Volume 5, Issue 8
August 2025
Assessment of Prevalence and Risk Factors Associated with Central Line-Associated Bloodstream Infection (CLABSI) in Hemodialysis Patients at King Fahd Armed Forces Hospital Renal Dialysis Center in Jeddah: A Retrospective Cross-Sectional Study
Ahlam Abdulrahman Alghamdi, Raghdh Mohammed Battarjee, Khalid Abdullah Almotairy, Wejdan Saleh Basudan, Mashael Abdulaziz Alkhuli, Rabab MohammedAmeen AlMojalled, Roqaya Moeedh Aljoaid, Kholod Samer Shopain
DOI: http://dx.doi.org/10.52533/JOHS.2025.50803
Keywords: Central Line-Associated Bloodstream Infection, CLABSI, Hemodialysis,Saudi Arabia, King Fahad Armed Forces Hospital
Introduction: Hemodialysis patients often contend with multiple co-morbidities, weakened immune systems, and prolonged hospital stays, factors that heighten their vulnerability to healthcare-associated infections, specifically Central Line-Associated Bloodstream Infection (CLABSI). CLABSI is a severe and potentially life-threatening infection that occurs when bacteria or other microorganisms enter the bloodstream through a central line or central venous catheter. This retrospective cross-sectional study aims to delve into the prevalence and identify the risk factors associated with CLABSI among hemodialysis patients at the King Fahad Armed Forces Hospital Renal Dialysis Center in Jeddah.
Methods: This retrospective cross-sectional study utilized a non-interventional approach and data from the electronic medical records system were collected. The study spanned from January 2022 to April 2023. The target population comprised adults undergoing renal replacement therapy via hemodialysis at the hospital. Encompassing the entire population of eligible adult hemodialysis patients during the specified timeframe ensured a comprehensive analysis of this specific target group.
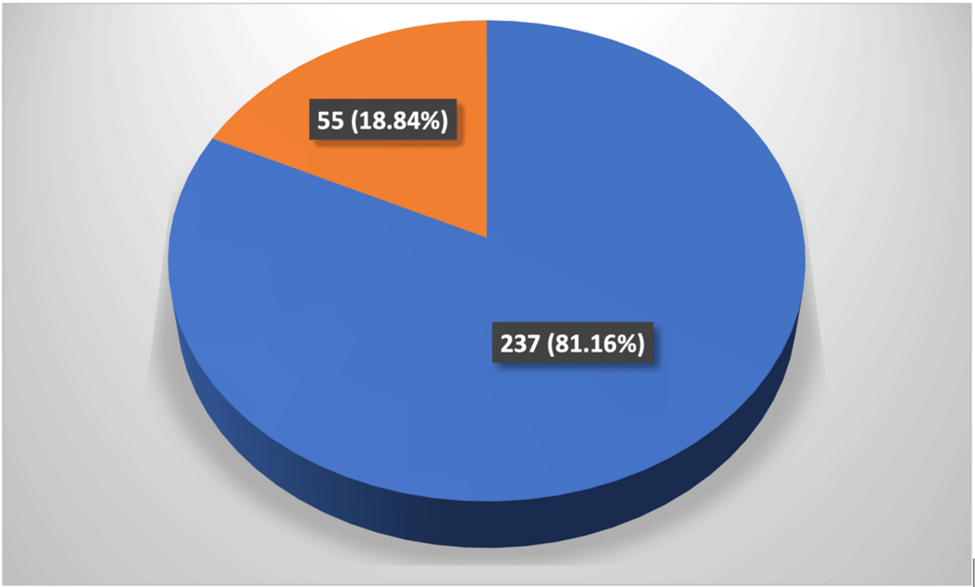
Results: Among the 292 dialysis patients included in the study, 55 developed CLABSI, resulting in an overall prevalence of 18.84%. Notably, the highest number of cases occurred in June 2022 with 10 cases (18.2%), followed by August 2022 with 8 cases (14.5%), with March 2023 showing the lowest incidence of only 1 case (1.8%). Pseudomonas aeruginosa was the most prevalent microorganism among CLABSI patients, accounting for 10 cases (18.2%), while Staphylococcus aureus ranked second, detected in 7 cases (12.7%). No statistically significant association was found between the type of microorganism and gender.
