitive molecular and immunophenotypic techniques (Figure 1). Pathology and hematopathology play crucial roles in this advancement, enabling more accurate prediction of relapses and guiding treatment strategies. The pathogenesis of acute leukemia involves the clonal proliferation of immature hematopoietic cells, leading to disruption of normal hematopoiesis (23). Even after achieving a CR in AML and ALL, residual leukemic cells can represent as the reservoir of disease relapse. Detection of MRD in acute leukemia primarily relies on ultra-sensitive methods capable of identifying leukemic cells beyond the limits of conventional morphology (Table 1) (24). Multiparameter flow cytometry (MFC) exploits differences in abnormal antigen expression to separate leukemic cells from normal hematopoietic cells (25). MFC is widely used for rapid MRD assessment with a sensitivity of 10-4; however, its reliability depends on the presence of a valid diagnostic immunophenotype and the technical proficiency of the operator (3). Accurate interpretation of MFC requires expert recognition of leukemia-associated immunophenotypes (LAIPs), especially in regenerating bone marrow post-chemotherapy, where reactive and malignant populations can overlap (26). Moreover, specimen quality—such as avoiding hemodilution or clot artifacts—can impact result reliability. Figure 2 illustrates how LAIPs are utilized in MFC to distinguish residual leukemic cells from normal regenerating marrow, highlighting the critical role of expert gating in precise MRD assessment.
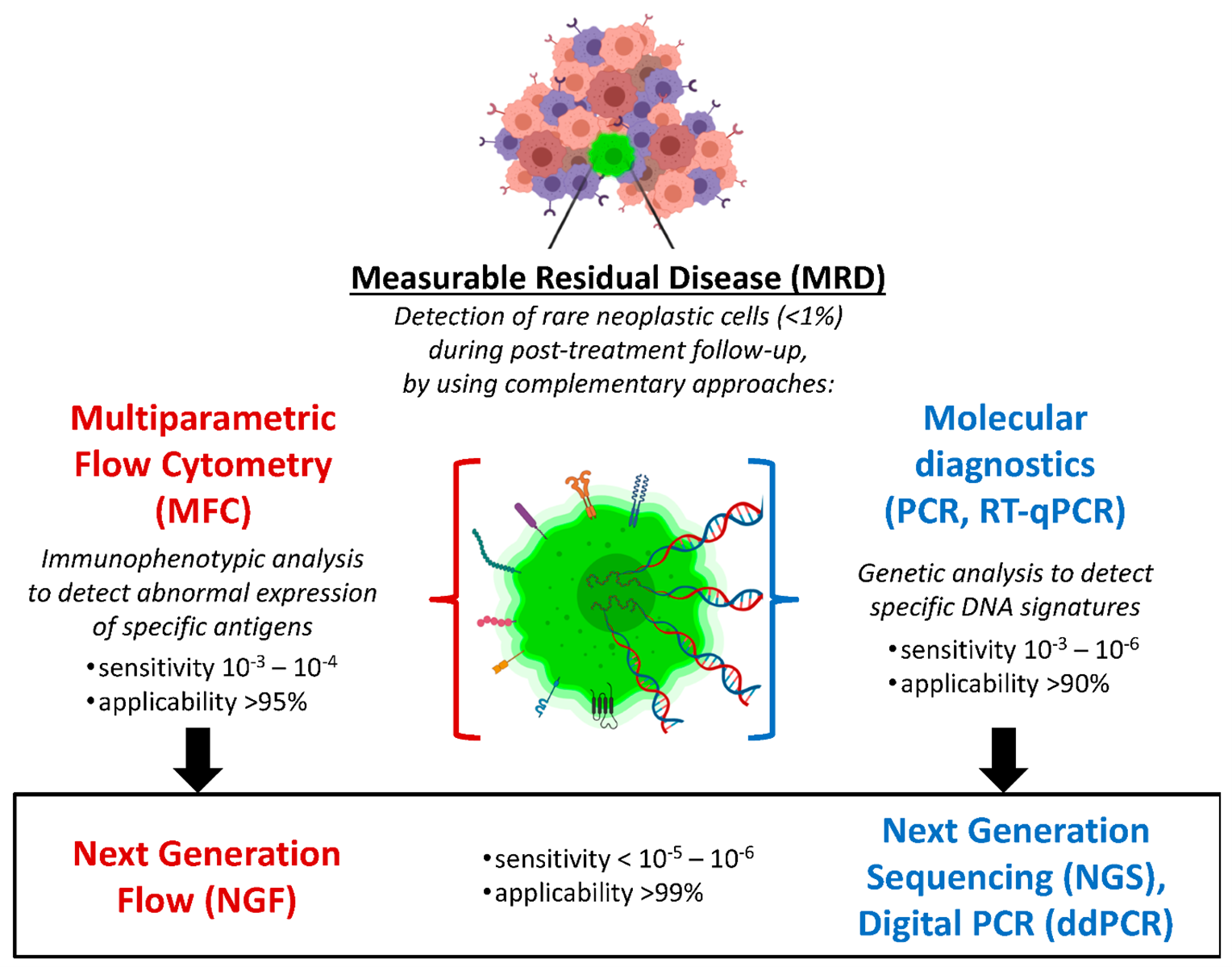
Figure 1: Overview of MRD detection techniques (27)
Real-time quantitative polymerase chain reaction (qPCR) employs leukemia-specific or rearranged fusion transcripts, for example BCR-ABL1 or RUNX1-RUNX1T1, which allows for identification or quantification of MRD to a sensitivity of 10-5. qPCR is applicable only to patients with a stable, known molecular target and cannot be used in the absence of such markers. Real-time qPCR requires standardized calibration against reference DNA and consistent input DNA quantities, with rigorous quality control across assays (29). The evolution and proliferation of next-generation sequencing (NGS) has more recently allowed for MRD monitoring through identification of a unique clonal rearrangement of immunoglobulin, or T-cell receptor genes in ALL, and recurrent mutations in AML (30). NGS has a sensitivity ~10-6 to MRD detection. NGS based MRD detection is transforming hematopathology by integrating molecular diagnostics with traditional hematological assessments. This approach allows for the tracking of clonal evolution and detection of residual leukemic cells at a single-cell level, offering a more sensitive and comprehensive evaluation of residual disease compared to older methods. This increased sensitivity is crucial for guiding treatment decisions and predicting patient outcomes (31). NGS offers broader clinical applicability and higher sensitivity compared to MFC or qPCR; however, its use is limited by high cost, longer turnaround times, and the need for specialized bioinformatics support (3). Each approach to MRD has advantages and limitations pertaining to sensitivity, specificity, clinical relevance, and standardization. All are important considerations in the choice of a context-specific MRD method for monitoring disease engagement (32).
