Volume 5, Issue 9
September 2025
The Knowledge and Attitude of Family Physicians Toward Urine Dipstick Results in Antenatal Clinics in the Primary Health Care Centers in Jeddah, Saudi Arabia
Razaz Wali, Feras Fatani, Saleh Alhumaidah, Abdulrahman Qutub, Warif Farrash, Amir Abushouk
DOI: http://dx.doi.org/10.52533/JOHS.2025.50904
Keywords: Saudi Arabia, antenatal clinic, attitude, knowledge, family physician, urine dipstick test
Background: The urine dipstick test is widely used in antenatal care units. The test may yield false positives and false negatives, raising concerns about its overall accuracy. Furthermore, pregnancy may affect the presence of positive components. The decisions to react to these findings differ according to knowledge, experience, and guidelines. Therefore, this study aimed to assess the knowledge and attitude of family physicians toward dipstick test results in antenatal clinics.
Method: A cross-sectional survey was conducted on family physicians in National Guard Health Affairs (NGHA-WR) IN Saudi Arabia. Data was collected using a questionnaire, and different sections for evaluating the level of knowledge and attitude thoroughly. The median presented variables as the distribution was skewed to the left with a 95% confidence interval. Chi-square and Fisher's exact tests were used to compare categorical variables.
Results: Out of 95 family physicians invited, 75 responded (response rate: 78.95%). The majority were aged 24–35 years 56 (74.67%) and had less than five years of experience 51 (68%). Glucose was the most commonly recognized urine dipstick component 7316.10%), while bilirubin and urobilinogen were the least recognized 43 (9.50%). About 35 (46.67%) of participants were unaware of false positive and false negative dipstick results, and 14 (18.76%) did not know when such results should be considered. Despite this, 60 (80%) of physicians reported proceeding with further investigations regardless of the patient’s symptoms. Significant associations were found between knowledge and variables such as age, physician position, and years of experience (p < 0.05). However, no significant associations were found between attitude and any of the studied variables.
Conclusion: The behavior of the doctors may be affected by their experience and expectations. Therefore, implementing evidence-based medicine and the regular review of clinical guidelines can unify clinical decisions and efficacy in primary health care centers.
Introduction
Antenatal care plays a critical role in improving maternal and fetal health outcomes by enabling early detection and timely management of potential complications during pregnancy. Regular antenatal visits are associated with reductions in maternal mortality, preterm births, and low birth weight, particularly when screening tools are effectively utilized (1). Urinalysis is a fundamental component of routine antenatal screening and plays a pivotal role in safeguarding maternal and fetal health. It allows for the early detection of conditions such as urinary tract infections (UTIs), gestational diabetes, and hypertensive disorders like preeclampsia—each of which can have significant implications if left unrecognized (2).
Urinalysis is either a microscopic or routine dipstick. Microscopic urinalysis involves examining urine samples under a microscope to identify various components such as white blood cells, red blood cells, bacteria, and crystals. On the other hand, urine dipstick test is capable of detecting abnormalities in the blood, hemoglobin, leukocyte esterase, protein, glucose, bilirubin, and urine-specific gravity (3). Hematuria, the presence of blood in urine, is commonly associated with UTIs and can also indicate kidney-related issues like kidney stones (4, 5). However, hematuria is relatively common in pregnant women and may not necessarily indicate serious conditions such as preeclampsia or UTIs (6). Leukocyte esterase is a reliable indicator of UTIs and can be useful for pregnant women, even if they have no apparent symptoms (7, 8). A negative leukocyte esterase result suggests a significantly reduced likelihood of infection (5). Additionally, a small amount of protein is normally present in urine (less than 150 mg/day). However, proteinuria, when protein levels exceed 150 mg/day, indicates serious conditions like preeclampsia (9). While glycosuria generally indicates high blood sugar levels, it's important to note that in pregnant women, glycosuria can be expected due to increased glomerular filtration rate and is not used as a sole indicator of high blood sugar levels (10). Liver diseases, such as prehepatic and intrahepatic jaundice, are suspected in cases of high levels of urobilinogen. Still, in pregnant women, it is unlikely to indicate hepatic-related disorders (11). Moreover, high urine specific gravity may detect heart failure and volume loss, while low urine specific gravity might indicate renal failure or diabetes insipidus (5, 12, 13).