Conclusion: These findings emphasize the importance of identifying the prevalence and risk factors of CLABSI to enhance patient outcomes and care quality. Looking ahead, sustained efforts in quality improvement, vigilant monitoring, and a dedication to antimicrobial stewardship are pivotal to reducing CLABSI rates and advancing the overall standard of care for hemodialysis patients.
Introduction
Hospital-acquired infections (HAIs) are infections that usually develop with symptoms after a stay at a hospital or healthcare facility and were not present in the patient’s system at the time of admission. They are usually associated with increased medical expenses, prolonged stay at the hospital, and compromised quality of life (1). Globally, almost 5%-10% of the total hospitalized patients end up developing HAIs, which is now a major patient safety concern around the world (2).
Hemodialysis is a critical and complicated medical procedure, essentially provided to patients with end-stage renal disease (ESRD). To facilitate the removal of waste products and excess fluids during hemodialysis, a vascular access point is established. Common vascular access points for hemodialysis are central venous catheters (CVC), arteriovenous fistulas (AVF), or arteriovenous grafts (AVG) (3). Hemodialysis patients are often burdened with multiple co-morbidities, weak immune systems, and prolonged hospital stays, which eventually increases their susceptibility to HAIs, such as Central Line-Associated Bloodstream Infection (CLABSI). It is a serious and potentially life-threatening healthcare-associated infection that occurs when bacteria or other pathogens enter the bloodstream through a central line (CL) or central venous catheter. CLABSI can result from contamination of the catheter during insertion, use, or maintenance. Prolonged placement of the CL is associated with a considerably higher risk of infection. The infection can lead to severe complications, including sepsis, and it requires prompt diagnosis and treatment (4).
Annually, in the United States, about 250,000 individuals suffer from CLABSI (5). Due to longer hospital stays, higher antibiotic costs, and higher medical expenses, every incident is expected to cost the hospital as much as $46,685 (6). Moreover, poor compliance with protocols and a higher prevalence of CLABSI in hemodialysis patients was also observed in the United States (7). Alarming rates of CLABSI in Asian countries, specifically low-middle-income countries were also highlighted in a study. The general CLABSI rate per 1000 CL days was 5.08, out of which the highest rate of 6.23 was estimated to be in the femoral catheter (8).
Various risk factors contribute to the occurrence of CLABSI. These include patient age, underlying conditions like diabetes, kidney disease, or hypertension, a prior history of catheter-related infections, and factors related to catheter use, such as placement site, type, duration, and number. Other influences include the length of dialysis, specific blood markers (e.g., albumin, C-reactive protein, hemoglobin, CD4+ cells, prolacitonin), poor hygiene practices, and the APACHE II score (9).
Hemodialysis, a critical life-sustaining therapy for individuals with renal insufficiency, often necessitates the use of central venous catheters to facilitate vascular access. The prevalence of CLABSI remains a significant concern in this patient population. This retrospective cross-sectional study aims to investigate the prevalence and identify the risk factors associated with CLABSI among hemodialysis patients at the King Fahad Armed Forces Hospital Renal Dialysis Center in Jeddah.
Materials & Methods
Study design and duration
The study was conducted retrospectively as cross-sectional research and employed a non-interventional approach. The study period spanned from January 2022 to April 2023.
Study setting and population
The study took place at the renal dialysis center of King Fahad Armed Forces Hospital in Jeddah, a large tertiary care hospital with a 420 inpatient bed capacity. The target population consisted of adults, who were receiving renal replacement therapy through hemodialysis at the King Fahad Armed Forces Hospital during the study period of 16 months.
Inclusion and exclusion criteria
All the patients who were adults and had a CL placed for their hemodialysis treatment were considered eligible for this study. These participants eventually get an arteriovenous access placed during the study. However, patients who had incomplete medical records, or were not on regular follow-ups at the King Fahad Armed Forces Hospital for their hemodialysis were excluded.
Sample size calculation
Since the study was conducted retrospectively, it was decided to include all the eligible cases available in the medical records system, eliminating the need for a traditional sample size calculation. The study encompassed the entire population of adult HD patients meeting the inclusion criteria during the specified timeframe, ensuring a comprehensive analysis of this specific targeted population.
