Volume 5, Issue 8
August 2025
Epidemiology, Management, and Prognosis of Periodontal Disease in the Elderly
Mohammed Abdullah Batwa, Israa Sayed AbuHamdah, Abdullah Mohammed Alzahrani, Sahaib Ghazi Alotaibi, Alaa Abdulkaliq Albasher
DOI: http://dx.doi.org/10.52533/JOHS.2025.50808
Keywords: Periodontal disease, older adults, immunosenescence, biomarker-based diagnosis, epidemiology, management, artificial intelligence in periodontology
Managing chronic, non-communicable diseases, such as periodontal disease, is particularly challenging for older adults. The aging population is increasing more rapidly than in the past, which emphasizes the need for healthcare systems to refine tailored approaches for management and treatment in older adults. Periodontal disease, a progressive inflammatory condition affecting the tissues surrounding teeth, is indeed more common in older adults. This is primarily due to age-related changes in the body's immune system and overall health, alongside the cumulative effects of bacterial plaque buildup over time. This review focuses on the complex relationship between periodontal disease and various systemic conditions, particularly in older adults, highlighting the role of inflammation and bacterial factors in conditions like diabetes, cardiovascular disease, and cognitive decline. In addition to the promising diagnostic approaches that can be developed based on understanding such interaction. It also provides tailored prevention and management strategies for older adults and explores the potential role of AI, aiming to improve oral health outcomes in geriatric patients and the overall quality of their lives.
Introduction
Most people nowadays tend to have longer life expectancies attributable to enhancements in healthcare and quality of life. The WHO reported that the population is aging faster than it has in the past and that by 2050, the percentage of people over 60 will have doubled from 12% to 22%. This rapid shift has drastic consequences on overall health. Aging often leads to frailty, characterized by a decline in physical and mental capabilities, increasing vulnerability to age-related diseases, including oral health problems (1).
Oral diseases are among the most prevalent non-communicable diseases globally, and periodontal disease is a prominent one. Periodontal disease, specifically, is an inflammatory condition arising from the buildup of plaque around the teeth. Periodontal diseases can often be prevented during the early stages. However, they can progress into periodontitis, where the periodontal ligament and alveolar bone are destroyed if left untreated. It presents a persistent health concern in the aging population (1, 2).
Recent global estimates showed that over 42% of adults have some form of periodontal disease. Periodontal disease has more DALYs (Disability-Adjusted Life Years) than dental caries, which has a higher incidence (3). The evidence suggests that the number of serious cases has significantly increased. As people age, the prevalence of periodontal disease rises; 60% of those people aged 65 and older suffer from some form of periodontal disease (2).
This incidence of periodontal disease is governed by several intrinsic and extrinsic factors. Compared to young populations, the elderly are more susceptible to developing periodontal disease because of the decline in physiological and mental capacities. Other influencing factors include education level and social and economic conditions, as well as limited self-care abilities of the elderly. Furthermore, the pathogenesis of periodontal diseases is influenced by several systemic diseases such as diabetes and cardiovascular disorders. Therefore, there is an urgent need for developing approaches to aid in the management of such complex diseases (4-6). In response to this multifactorial challenge, researchers and clinicians should develop effective management strategies as well as preventive measures and educate patients about the significance of oral healthcare. The advancement in technology should also be put into practice by developing novel approaches for treatment and early diagnosis (7, 8). This review aims to explore the epidemiology and prognosis of periodontal disease in older adults, as well as effective management approaches and preventive measures. Thus, it provides insight into new management and treatment approaches that are more applicable to elderly patients.
Methodology
This review is based on an inclusive literature search conducted on July 16, 2025, in the PubMed and ClinicalKey databases, as well as Google Scholar. Utilizing MeSH (Medical Subject Headings) and relevant keywords, such as periodontal disease, older adults, immunosenescence, biomarker-based diagnosis in periodontology, epidemiology, prevalence, management, and artificial intelligence in periodontology, the search aimed to explore studies on epidemiology, pathogenesis, clinical staging, and novel identified risk factors of periodontal disease in older adults as well as associated complications and personalized management approaches. Moreover, it examined the latest advances in periodontology, such as the use of AI and biomarkers in diagnostics. The search was not confined by publication date, language, or type of publication to ensure a broad exploration of the available literature.
