Volume 5, Issue 7
July 2025
The Role of Radiofrequency Ablation in the Management of Benign and Malignant Breast Lesions
Faisal Hasan Khadwardi, Amal Abdullah Albuqaisi, Mona Adel Almaqseed, Khairiah Yaqoub Alqashqari, Fahad Hussein Almalki, Meshaal Ibrahim Alenezi, Nejoud Faeq Alsharif, Yousef Ahmed Alghamdi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50716
Keywords: radiofrequency, radiofrequency ablation, RFA, benign lesions, malignant breast lesions, breast lesions, breast tumors
The management of breast lesions encompasses a comprehensive clinical spectrum ranging from benign tumors like fibroadenomas to early-stage breast cancer. Conventional treatments, including radiotherapy and surgical excision—continue to be fundamental, although they may cause major morbidity, cosmetic compromise, and psychological discomfort. Recently, there has been an increased interest in image-guided ablation techniques in minimally invasive, organ-preserving therapies. Radiofrequency ablation (RFA) has started to be a reasonable intervention for various breast lesions. Emphasizing its utility, clinical effectiveness, safety, and comparative advantages over other ablative techniques, this review aims to assess the role of RFA in controlling benign and malignant breast diseases. Specific attention is directed toward patient selection criteria, oncological results, aesthetic satisfaction, and modern imaging technology integration. Current studies, particularly in small and well-defined lesions, show that RFA is effective in obtaining high local control rates and patient satisfaction. Current studies, particularly in small and well-defined lesions, show that RFA is effective in obtaining high local control rates and patient satisfaction. Although long-term survival and recurrence data remain limited, RFA may be highly suitable for nonsurgical candidates with early-stage breast cancer. Although RFA has emerged as a promising technique, its integration into clinical practice requires further validation through cost-effectiveness studies and randomized controlled trials. The results support RFA's prospective application in enhancing customized, minimally invasive intervention for breast lesions.
Introduction
Benign and malignant forms of breast lesions constitute a major issue in women's health globally. Malignant lesions, particularly breast carcinomas, are the most commonly diagnosed cancers among women worldwide. Primarily breast carcinomas and benign lesions, including fibroadenomas, cysts, and papillomas are common, especially in premenopausal women (1, 2). Based on GLOBOCAN 2020 figures showing almost 2.3 million new cases and 665,000 deaths yearly, breast cancer is obviously crucial for public health (3). Although benign breast tumors commonly lack malignant potential, their treatment is required for related symptoms, cancer-related anxiety, or cosmetic issues. Standard treatment modalities—ranging from observation to surgical excision—are commonly used but may result in physical morbidity, scars, psychological suffering, and financial consequences for healthcare (4). Investigating minimally invasive treatments that provide efficient treatment with fewer complications and improved aesthetic results has thus attracted more interest (5).
Surgery has consistently been regarded as the fundamental approach for both benign and malignant breast lesion treatment. Common operations in malignant cases are lumpectomy and mastectomy, often accompanied by radiation or systemic treatments. Although these procedures are effective, they carry operational disadvantages, long recovery times, and, in many cases, unsatisfactory cosmetic outcomes (6). For benign lesions—particularly those that are growing or symptomatic—core needle biopsy or vacuum-assisted excision is commonly employed (7). Nevertheless, in both benign and malignant breast tumors, careful patient selection and adherence to procedural protocols are essential to minimize risks and ensure therapeutic efficacy. Recently, several reduced invasive image-guided ablation techniques have become available as appropriate interventions. Radiofrequency ablation (RFA) had a growing interest among the other techniques. By using high frequency alternating electrical currents, RFA produces thermal coagulation necrosis in specific tissues (8). Already confirmed in pulmonary, renal, and hepatic neoplasms, it has shown safety, accuracy, and effectiveness in the management of benign and malignant breast lesions (9). Regarding local management, aesthetic preservation, and patient satisfaction concerning the use of RFA in breast lesions—both benign and malignant cases—limited studies and early clinical trials have shown promising outcomes (2).