Family physicians order the urine dipstick test due to its accessibility and low cost (14). It is considered useful in various clinical settings, particularly to exclude infections in leukocyte esterase-negative patients (15). However, despite its widespread concerns remain regarding its variable accuracy in detecting UTI, such as bacteriuria (14, 16). A relatively high number of asymptomatic pregnant women have shown positive urine dipstick results (17). Testing for leukocyte esterase and nitrite by urine dipstick test in screening asymptomatic urinary tract infected patients has shown many false-negative and false-positive results among pregnant women (18). Despite its convenience urine dipstick tests miss many infections, which may exacerbate the consequences of undetected clinical conditions. Its diagnostic performance may vary between asymptomatic and symptomatic individuals, with notably lower sensitivity in the former. As a result, its routine use, particularly among low-risk pregnant women, has been questioned. Various factors could result in false negative results. Excessive fluid intake may dilute the urine and affect urine dipstick test accuracy. In addition, using antibiotics could also result in no apparent infection (15, 19). Moreover, ascorbic acid consumption may lead to false negative findings (20, 21). However, the urine culture, the gold standard, has established fewer false negatives and positives than the urine dipstick test (18). Furthermore, the urine dipstick test shows moderate sensitivity and relatively high specificity in detecting preeclampsia, so there is uncertainty about its reliability as a standalone test (22). In the National Guard Health Affairs-Western Region (NGHA-WR), family doctors frequently use urine dipstick tests among pregnant women. However, the change in physicians' decisions based on the urine dipstick results has not been adequately studied. It is believed that physicians' attitudes toward urine dipstick results vary, and the results are not always considered. Important findings may be overlooked if urine dipstick results are not adequately considered. Therefore, this study aims to assess physicians' knowledge and attitude toward the findings of urine dipstick tests in antenatal care in the primary health care center in the NGHA-WR.
Material and methods
Study design
A quantitative cross-sectional questionnaire-based study was conducted to assess the attitude and knowledge of family physicians toward urine dipstick test results. A non-probability consecutive sampling technique was the chosen modality. All the data were collected depending on the family physicians in NGHA-WR.
Study setting and participants
This study was conducted in the primary healthcare centers in NGHA-WR in Saudi Arabia. The questionnaire targeted 95 family physicians, which represents the total number of physicians. The number of family physicians was determined based on the center managers in each primary healthcare center of NGHA-WR in Saudi Arabia.
Selection criteria
The study included physicians currently practicing in the five selected primary healthcare centers who provided informed consent and agreed to participate in the survey. Physicians not affiliated with NGHA-WR or not working in the selected centers were excluded, as were personnel not directly involved in clinical family practice, such as administrative officers, nurses, or other healthcare workers. Additionally, family physicians who participated in the pilot testing of the questionnaire, as well as individuals who declined consent or submitted incomplete questionnaires, were excluded from the main study sample.
Data collection method
This cross-sectional study collected data through a self-developed questionnaire after an inclusive literature review (23, 24). The questionnaire underwent a process of face validity assessment by being sent to four expert family physicians. Minor modifications were made based on the observations and feedback provided by these specialists. Additionally, a pilot study involving 30 family physicians who were not part of the main sample was conducted, leading to further refinement in the validation process. The original 32-item questionnaire was subsequently reduced to 28 items following the pilot study and face validity assessment, and this revised version was employed as the data collection instrument. Furthermore, the reliability of the questionnaire was evaluated using Cronbach's alpha test.
The questionnaire's properties were evaluated through tests of internal consistency (reliability).
Reliability analysis
Internal consistency reliability was assessed using Cronbach’s alpha. Domain 1, which assesses physicians’ knowledge of urine dipstick tests and includes 9 items, demonstrated a Cronbach's alpha of 0.722, indicating an acceptable internal consistency. Domain 2, focused on physicians’ attitudes toward urine dipstick tests and consisting of 13 items, showed a Cronbach's alpha of 0.766, suggesting acceptable internal consistency.
Furthermore, the survey was divided into three sections. First is the sample's demographic, which includes five questions. The second section is ten questions about physicians' knowledge of urine dipstick tests. The final section, which consists of 13 items, studies the attitude of physicians toward urine dipstick tests.