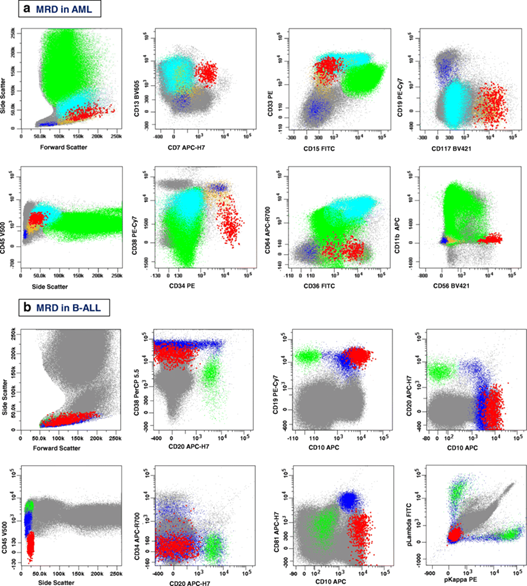
Figure 2: MCF plots illustrating MRD detection in (a) AML and (b) B-cell Acute Lymphoblastic Leukemia (B-ALL). Red dots represent leukemic cells exhibiting LAIPs, identified based on aberrant expression patterns of surface antigens compared to normal hematopoietic populations (gray, blue, green) (28)
|
Table 1. Diagnostic Techniques for Detecting MRD in Acute Lymphoblastic Leukemia (24) |
|||
|
TECHNIQUE |
PROS |
CONS |
SENSITIVITY |
|
MORPHOLOGY |
>5% Blasts |
Low sensitivity; not suitable for subclinical disease |
1% to 5% |
|
FISH |
Fast, no dividing cells required |
Labor intensive: low level of sensitivity especially with low cell counts |
0.3% to 5% |
|
PCR |
Limited to leukemias with available primers for common recurrent abnormalities |
High likelihood of false-positive results; expensive; applicable in only a subset of AML and ALL |
10-4 to 10-5 |
|
FC |
Applicable in ~80% of cases; cost effective; accurate for normal and abnormal cell types; rapid turnaround (1–2 days) |
Not as specific as PCR; phenotypic shifts post treatment or therapy; sub-populations of blasts |
10-4 |
FC: Flow Cytometry; FISH: Fluorescence In Situ Hybridization, PCR: Polymerase Chain Reaction, Morphology: Conventional Light Microscopy
Prognostic significance of MRD in acute lymphoblastic leukemia
Minimal residual disease has proved to be the best prognostic factor in ALL and has a considerable base of evidence in adults and children (33). MRD positivity after induction therapy and after continuation or consolidation is consistently an independent predictor of the risk of relapse and long-term survival in a number of clinical trials, including COG—Children's Oncology Group—and in several of the European ALL groups (34). In pediatric ALL, the MRD-negative status after induction has an event-free survival (EFS) of over 90% (35); similarly, in adult ALL, the MRD status is associated with a higher relapse rate and negative outcomes, according to the studies conducted by the United Kingdom ALL14 study and the GRAALL studies (36). In these studies, the patients with persistent MRD after induction, defined as <0.01% of leukemic cells, relapse will happen as an independent predictor of worse prognosis, and allogeneic stem cell transplant may be indicated for many MRD-positive patients (37). MRD has revolutionized the clinical decision-making and risk stratification process in therapeutic planning. MRD-negative patients could de-escalate their therapy and receive low-toxicity treatment, with no compromise in efficacy (38). For the MRD-positive patients, they can access more intensive regimens and emerging therapies available, such as immunotherapies with blinatumomab or CAR-T cells. Recently, MRD status and assessment are more than just prognostic markers; they are part of the personalized treatment option for ALL (39).