Although the preliminary findings for RFA demonstrate therapeutic potential, its role in standard clinical treatment for breast tumors remain unclear. Recent literature consists of single-center studies with limited sample sizes, limited follow-up periods, and various approaches. Regarding recurrence rates, survival outcomes, and histological changes following RFA in malignant cases, the long-term oncological data is insufficient (10). The evidence for benign lesions is mainly anecdotal or observational; randomized comparisons with surgical or vacuum-assisted techniques are unavailable (11). Furthermore, protocols from well-known surgical and oncology groups have not yet included RFA in accepted treatment strategies for breast lesions, suggesting the need for more comprehensive, controlled research (12).
Regarding the worldwide incidence of breast disease and the limitations of conventional surgical techniques, there is a compelling case for extending the database on RFA. Particularly for patients who are not candidates for surgery or those seeking breast conservation without scarring, its reduced invasive qualities, fit for outpatient operations, and pleasing aesthetic results appeal (13). Within a multidisciplinary therapeutic framework, especially in certain early-stage or inoperable cases, RFA may either augment or maybe replace surgery in malignancies (14). Valuation of RFA in both benign and malignant breast tumors is vital as healthcare increasingly emphasizes tailored and patient-centered treatment approaches (15). Comparative research, cost-effective analysis, and region-specific evaluations will improve practice recommendations.
This article aims to compile current data regarding the use of RFA in the treatment of benign and malignant breast lesions. Evaluating its clinical efficacy, safety, and patient outcomes across various lesion types and identifying the flaws in existing techniques, the comparison of RFA with alternative ablative and conventional therapies and pinpointing the areas that require further investigation. This review attempts to ascertain whether RFA is a reasonable therapeutic choice in emerging breast lesion management.
Methodology
A comprehensive literature search was conducted in PubMed, Web of Science, ScienceDirect, and Cochrane databases on March 25, 2025. The search utilized medical topic headings (MeSH) and relevant keywords such as ‘radiofrequency’, ‘radiofrequency ablation’, ‘RFA’, ‘benign lesions’, ‘malignant breast lesions’, ‘breast lesions’, ‘breast tumors’, and a combination of all available related terms. Peer-reviewed articles involving human subjects and available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, or participant age.
Discussion
Principle of radiofrequency ablation
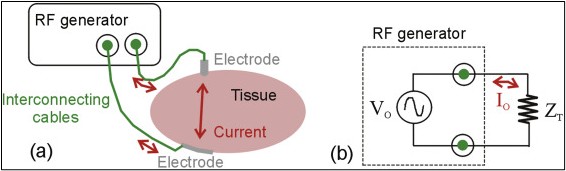
RFA is a percutaneous, image-guided technique that uses a targeted application of high-frequency alternating electrical current to thermally eliminate target tissue (16). The radiofrequency current, usually in the range of 300 to 500 kHz, is delivered directly from the electrode into the targeted lesion (17). The resulting ionic disturbance within the tissue generates frictional heat (Figure 1) (18), which raises temperatures to 60–100°C and causes coagulative necrosis (19). Tissue impedance, lesion size, electrode placement, and application timing all affect the degree of ablation. The traditional RFA arrangement calls for a radiofrequency generator, grounding pads to create the electrical circuit, and a probe or electrode with temperature-monitoring capabilities (20). The use of internally cooled or multi-tined expandable electrodes is commonly employed to improve energy distribution and prevent charring, thus hindering energy transfer. Usually performed under local anesthetic or awake sedation, the treatment increases patient comfort and reduces perioperative risk (21). Precise aiming and real-time observation rely on image guidance. Because of its accessibility, economy, and ability to provide real-time feedback, high-resolution ultrasonic waves are the recommended modality for superficial breast lesions (22). Magnetic resonance imaging (MRI) provides improved contrast resolution and multiplanar capabilities in cases of insufficiently visible lesions or dense parenchyma, thus allowing correct electrode placement and post-ablation evaluation (23). RFA in breast applications generally demonstrates a favorable safety profile, with most adverse effects being minor and self-limiting (2). Regular consequences include localized pain, skin erythema, hematoma, and transient edema. When the optimal technique and imaging direction are applied, severe negative effects—including skin burns, infections, or damage to surrounding structures—are rare (24). RFA removes surgical scars and preserves breast form, thereby enhancing cosmetic outcomes. However, in benign and malignant breast tumors, careful patient choice and adherence to procedural recommendations are crucial to reduce risks and guarantee therapeutic efficacy (25).