Data Collection
The data for this study was exclusively collected from the patient list of those who underwent hemodialysis during the study period and subsequently developed CLABSI. The information was acquired from the hospital’s database after obtaining all the necessary permissions.
Statistical Analysis
The data, sourced from medical records at the King Fahad Armed Forces Hospital Renal Dialysis Centre, were entered into an Excel spreadsheet and analyzed using IBM SPSS Statistics 26. This dataset encompassed patient gender, duration of dialysis, and identified microorganisms. Chi-square and Fisher's exact tests were utilized to explore the relationship between CLABSI and gender, as well as each microorganism with gender. The study specifically focused on patients who developed CLABSI, examining the frequency (measured in months) and the types of microorganisms involved.
Ethical Statement
The study was approved by The Research Ethics Committee of Armed Forces Hospitals-Jeddah with approval number: REC 667. An informed consent was provided by the patients to include the data anonymously.
Results
The study included 292 dialysis patients with central line catheters placed for durations ranging from 4 to 12 months. The catheter placement locations varied based on individual patient needs (internal jugular, subclavian or femoral). The type of catheter also varied depending on the patient (tunneled or non-tunneled). And samples for bacterial growth were taken from the catheter every month. Among these 292 patients, 55 developed CLABSI, resulting in an overall prevalence of 18.84% (Figure 1).
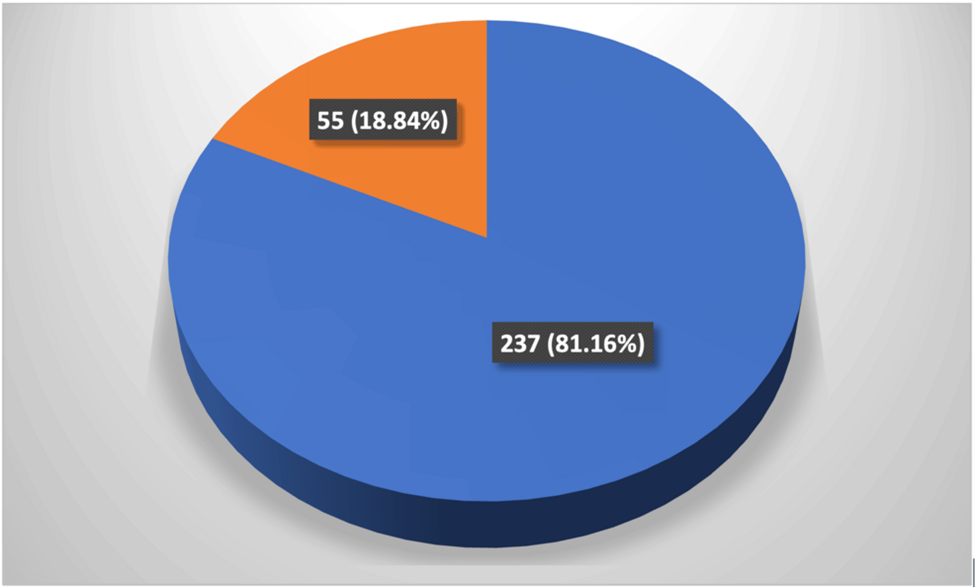
Figure 1: Distribution of CLABSI in 292 hemodialysis patients. Orange: CLABSI, Blue: No CLABSI
Demographic characteristics of patients who developed CLABSI, with a total sample size of 55 patients, are presented in Table 1.
|
Table 1: Demographic characteristics of CLABSI-developed patients |
|
|
Variables |
Frequency (%) n=55 |
|
Gender* |
|
|
Female |
22 (40) |
|
Male |
31 (56.4) |
|
Months |
|
|
January-2022 |
4 (7.3) |
|
February-2022 |
1 (1.8) |
|
March-2022 |
4 (7.3) |
|
April-2022 |
2 (3.6) |
|
May-2022 |
5 (9.1) |
|
June-2022 |
10 (18.2) |
|
July-2022 |
5 (9.1) |
|
August-2022 |
8 (14.5) |
|
September-2022 |
6 (10.9) |
|
October-2022 |
6 (10.9) |
|
November-2022 |
3 (5.5) |
|
March-2023 |
1 (1.8) |
*Two cases had missing gender details
Among the CLABSI-developed patients, a slight male predominance (56.4%) in comparison to the female population (40%) was observed. Additionally, the trend of CLABSI cases in different months was noted. The highest number of cases occurred in June 2022 (18.2%), followed by August 2022 (14.5%). February 2022 and March 2023 had the lowest number of cases (1.8%). It appears that CLABSI cases varied across the months, with some months having higher incidence rates than others which may be attributed to the increased bacterial growth and presence during different seasons.