The survey was based on yes, no, and sometimes or maybe questions. Also, multiple response questions were used to ask about the components seen in the urine dipstick test. In addition, a separate part related to the attitude section was developed to assess when they will act. The questionnaire was distributed to the family physicians in person. The researchers went to the centers and took the responses individually.
Data analysis
The data were entered into an Excel sheet on a personal laptop and assessed only by the research team. The data was analyzed using JMP 15. The categorical variables were presented by percentage frequency, and continuous variables were presented by mean and standard deviation. The statistical association between two categorical variables was assessed through the use of a chi-square test. To explore the relationship between numerical and categorical variables, a T-test was employed. The Cronbach alpha test was used to test the reliability of the questionnaire, as between 0.7 and 1.0 is a good result.
Regarding the knowledge, the value was 0.62, while it was 0.78 for the attitude part. The p-value is significant when it is less than 0.05, and a 95% Confidence interval was used. The cut-off point was used to estimate the knowledge and attitude of physicians in the primary health care centers of the NGHA-WR.
In order to assess the participants' level of knowledge and attitude, the results were categorized into three levels: poor, moderate, and high, using a scoring scale. The survey responses were assigned corresponding marks, where "yes" received two marks, "no" received zero marks, and "sometimes" or "maybe" received one mark. The knowledge section consisted of nine questions, with a total possible score of 18. Similarly, the attitude section comprised seven questions with a total score of 14. The participants' knowledge level was categorized as poor if they scored 13 or less, moderate if they scored between 14 and 17, and high if they scored 18. In terms of attitude, a score of 11 or less was considered low, 12-13 was deemed reasonable, and 14 indicated an increased level of attitude.
Ethical approval
After Institutional Review Board (IRB) approval was attained from King Abdullah International Medical Research Center (KAIMRC), IRB number: IRB/0729/22, on Apr 5, 2022. An informed consent form preceding the questionnaire that included the research's title, specialty, and privacy insurance clarified that all personal information had been unreleased, and the only data used were the answers. Additionally, the consent included either agreement or disagreement to participate. By agreeing to the consent, the participants were asked for personal information, not identifying them.