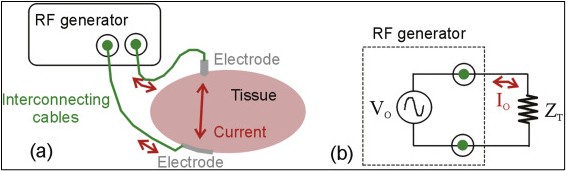
Figure 1: Radiofrequency Ablation (18).
RFA in benign breast lesions
RFA has emerged as a reasonable substitute for surgical excision. Particularly in the treatment of benign breast lesions such as fibroadenomas. Indications for RFA generally include symptomatic lesions, progressive growth, cosmetic concerns, or patient anxiety—particularly in individuals seeking to avoid surgery (26). Ideal candidates have precisely defined, ultrasonically detectable tumors of less than 3 cm along with histological evidence of benignity obtained through core needle biopsy. Typically eliminated are lesions showing atypical imaging features or ambiguous pathology since RFA cannot produce tissue for further examination (27). RFA has shown significant effectiveness in clinical studies in reducing lesion volume and thus decreasing symptoms (28). In most cases, a volume reduction of over 80% is observed within 6 to 12 months post-procedure, significant volumetric reduction has been repeatedly recorded (29). Although the procedure may be time-consuming, complete resolution occurs through gradual resorption of necrotic tissue. The procedure’s reduced recuperation requirements are shown by most patients attaining pain relief within weeks and most starting regular activities within the first week (30). Although RFA reduces the morbidity linked to open surgery, it offers comparable clinical outcomes to surgical excision. Excision carries risks of scarring, anesthesia-related issues, and changes in breast form even if it provides rapid lesion removal and histological confirmation (31). Conversely, RFA reduces the need for conventional sutures and incisions, thus enhancing cosmetic preservation. Imaging follow-up following RFA confirms lesion regression, thus negating the need for surgical pathology in the appropriate cases (32). High patient satisfaction with RFA can be ascribed to its non-invasive properties, outpatient applicability, and preservation of breast aesthetics. Reports indicate high acceptance among young females and those with bilateral or numerous lesions, for whom repeated surgery would involve more risk (33). For the treatment of benign breast lesions, RFA thus represents a clinically efficient, aesthetically pleasing, and patient-oriented technique.