The most prevalent microorganism among CLABSI patients was Pseudomonas aeruginosa, accounting for 18.2% of the cases. This was followed by Staphylococcus aureus, detected in 12.7% of cases, and Klebsiella pneumoniae, present in 9.1% of cases. Other notable microorganisms included Serratia marcescens and Escherichia coli, each identified in 7.3% of cases, and Proteus mirabilis, which accounted for 5.5%. Less frequently identified microorganisms included Methicillin-Resistant Staphylococcus Aureus (MRSA) (3.6%), Enterobacter aerogenes (3.6%), and Enterobacter cloacae, Citrobacter freundii, Enterococcus faecium, Acinetobacter baumannii, Staphylococcus epidermidis, and Morganella morganii, each representing 1.8% of cases (Table 2).
|
Table 2: Frequency distribution of microorganisms in CLABSI patients |
|
|
Microorganisms |
Frequency (%) |
|
Pseudomonas aeruginosa |
10 (18.2) |
|
Staphyloccocus aureus |
7 (12.7) |
|
Klebsiella pneumonia |
5 (9.1) |
|
Serratia marcescens |
4 (7.3) |
|
Escherichia coli |
4 (7.3) |
|
Proteus mirabilis |
3 (5.5) |
|
Methicillin-Resistant Staphylococcus Aureus |
2 (3.6) |
|
Enterobacter aerogenes |
2 (3.6) |
|
Enterobacter cloacae |
1 (1.8) |
|
Citrobacter freundii |
1 (1.8) |
|
Enterococcus faecium |
1 (1.8) |
|
Acinetobacter baumanii |
1 (1.8) |
|
Staphylococcus epidermidis |
1 (1.8) |
|
Morganella morgani |
1 (1.8) |
Among females, 16.58% had CLABSI while among males, 21.36% had CLABSI (Table 3). However, the p-value associated with this comparison is 0.313, indicating that there is no statistically significant difference in CLABSI incidence between genders.
|
Table 3: Comparison of CLABSI with gender |
|||
|
Female N (%) |
Male N (%) |
P value |
|
|
CLABSI |
|||
|
Yes |
31 (16.58) |
22 (21.36) |
0.313 |
|
No |
156 (83.42) |
81 (78.64) |
|
CLABSI: Central Line-Associated Bloodstream Infection; P value: Fishers Exact test
The analysis indicates that across various microorganisms, including Pseudomonas aeruginosa, Klebsiella pneumoniae, Serratia marcescens, Escherichia coli, Methicillin-Resistant Staphylococcus Aureus, Proteus mirabilis, Enterobacter cloacae, Enterobacter aerogenes, Citrobacter freundii, Enterococcus faecium, Acinetobacter baumannii, and Staphylococcus epidermidis, no statistically significant association exists with gender based on their occurrence. Most of these microorganisms show comparable percentages of presence between genders, suggesting that gender may not be a significant influencing factor in their prevalence within this dataset (Table 4).