Prognostic significance of MRD in acute myeloid leukemia
Minimal residual disease clinical evaluation has grown in relevance and is now an important assessment in acute myeloid leukemia (AML) to provide further prognostic information after usual cytomorphologic and cytogenetic evaluation. MRD assessment in AML can be either molecular markers, for example, NPM1 mutants, RUNX1-RUNX1T1, CBFB-MYH11, or leukemia-associated immunophenotypes (LAIPs) from multiparameter flow cytometry (40). MRD assessment using molecular markers provides a sensitive measurement of the residual leukemic clones; however, multiparameter flow cytometry (MFC) is more sensitive than morphologic assessment, with sensitivity of 10-3 to 10-4; real-time quantitative PCR or next-generation sequencing (NGS) have even displayed sensitivity down to 10-6 for certain targets (3, 41). MRD positivity at the time of induction or consolidation therapy is a robust predictor of risk of relapse and poor overall survival (OS), regardless of baseline risk assignment (42). Apart from the findings of improved survival with MRD negativity, if the MRD is subtyped by MFC and/or an NPM1 mutation or other mutations, the equal value of MRD looks universal across combinations of cytogenetic and molecular aberrations observed in AML (e.g., CBF AML and NPM1-mutated AML) (43). MRD assessment can identify patients at high risk in the cytogenetically favorable subgroups who were assigned to low-risk groups based upon conventional risk assignment methods (44). Conversely, MRD negativity is associated with effective remissions and elevated survival rates; thus, MRD assessment provides an important variable in the decision-making regarding post-remission strategies (e.g., allogeneic stem cell transplant decision) (45). The integration of MRD assessment into treatment algorithms and treatment decision frameworks highlights the importance of MRD assessment in the individualized care and treatment of patients with AML (46).
Timing and frequency of MRD assessment
The timepoint for MRD evaluation and frequency of MRD monitoring plays a significant role in accurately quantifying treatment response and predicting relapses in acute leukemia. MRD assessment is mainly performed at established timepoints in treatment, including at specific therapeutic milestones, the post-induction, the post-consolidation, and the pre-transplantation phases (Figure 3) (47). Post-induction MRD represents an opportunity to determine early treatment responses and assess initial chemosensitivity. At this timepoint, if MRD is negative, it is highly associated with better long-term outcomes; conversely, if MRD is present, even at low thresholds, there is suboptimal disease-related response to treatment and a higher tendency for relapse (48). The post-consolidation MRD assessment continues to build off this prognostic assessment of potential treatment response. If disease is residual after multiple rounds of chemotherapy, this presents potential options for further intensifying therapy or proceeding to HSCT (49). Post-transplant MRD is more recognized as a significant determinant of success post-transplant. Patients who undergo HSCT in an MRD-negative and undetectable state have superior relapse-free and overall survival in comparison to patients with detectable MRD (50). The temporal dimension of MRD or MRD kinetics are uniquely available to monitor the evaluation of MRD changes. Generally, rapid decline in MRD indicates chemosensitivity; slower or static trends can indicate therapy resistance or evolution of clonal populations (51). The longitudinal nature of serial MRD assessments allows for complexity in risk stratification and real-time changes to treatment. For both practical and scientific reasons, proposed standards for timepoint definitions and tracking of longitudinal MRD assessments will be essential for the encompassing epitome of precision medicine for acute leukemia (52).