Discussion
Epidemiology of Periodontal Diseases
Examining the prevalence and demographic nature of a disease is essential to fully understand its impact. With a global incidence of 45%, oral disorders are among the most common noncommunicable diseases (NCDs) in the world, impacting around 3.5 billion people and ranking as the 11th most common cause of disability worldwide (3, 9). Geographically, the prevalence of periodontitis varies. Western Sub-Saharan Africa was designated as a high-risk region, and the Gambia had the highest burden in the most recent WHO study from 2019 (10).
Approximately 8% of people over thirty worldwide suffer from severe periodontal disease, while over 42% of adults have some form of the condition. As people age, the incidence rises. It is estimated that 60% of adults 65 and older have some kind of periodontal disease. It is more prevalent in men than women, affecting over 50% of men and only 35% of women (2, 10).
Periodontal disease pathogenesis in older adults involves bacterial infection, host immune response, and age-related changes that lead to inflammation and tissue damage.
Pathogenesis of periodontal disease
Periodontal disease is a progressive oral disease characterized by the formation of dysbiotic biofilm of bacteria, which evokes an inflammatory immune response, leading to the progressive damage of soft and hard periodontal tissue. Inflammation enhances further bacterial growth, and bacteria intensify the inflammation, creating a positive feedback cycle of infection and damage that gradually destroys the periodontal tissue and alveolar bone (11-15).
According to the 2018 classification (used by Salvi et al., 2023), periodontitis is classified by staging and grading into 4 stages, based on severity, complexity, and risk. The clinical attachment loss (CAL) and bone loss increase gradually from 1-2 mm in stage I initial periodontitis, which is mostly reversible with good care, until it reaches a CAL ≥5 mm, pocket depths ≥6 mm, and tooth in stage VI advanced periodontitis, which is characterized by masticatory dysfunction and bite collapse. Complex rehabilitation is often needed (16).