RFA in malignant breast lesions
RFA has attracted significant research as a minimally invasive alternative to surgery, in cases of early-stage breast cancer. Given no clinical or radiologic lymph node involvement, current data indicates that RFA can be safely used in patients with unifocal, estrogen receptor-positive, and HER2-negative tumors measuring ≤ 2 cm (34). These criteria point to a subpopulation of breast cancer marked by positive biological behavior and reduced spreading potential; hence local ablative treatment becomes a realistic choice (2). Confirmation of invasive cancer through image-guided biopsy is essential prior to performing RFA; axillary assessment is generally conducted as a separate procedure. Promising oncological outcomes have come from clinical trials and observational research (35). In most studies, local control rates exceed 90% and are combined with low in-field recurrence rates over short to medium terms (36). Notably, survival data have not shown inferiority for RFA in appropriately selected patients. Most studies are non-randomized, involve limited cohorts, and lack long-term follow-up, thus limiting significant results on long-term survival and recurrence risk (37). Furthermore, lacking a surgical specimen, RFA prevents pathological evaluation of tumor margins, lymphovascular invasion, and other prognostic factors. In an oncological safety assessment, this represents a clear limit (38). Concerns include ineffective ablation in tumors with uneven margins or significant ductal components in addition to challenges interpreting post-ablation imaging (39). Although the consistency of follow-up methods varies among studies, magnetic resonance imaging (MRI) has shown significant success in assessing therapy response (40). Notwithstanding these limitations, RFA could provide major benefits to high-risk groups, including elderly people, those with major comorbidities, or patients who refuse surgical intervention. In these cases, RFA provides a low-morbidity solution that preserves breast architecture and guarantees local tumor control. Particularly concerning tailored, minimally invasive therapeutic approaches, current studies aim to clarify the role of RFA in oncological procedures (2).
Comparative analysis with other ablative techniques
RFA is one of several image-guided thermal ablation methods being evaluated for the treatment of breast lesions. In both benign and malignant breast cancer, alternative approaches, including cryoablation, microwave ablation, and high-intensity focused ultrasonic (HIFU), have shown varied degrees of clinical efficacy, safety, and feasibility (41). Cryoablation causes cell death by ice crystal development and ischemia by alternately rapidly freezing and thawing tissue (Figure 2) (42).
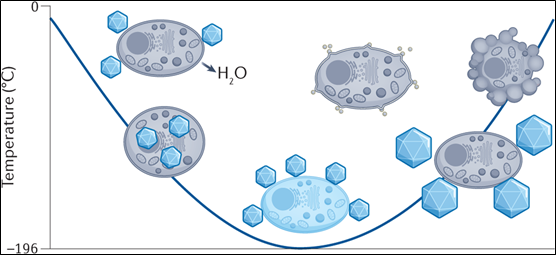
Figure 2: Chemical Approaches to Cryopreservation (42).
It provides real-time vision of the ice ball under ultrasonic direction, thus enabling exact control and less damage to surrounding tissues (43). Typically, well tolerated, cryoablation does not elicit pain during treatment since cold naturally has analgesic effects. Nevertheless, lesion size reduction occurs gradually, and the efficacy of this approach for poorly defined or irregular tumors is still being evaluated (44). Unlike RFA, microwave ablation generates higher intratumoral temperatures (>100°C) in a shorter period by exciting water molecules. It may be applied to treat significant or denser lesions; it accelerates ablation with higher coagulation volumes. However, rapid heating increases the possibility of uncontrolled thermal diffusion and adjacent tissue damage, which calls for careful control and experienced practitioners. Without penetrating the skin, the non-invasive (45), extracorporeal HIFU concentrates ultrasonic waves to thermally ablate tissue. Notwithstanding its appeal, the use of HIFU is limited by long-term process, motion sensitivity, and dependence on specific acoustic characteristics of tissues, thus compromising accuracy and dependability (46). RFA provides a comprehensive profile of efficacy, safety, and accessibility comparable to these modalities. In addition to its low cost and proven approach, its interoperability with conventional ultrasonic devices makes it essentially feasible. However, there are disadvantages, including limited previous studies of tissue and the possibility of partial ablation in heterogeneous tumors. Therefore, the choice of the most appropriate technique should consider lesion features, clinical background, and available institutional resources (47).