|
Table 4: Comparison of microorganism with gender |
||||
|
Microorganisms |
Gender |
P value |
||
|
Female n (%) |
Male n (%) |
|||
|
Pseudomonas aeruginosa |
No |
18 (81.8) |
26 (83.9) |
1.000 |
|
Yes |
4 (18.2) |
5 (16.1) |
||
|
Klebsiella pneumoniae |
No |
19 (86.4) |
29 (93.5) |
0.638 |
|
Yes |
3 (13.6) |
2 (6.5) |
||
|
Staph aureus |
No |
21 (95.5) |
25 (90.6) |
0.218 |
|
Yes |
1 (4.5) |
6 (19.4) |
||
|
Serratia marcescens |
No |
21 (95.5) |
28 (90.3) |
0.633 |
|
Yes |
1 (4.5) |
3 (9.7) |
||
|
Escherichia coli |
No |
20 (90.9) |
29 (93.5) |
1.000 |
|
Yes |
2 (9.1) |
2 (6.5) |
||
|
Methicillin-Resistant Staphylococcus Aureus |
No |
21 (95.5) |
30 (96.8) |
1.000 |
|
Yes |
1 (4.5) |
1 (3.2) |
||
|
Proteus mirabilis |
No |
22 (100) |
28 (90.3) |
0.258 |
|
Yes |
0 (0) |
3 (9.7) |
||
|
Enterobacter cloacae |
No |
22 (100) |
30 (96.8) |
1.000 |
|
Yes |
0 (0) |
1 (3.2) |
||
|
Enterobacter aerogenes |
No |
21 (95.5) |
30 (96.8) |
1.000 |
|
Yes |
1 (4.5) |
1 (3.2) |
||
|
Citrobacter freundii |
No |
22 (100) |
30 (96.8) |
1.000 |
|
Yes |
0 (0) |
1 (3.2) |
||
|
Enterococcus faecium |
No |
22 |
30 |
1.000 |
|
Yes |
0 (0) |
1 (3.2) |
||
|
Acinetobacter baumanii |
No |
21 (95.5) |
31 (100) |
0.415 |
|
Yes |
1 (4.5) |
0 (0) |
||
|
Staph epidermidis |
No |
21 (95.5) |
31 (100) |
0.415 |
|
Yes |
1 (4.5) |
0 (0) |
||
P value: Fishers Exact test
Discussion
The current study showed that the prevalence of CLABSI was 18.84%. A California study conducted in 2022 on 1125 study participants determined the prevalence of CLABSI in both surgical and intensive care units (ICUs). The study showed that the rate of CLABSI in ICU was twice the national average and triple the national average for surgical/medical units (7). A study from Egypt done in 2018 estimated that approximately 6 cases per 1000 CL days were the incidence of CLABSI in a private hospital. Moreover, the mortality rate among patients who had CLABSI was almost 16.8% (10). Another prospective study involving multiple Asian and Middle Eastern countries concluded that CLABSI was much more prevalent in these countries as compared to the United States and Australia, and hence the prevalence was found to be comparable with this study (11). A research study from Saudi Arabia estimated the rate of CLABSI in the region to be 3.33 per 1000 CL days between 2018-2020, with a higher risk of infection in patients who have chronic kidney disease (12). Another study from Saudi between 2013-2016 concluded that the rate of CLABSI ranged between 2.2 to 10.5 per 1000 CL days among the health facilities, however, the mortality rate attributable to the CL was approximately 41.9% (13).
This study also identified the varying microorganisms causing CLABSI in Saudi Arabia. Pseudomonas aeruginosa was the leading microorganism present in the CLABSI culture followed by Klebsiella pneumonia. Other bacteria were all either present in minimal or trace amounts. A similar study performed in India showed a higher prevalence of CLABSI (22.5%). Additionally, various microorganisms were found to be responsible for the infections found in that study primarily including Staphylococcus aureus. The second isolate that was Gram-positive was a Coagulase negative staphylococcus (CONS). Most Gram-negative bacteria that were recovered from 3 (16.6%) individuals were Klebsiella species. Acinetobacter species and Pseudomonas aeruginosa were the other Gram-negative isolates (14). Dube et al. conducted a similar study to assess the prevalence of CLABSI and its bacterial composition at Soetomo General Hospital in 2020. The study found that both Gram-positive and Gram-negative bacteria were detected in blood cultures. Staphylococcus aureus was the most common Gram-positive organism, while Enterobacter cloacae was frequently identified among the Gram-negative bacteria. Variations in patient populations and predominant bacterial species between centers contributed to differences in organism distribution across regions and climates (15).
This study showed that CLABSI was found to be more prevalent in males as compared to females. Similar findings have been found in evidence in research studies based on descriptive data (16). However, these findings are sparsely present. Upon further investigation in this study, it was noted that the presence of CLABSI-causing bacteria was not significantly different between male and female patients, and hence it was concluded that gender was not a predictor for CLABSI in adults. Multiple studies have endorsed this finding from different regions around the world (17,18). The relationship between CLABSI and gender has been explored in various research studies however inconsistent findings have been identified (16). Another study from Italy highlighted that a higher prevalence was observed in females, which completely contradicts the findings of other studies (19). The difference in the CLABSI occurrence between males and females could be present due to less reporting from female patients, or a possible bias due to the exclusion criteria for missing data. Furthermore, differences based on anatomical skin consistencies and accumulation of bacteria due to environmental exposure were also one of the possible reasons highlighted for the probability of a higher incidence of CLABSI in males as compared to females (20).