Diagnosis is based on a group of clinical parameters such as probing depth, which is measured using a periodontal probe; bleeding on probing, which indicates inflammation; and clinical attachment loss (CAL), which indicates tissue damage. Furthermore, radiographic assessment is required to detect the pattern and extent of bone loss and to compare baseline radiographs with progressive ones to detect prognosis (16).
Key clinical signs include red, swollen gums, bleeding on probing (BOP), deep periodontal pockets (≥4 mm), gum recession, tooth mobility, and radiographic bone loss. Patient-reported symptoms include bleeding during brushing or eating, halitosis (bad breath), loose teeth, pain or discomfort in the gums, and sensitivity to hot/cold due to exposed roots (16).
Risk factors
Age-related biological changes in the elderly contribute to an increased susceptibility and prevalence of periodontal disease. These changes impact the immune system, making older adults more vulnerable to the bacteria that cause gum disease.
Age-related biological factors
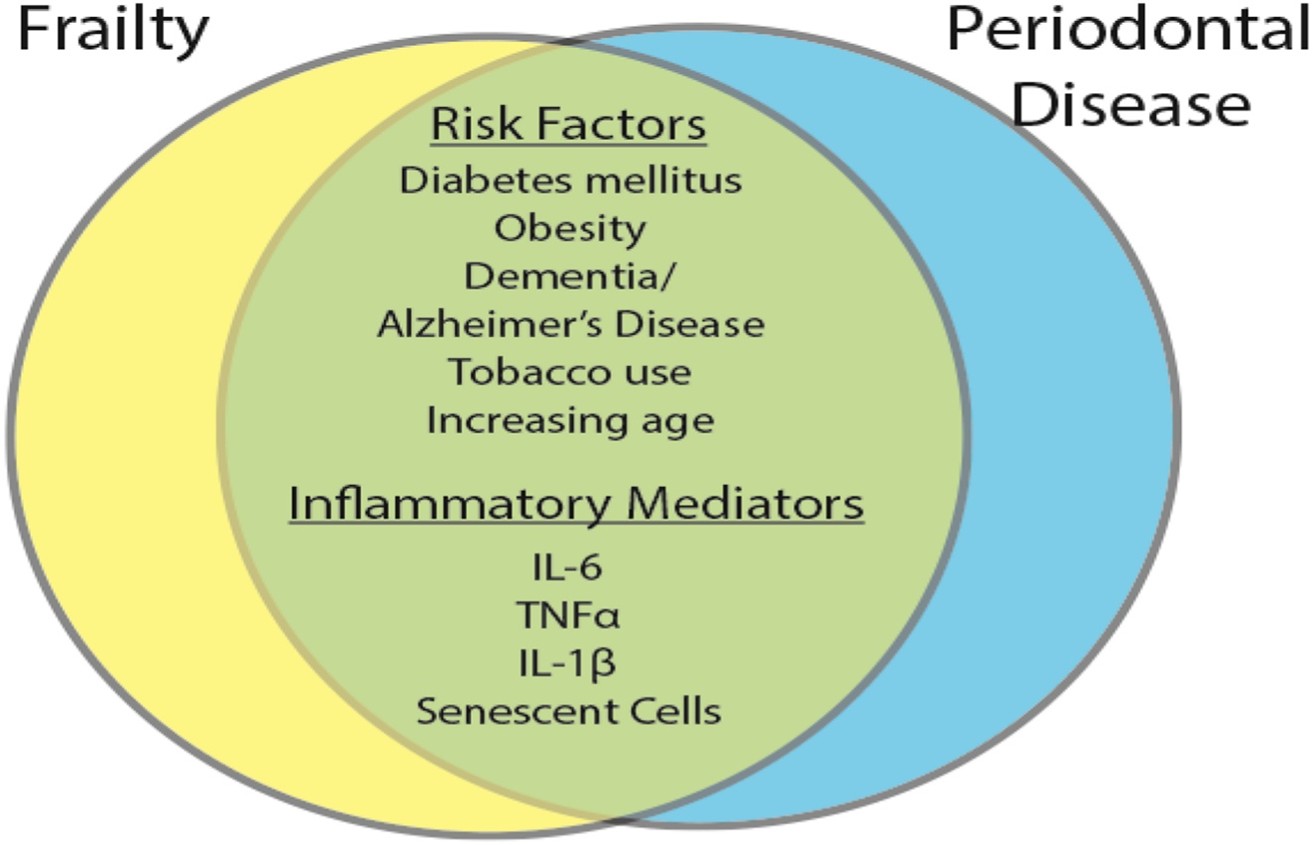
Immunosenescence is the age-associated decline in immune function, often exacerbated by frailty, and leads to chronic low-grade inflammation known as inflamm-aging. The increased levels of inflammatory markers like IL-6 and TNF-α induce apoptosis of neutrophils, leading to lower bacterial clearance. While macrophages shift toward an inflammatory state, T cells move toward pro-inflammatory types (Th1 and Th17), which promote tissue damage, resulting in more inflammation. Senescent cells also accumulate in tissues, releasing the senescence-associated secretory phenotype (SASP), which triggers inflammation by turning more cells senescent. Thus, promoting immune dysfunction. This aging process is governed by the mTOR pathway, which impairs cell repair and promotes inflammation. These biological changes make older adults more susceptible to infections and chronic diseases like periodontal disease (7, 8, 11, 13, 15, 17-20) (Figure 1).