Results
In this study, 75 responses were collected from a population of 95 family physicians working in primary healthcare centers of NGHA-WR, with a response rate of 78.95%. Five centers in the western region were included. Out of the total number of respondents, the majority (N=34, 45.33%) were affiliated with specialized polyclinics, while the smallest number of responses came from the staff health clinic (N=4, 5.33%). The age group of 24-35 represented the highest proportion (N=56, 74.67%) among the participants. A significant number of participants were residents (N=37, 49.33%). The majority of respondents (N=51, 68%) had less than five years of experience as family physicians. Additionally, a relatively small portion of participants (N=27, 36%) had prior experience outside the NGHA (Table 1).
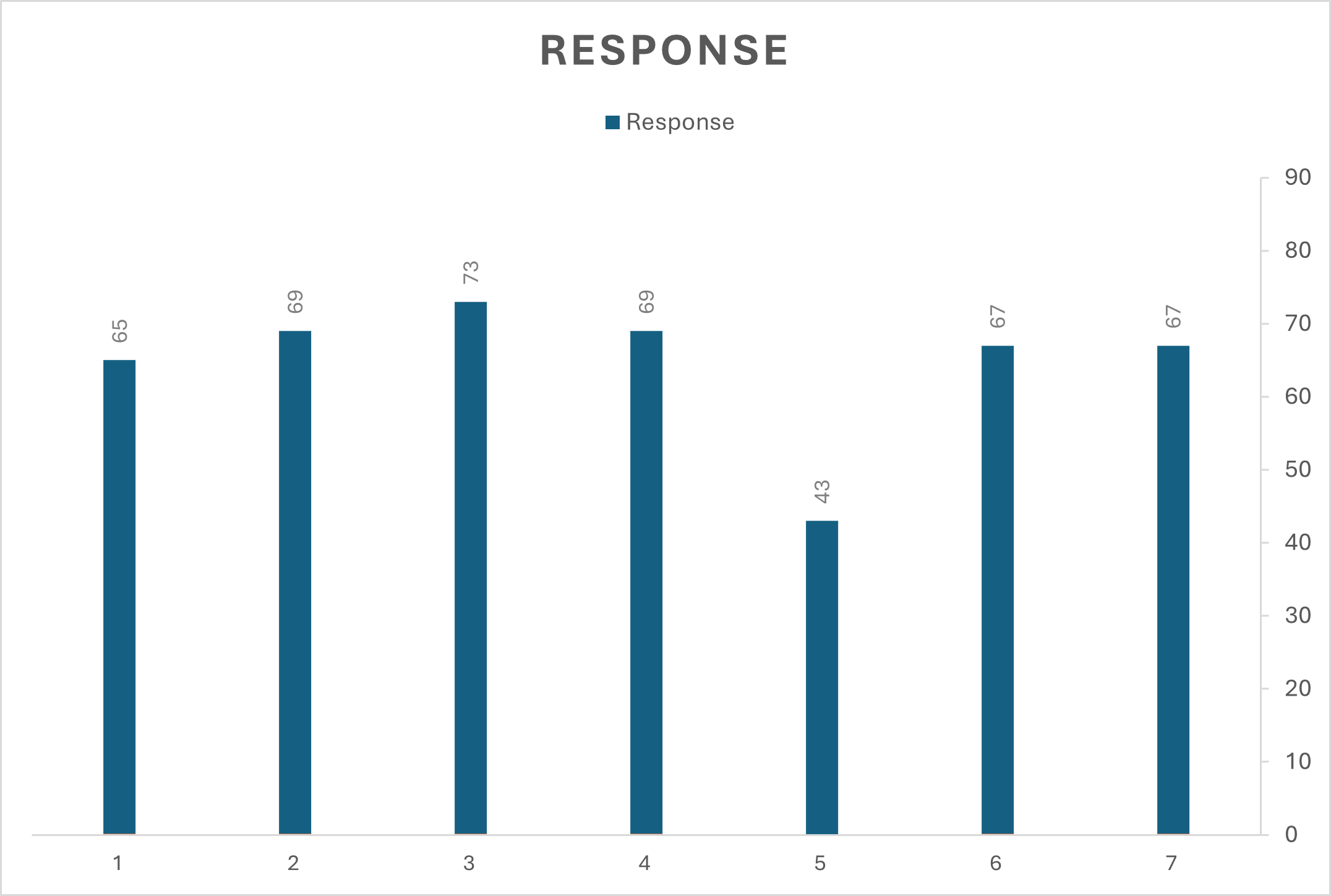
The study consists of two sections: knowledge and attitude. The physicians were asked to determine what could be measured by the urine dipstick test in a multiple-response question, and the number of responses was 453. The highest was glucose (N=73, 16.10%), while the least was bilirubin and urobilinogen (N=43, 9.50%). The other variables ranged from 67 (14.80%) to 69 (15.20%) (Figure 1).
Most participants know when to use the urine dipstick test (N=56, 74.67%). Moreover, 58 (77.33%) of the participants know when to consider the results dangerous. Furthermore, (N=57, 76%) of the participants are familiar with further investigations of the positive results. However, (N=35, 46.67%) of the participants are not always aware of false positive and false negative effects, while (N=14, 18.76%) do not know when to consider them. Most participants know when to refer patients to other departments (N=57, 76%). Whether the patient is symptomatic or not, further investigations are done based on positive results by 60 (80%) of family physicians. Furthermore, most physicians are confident in taking proper history according to urine dipstick results (N=69, 92%). (N=15, 20%) of the participants do not personally check the test results. Additionally, almost half of the doctors do not always refer patients after positive test results (Table 2).