Moreover, in this study, an increasing trend of CLABSI occurrence was observed in the month of June 2022 as compared to other months. Literature suggests that CLABSI is known to peak during summers due to the prevalent presence and increase in the multiplication of gram-negative bacteria. Multiple prospective longitudinal studies have proven that there is a peak in the incidence of CLABSI in warmer months (21-23).
Hygiene is a key factor in preventing CLABSI. Research has shown that high CALBSI rates can be linked to low adherence to hygiene protocols. Enhancing hand hygiene is critical, along with the use of protective equipment such as masks and sterile gowns. According to Sahli et al., diabetes and extended use of central venous catheters (CVCs) for 10 days or more are significantly associated with an increased risk of CVC-related infections. These factors are recognized as primary infection risks in hemodialysis patients (24).
Study Limitation
Several limitations should be considered in interpreting the findings of this study. The retrospective nature of the research, which relies on existing medical records, may have introduced constraints regarding data accuracy and completeness. Additionally, the exclusion criteria employed might have introduced selection bias, limiting the representation of certain subsets of hemodialysis patients. Being a single-center study, the generalizability of findings to broader populations or varied healthcare settings might be restricted. Furthermore, the analysis focused on specific parameters such as gender, and identified microorganisms, while lacking a comprehensive inclusion of broader demographic factors (e.g., age, socio-economic status) and clinical variables (e.g., coexisting medical conditions, immune status). The absence of these crucial variables might limit the depth of understanding regarding factors influencing CLABSI development among hemodialysis patients.
Recommendations
Based on the findings of this study, several recommendations can be proposed to mitigate the risk of CLABSI and improve patient outcomes. Primarily, the implementation and reinforcement of standardized catheter care protocols, emphasizing strict aseptic techniques during insertion, maintenance, and removal of central venous catheters is very crucial. Moreover, using checklists and standardized guidelines is essential for the maintenance of quality and best practice protocols within a healthcare facility (25). Fostering collaboration among healthcare professionals involved in the care of hemodialysis patients, including nephrologists, infectious disease specialists, nurses, and infection control practitioners also plays a vital role in the prevention of CLABSI. Regular interdisciplinary meetings can facilitate the exchange of knowledge and insights to enhance infection prevention strategies (26). Additionally, regular training sessions for healthcare providers on these protocols can help ensure adherence and should be made mandatory for critical care staff. This training also encourages the use of alternative vascular access methods, such as arteriovenous fistulas or grafts, to reduce reliance on central venous catheters. Timely referral for vascular access creation and monitoring can minimize the duration of catheter use.
Another prevention method is to establish a robust surveillance system for monitoring CLABSI rates and associated risk factors. Routine data collection and analysis can facilitate the early identification of trends, allowing for timely interventions and improvements in infection prevention strategies. Moreover, continuous quality improvement initiatives and infection control audits to regularly assess and refine infection control practices are the keys to strengthening the prevention of CLABSI. This involves ongoing evaluation of processes, identification of areas for improvement, and the implementation of evidence-based interventions (27). By incorporating these recommendations, the King Fahad Armed Forces Hospital Renal Dialysis Center in Jeddah can enhance its infection prevention measures, ultimately reducing the prevalence of CLABSI and improving the overall safety and well-being of hemodialysis patients.
Conclusions
In conclusion, the findings of this study underscore the significance of addressing this critical issue to improve patient outcomes and enhance the quality of care. Understanding prevalence improves assessment of CLABSIs burden in clinical settings, while analyzing risk factors helps inform targeted prevention strategies. It may also have an important impact on policy-making that will advance patient safety. Moving forward, continuous efforts in quality improvement, vigilant monitoring, and a commitment to antimicrobial stewardship will be instrumental in reducing CLABSI rates and elevating the overall standard of care.
Disclosure
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
The study was approved by The Research Ethics Committee of Armed Forces Hospitals-Jeddah with approval number: REC 667. An informed consent was provided by the patients to include the data anonymously.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.