Figure 3: Role of Measurable Residual Disease at Different Timepoints of the Treatment Pathway in Acute Myleoid Leukemia (47).
MRD-guided treatment strategies
Minimal residual disease has become a cornerstone in risk-adjusted treatment approaches for acute leukemia, where one assesses the patient dynamically depending on disease burden over time rather than statically based on a patient’s initial baseline risk. MRD serves as a dynamic biomarker for treatment response, providing decision-making guidance beyond baseline risk stratification (53). The presence of MRD in patients early in their remission period allows treatment to be more safely de-escalated or maintained at a lesser intensity, thereby reducing the cumulative toxicity in a patient while not compromising clinical efficacy (54). MRD-positive patients are at higher risk of relapse and may require intensified chemotherapy, targeted therapy, or immunotherapy, including monoclonal antibodies or CAR T-cell therapy (55). MRD assessment is a critical factor in guiding decisions regarding HSCT. MRD-positive patients undergoing HSCT post- ALL and AML have significantly worse outcomes post-HSCT as they have been more likely to relapse in the post-transplant setting (56). Given this phenomenon, MRD provides important information on the timing of HSCT, conditioning regimen, and next steps after HSCT as it relates to the management of leukemia. MRD-directed maintenance therapy and monitoring are evolving, with significant enthusiasm surrounding ALL specifically (57). The ability to continue to monitor for MRD post-treatment will lead to earlier identification of molecular relapses, guiding the initiation of preemptive therapy. Overall, MRD-guided approaches do allow a personalization of therapy, with improved outcome performance and an exciting point of change in the management of acute leukemia (58).
Limitations and challenges in MRD implementation
Minimal residual disease (MRD) assessment in acute leukemia is associated with numerous limitations and difficulties with its implementation on a larger scale. Assays such as MFC, qPCR, and NGS differ in their targets, sensitivity, and specificity, and clinical variability may arise if methodologies or acquisition techniques are not standardized across trials (43). Assay variability and a lack of standardization across laboratories—particularly with MFC—can affect MRD interpretation due to differences in instrument calibration, reagent selection, and gating strategies. Technical and logistical barriers exist as factors contributing to the limited implementation of MRD into routine clinical practice (59). In certain AML or ALL subtypes, MRD assessment may be limited due to poorly characterized molecular or immunophenotypic markers. There are also challenges in determining clinically meaningful MRD thresholds and the optimal timing for intervention on an individual basis (60). These limitations will need to be addressed in order for MRD to be made available in a dependable, equitable, and standardized method in regard to its influence on the management of acute leukemia.
Future perspectives and research directions
Advances in precision oncology have positioned MRD detection as a key, multifaceted tool in acute leukemia management. Novel technological methods such as next-generation sequencing (NGS) and digital PCR have improved the sensitivity, specificity, and scalability of MRD detection. Today, we can access MRD detection with single-cell resolution, clonal tracking, and mutational tracking, thus providing more in-depth information about the persistence and evolution of the disease (61). Future advances will be focused on reducing time to result, cost, and access to MRD to allow its use on a broader scale in the clinics. Adding MRD to clinical trial design adds a critical factor for establishing the validity of MRD as a surrogate endpoint to longer-term endpoints such as relapse-free survival and overall survival (62). Real-time MRD detection could be considered a form of an adaptive biomarker during clinical trials, informing treatment changes in real-time, and can be used to personalize treatment protocols in real-time as well. Combining MRD with genomic, transcriptomic, and immunologic profiling may further refine risk stratification and guide targeted therapy (63). In the future we can anticipate standardized understanding of MRD-centric approaches to the management of acute leukemia.
Conclusion
Minimal residual disease has become an important part of management in acute leukemia due to its singular sensitivity in the detection of subclinical disease and prediction of relapse. The use of MRD in clinical practice enables ongoing risk stratification, evidence-based clinical decision-making, and personalized treatment regimens. Dedicated methods for MRD detection, including multiparameter flow cytometry, qPCR, and next-generation sequencing, all carry specific advantages for detecting MRD; however, limitations exist for assay standardization, accessibility, and interpretation. There is an emerging body of literature showing an effect for MRD in the context of risk stratification for hematopoietic stem cell transplantation, maintenance therapy, and early intervention. The next developments in MRD will focus on assay advances and the incorporation of MRD with genomic profiling. The standardized utilization of evidence-based MRD will be vital to optimize long-term outcomes and reduce or eliminate relapse for AML and ALL.
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Non-applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.