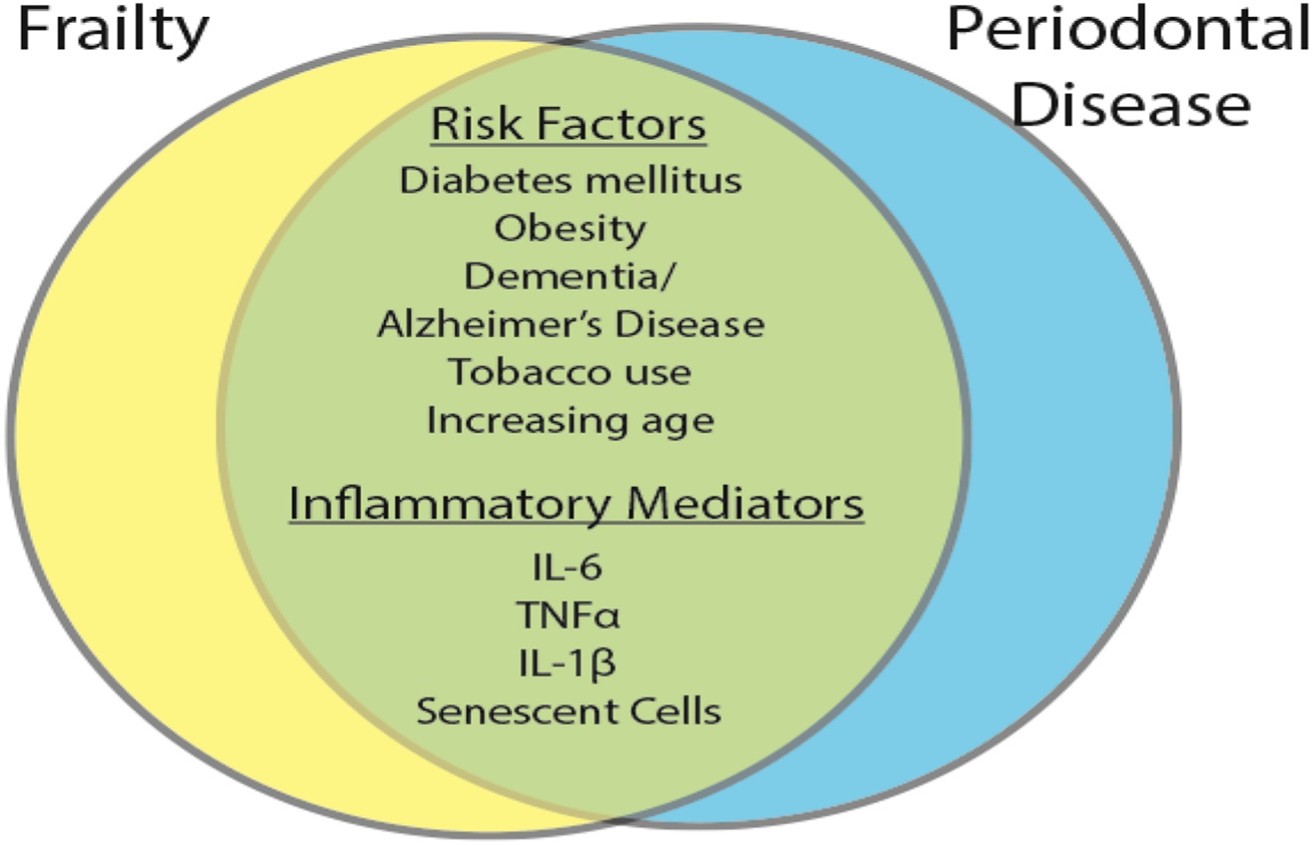
Figure 1: Shared features of periodontal disease and frailty. Many of the risk factors and comorbid diseases are similarly associated with frailty and periodontal disease. Similarly, systemic and local inflammatory mediators are shared across the two conditions (13).
Socioeconomic and Psychological Factors
In addition to age-related biological factors, social factors like low income and education have also been correlated with worse oral healthcare, leading to increased risk of periodontal disease. This correlation between periodontal disease and socioeconomic status could be further explained by the allostatic load, which is the physiological effect of being exposed to chronic stress. This interrelationship could also be influenced by other factors, such as sex, race, and ethnicity. Additionally, those struggling with depression and other mental illnesses, as well as institutionalized patients, often have limited access to therapy and tend to ignore their oral health, increasing the risk of developing periodontal disease (5, 6). Differences in social and economic standards, as well as education level, result in different behavioral and oral care habits, influencing the risk of periodontal diseases.
Oral and Behavioral Factors
Alongside the impact of mental illnesses, older adults often suffer from loss of dexterity (ability to use their hands skillfully), leading to a decline in oral health care. Additionally, diseases like cognitive impairment and dementia elevate the risk of several oral disease conditions like tooth loss (edentulism), decay (caries), periodontal disease, and others. This stems from patients’ limited self-care abilities, which lead to neglect of their oral health (4, 5).