Challenges and limitations
Although there is a growing interest in RFA for breast lesion treatment, numerous factors prevent its general clinical acceptance. However, RFA is the most effective technique in the management of small, well-defined lesions less than 3 cm. Lesions above this size could call for repeated overlapping ablations, thus increasing procedural complexity and the risk of incomplete necrosis (48). The location of the tumor significantly influences feasibility; lesions adjacent to important structures like the epidermis, pectoral fascia, or nipple-areolar complex cause hazards of thermal damage and cosmetic disfigurement, thus careful planning and operator expertise are essential (49). One significant limitation is the lack of long-term oncological outcome data. The majority of the current studies are retroactive, depend on limited patient populations, and provide limited follow-up durations, typically less than five years. However, unresolved are the longevity of tumor control, recurrence patterns, and how they affect disease-specific and general survival (50). Currently, RFA does not serve as a substitute for standard surgical guidelines of early-stage breast cancer therapy in the lack of significant data from randomized controlled trials. RFA for malignant breast lesions has remained regarded in many countries as exploratory and calls for strict informed permission and ethical supervision. Particularly in infiltrative tumors, the absence of surgical specimens following RFA causes concerns about margin status and possible under-treatment, thus affecting thorough histological assessment (51). From a health economics perspective, RFA's cost-effectiveness is yet unknown in a comprehensive evaluation (52). The need for enhanced imaging, specialized equipment, and trained staff may diminish this technique’s cost even if it might shorten hospitalization length and postoperative recovery costs. Moreover, follow-up treatments and repeated imaging could help to explain total healthcare expenses (53). Establishing the clear position of RFA in the modern management of benign and malignant breast tumors will depend critically on standardized protocols, improved imaging techniques, and prospective multicenter trials mitigating these constraints (54).
Future directions and recommendations
The application of RFA in the management of breast lesions is significantly correlated to current clinical studies, assessment of precision medicine, and technological advancements. To evaluate the long-term oncological efficacy, safety, and aesthetic results of RFA in benign and early-stage malignant breast lesions, numerous multicenter trials and prospective studies are needed. These studies must aim to generate strong data on local recurrence, recurrence-free survival, and patient-reported quality-of-life outcomes—all of which are vital for RFA validation as a standard treatment option. One development is the use of RFA with high-resolution imaging methods. Improvements in contrast-enhanced ultrasonography, elastography, and magnetic resonance thermometry enable accurate lesion characterization, real-time procedural control, and post-ablation assessment. These imaging techniques reduce residual disease risk, allow early identification of incomplete ablation areas, and increase procedural accuracy (55). Furthermore, by using the heat-sensitive release of therapeutic drugs within the ablation zone, the combination of RFA with focused drug delivery techniques—such as thermo-sensitive liposomal chemotherapy—may improve local tumor control (56). Regarding tailored medicine, RFA is significantly promising. Through molecular analysis of breast tumors, patients with favorable biological subtypes—such as low-grade carcinomas driven by hormones—who might benefit from non-surgical ablation can be identified (57). RFA may be included in tailored treatment algorithms in future approaches whereby ablative therapy is customized depending on tumor biology, patient comorbidity profiles, and personal preferences (58). Moreover, the combination of RFA with additional systemic therapy—such as endocrine or immune-modulating medications—may contribute to the control of local and systemic diseases while reducing treatment-related morbidity (59). These guidelines point to a move toward minimally invasive, patient-centered treatments. Through continuous research and multidisciplinary cooperation, RFA could evolve into a validated and customized tool for treating benign lesions and controlling breast cancer.
Conclusion
In the treatment of particular benign and early-stage malignant breast lesions, RFA shows significant efficiency and safety. Particularly in patients considered as non-candidates for surgery, evidence supports its effectiveness in achieving high local control rates along with enhanced esthetic outcomes. RFA provides harmonic features such as accuracy, availability, and procedural efficiency in comparison to other ablative techniques. However, there are ongoing concerns about tumor size, long-term oncological outcomes, and the lack of histological samples. Clinically, especially within minimally invasive and customized therapeutic frameworks, RFA may serve as an alternative or complement to conventional surgery in specific cases. Its future performance is enhanced by its combination of tailored therapies and advanced imaging. To support RFA as a conventional therapeutic modality in the management of breast lesions, future studies should apply randomized controlled trials, standardized imaging technologies, and cost-effectiveness analyses.
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Non-applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.