Edentulism is particularly common in older adults, where 25% of aged patients suffer from edentulism before the age of 80 years. It results in malnutrition and challenges in prosthodontic replacement, leading to an increased risk (4, 5).
Dental implants, while effective for replacing missing teeth, can trigger an inflammatory response due to the presence of titanium particles. These particles, released during implant installation or from wear and tear, can be recognized as foreign substances by the body's immune system, leading to inflammation and potentially peri-implantitis (4, 5).
Nutritional Factors and Obesity
Adequate nutrition is fundamental for a properly functioning immune system, effective regulation of inflammation, and efficient tissue repair. A balanced diet provides the necessary building blocks for immune cells, regulates inflammatory responses, and supports the cellular processes involved in healing. Poor nutrition may modulate inflammatory immune response and tissue healing, thus triggering periodontal disease. Additionally, some studies have linked obesity with inflammatory pathways. However, the association between healthy nutrition and periodontal diseases needs further exploration (4, 5, 21). Older adults are more prone to developing other systemic diseases in cases of malnutrition or unhealthy diets.
Medication Use
Alongside malnutrition, health gradually declines with aging, in part because of physiological and psychological changes, such as immunosenescence, decline of oral mucosa/salivary gland function, and oral microbiota imbalance (frailty), which leads to older adults consuming numerous medications concurrently (polypharmacy). Accordingly, most older adults suffer from xerostomia, which contributes to disease progression (4, 13, 22, 23).
Besides the impact of polypharmacy, certain systemic medications, like those used in the treatment of diseases common among older adults, like immune diseases and mental illnesses (e.g., SSRIs, bisphosphonates, steroids, and TNF-alpha inhibitors), can impair bone healing or alter immune response. Not only does xerostomia caused by polypharmacy of legally prescribed drugs contribute to periodontal disease development, but also smoking and illegal substance abuse elevate the risk.
Smoking and Substance Abuse
Periodontal diseases are prevalent among smokers. Over 60% of current smokers suffer from periodontal disease. Smoking tobacco has been reported to be associated with the pathogenesis of periodontal disease. Poor periodontal tissue healing outcomes are common among smokers, as smoking induces the immune inflammatory response, changing the subgingival microbial community, resulting in dysbiosis (4, 5, 24).
Besides tobacco and cigarettes, a limited number of studies reported that frequent long-term abuse of cannabis causes recessions, deep pockets, gingival enlargements, and loss of periodontal attachment. Little evidence further demonstrates that the regular abuse of cocaine can induce traumatic or necrotizing ulcerative lesions likely triggered by the chemical reactions resulting from its repeated application to the gums. There’s little evidence available regarding other substances. More evidence-based studies are essential to obtaining accurate and reliable information (4, 5).
If the risk factors and diagnostic symptoms remain unaddressed, periodontal disease may result in severe complications, not only affecting oral health but also overall systemic health.
Complications and Prognosis in Older Adults
Edentulism, often caused by persistent tissue damage from untreated periodontitis, malnutrition caused by pain and difficulty chewing, and xerostomia, are among the common complications of periodontal disease. Additionally, those suffering from periodontitis may develop severe infectious diseases, such as aspiration pneumonia, by inhaling pathogens from periodontally infected sites. (6, 9).
In addition to infectious diseases, chronic inflammation caused by periodontal disease pathogens contributes to cardiovascular and systemic diseases such as atherogenesis (via IL-6, CRP, and TNF-α), endothelial dysfunction, and a higher risk of myocardial infarction and stroke. Recent studies showed that periodontal inflammation has an impact on cognitive function and dementias via its interaction with the microbiome (15, 25, 26).
Management Strategies for Older Adults
While advanced periodontal disease is not curable, it can be effectively managed to prevent further complications, particularly in older adults where tailored approaches are crucial. Management strategies need to consider age-related physical and mental health changes, alongside the disease's progression. Consistent and lifelong adherence to good oral hygiene practices is crucial for preventing and managing periodontal disease. This involves a combination of effective plaque control through brushing and flossing, regular dental checkups, and addressing any underlying health conditions. Developing care programs tailored according to the patient's cognitive abilities and level of independence is necessary to ensure applicability. Promoting dental coverage under national health insurance frameworks should help lessen financial restrictions (7, 8).
Interprofessional collaboration between clinical teams and caregivers can facilitate early detection. Furthermore, educational training programs in geriatric dentistry are necessary to educate dentists about suitable approaches for dealing with the elderly and the underlying systemic comorbidities associated with aging. A key consideration is the patient’s comfort, functionality, and satisfaction should be the top priority. Overall, the main goal of effective management of periodontal disease in older adults is preventing the development of systemic complications. This can be achieved by early diagnosis.
Emerging Topics and Future Prospects
Association of Periodontal Disease with Systemic Conditions and Biomarker-Based Diagnosis
Periodontal microbes enter the bloodstream through routine activities like chewing, brushing, flossing, and invasive dental procedures. Such bacteremia is temporary and can be effectively cleared by the immune system in healthy periodontal tissues. However, in periodontal disease, inflammation leads to the formation of a more persistent bacteremia that involves a greater number of microorganisms. Pathogens found in the mouth can enter the bloodstream and travel to various tissues and organs, contributing to the development of systemic diseases like type 2 diabetes, atherosclerosis, and neurodegenerative disorders.
Diabetes mellitus is a metabolic disorder of glucose. It is characterized by elevated levels of glucose in the blood, caused either by a lack of insulin in type 1 diabetes or by insulin resistance linked to beta-cell dysfunction in type 2. The two-way interplay between periodontal disease and type 2 diabetes can be explained by periodontal inflammation increasing insulin resistance by impairing beta cells through the release of cytokines like TNF-α and IL, resulting in impaired glycemic control, which in turn promotes periodontitis by enhancing further inflammation. This can be detected by HbA1c levels (23).
Cardiovascular diseases (CVD) are indeed more prevalent among individuals with periodontal disease, and this connection is thought to be partially explained by the systemic inflammatory response triggered by bacteria from periodontal pockets entering the bloodstream. This inflammatory response, characterized by an elevation in C-reactive protein (CRP).. High CRP levels are a known risk factor for CVD, suggesting a potential pathway through which periodontitis might contribute to heart disease (19, 24, 25).
Periodontal disease can lead to malnutrition and weakness due to inflammation and chewing difficulties, which in turn can contribute to frailty. Conversely, frailty, with its associated factors like malnutrition and muscle weakness, can also increase the risk and severity of periodontal disease (4, 26).
In severe or untreated periodontal disease, pathogens and inflammatory substances can potentially cross the blood-brain barrier, leading to neuroinflammation and cognitive decline, including Alzheimer's disease and dementia. Given the often-irreversible nature of advanced periodontal disease, early detection and intervention are crucial to prevent both oral and systemic complications. Β-amyloid and tau protein (the hallmarks of these disorders) serve as biomarkers in neurodegenerative diseases (27) (Figure 2).

Figure 1: Overview of periodontitis and its associated comorbidities (28)
The use of AI can be particularly beneficial in biomarker-based diagnostics. AI systems can be used to analyze complex biomarker datasets and identify overlooked patterns, enhancing diagnostic insights.
Artificial Intelligence in Periodontology
AI is progressively incorporated into the field of periodontology. It can improve personalized care, treatment planning, and diagnostic accuracy. In addition to identifying periodontal bone loss and furcation involvement, AI can easily estimate the course of a disease or the effectiveness of a treatment by integrating clinical and radiological as well as genetic data via deep learning. AI holds significant promises for transforming geriatric periodontology, offering advancements in prevention, diagnosis, and personalized treatment approaches. AI-powered tools can enhance the early detection of periodontal disease, improve treatment planning, and enable more tailored therapies, ultimately leading to better oral health outcomes for older adults (29).
Conclusion
Managing periodontal disease poses significant challenges in elderly individuals because of the interplay of biological aging, behavioral challenges, comorbidities, and socioeconomic barriers. Therefore, it requires strategies that meet the physical and mental needs of the elderly and adapt to their capabilities and overall health conditions. Employment of AI and biomarker diagnostics offers an opportunity to enhance diagnostic accuracy and develop tailored care strategies for the aging population.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical considerations
This study is a review of previously published literature and does not involve any original data collection involving human or animal subjects. Therefore, ethical approval was not required.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.