|
Table 1: Demographic data of the included participants |
||
|
At which center do you work? |
Quantification |
Percentage |
|
Bahrah |
14 |
18.67% |
|
AL-Iskan |
14 |
18.67% |
|
AL-Shara’i |
9 |
12% |
|
Specialized polyclinic |
34 |
45.33% |
|
Staff Health Clinic |
4 |
5.33% |
|
Age (years) |
||
|
24 – 35 |
56 |
74.67% |
|
36 – 45 |
13 |
17.33% |
|
46 – 55 |
4 |
5.33% |
|
56 – 65 |
2 |
2.67% |
|
Position |
||
|
Staff physician |
11 |
14.67% |
|
Board certificate family physician |
12 |
16% |
|
Assistant consultant |
2 |
2.67% |
|
Consultant |
13 |
17.33% |
|
Resident |
37 |
49.33% |
|
Years of experience |
||
|
Below 5 |
51 |
68% |
|
5 – 10 |
15 |
20% |
|
More than 10 |
9 |
12% |
|
Experience in antenatal care other than NGHA |
||
|
Yes |
27 |
36% |
|
No |
48 |
64% |
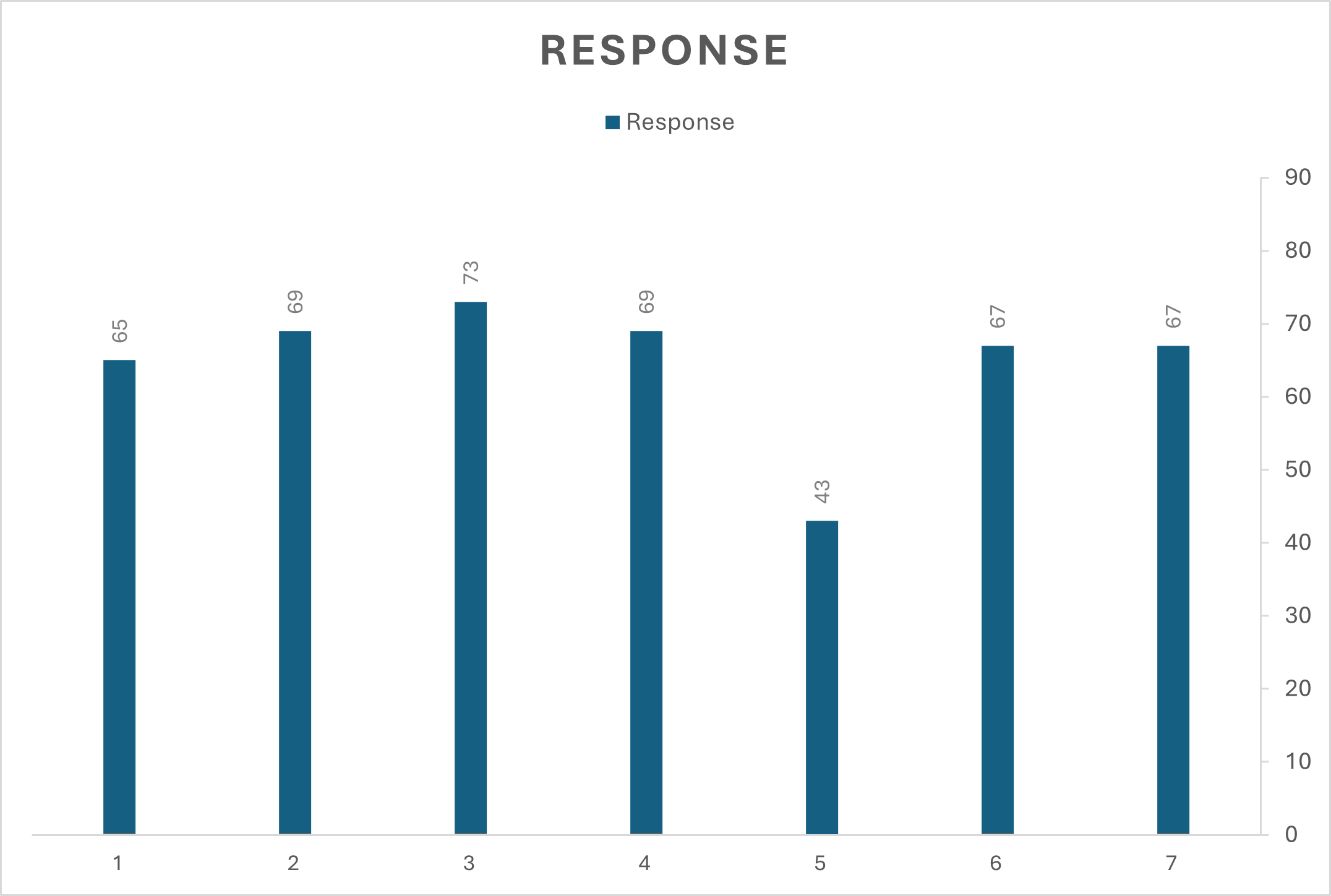
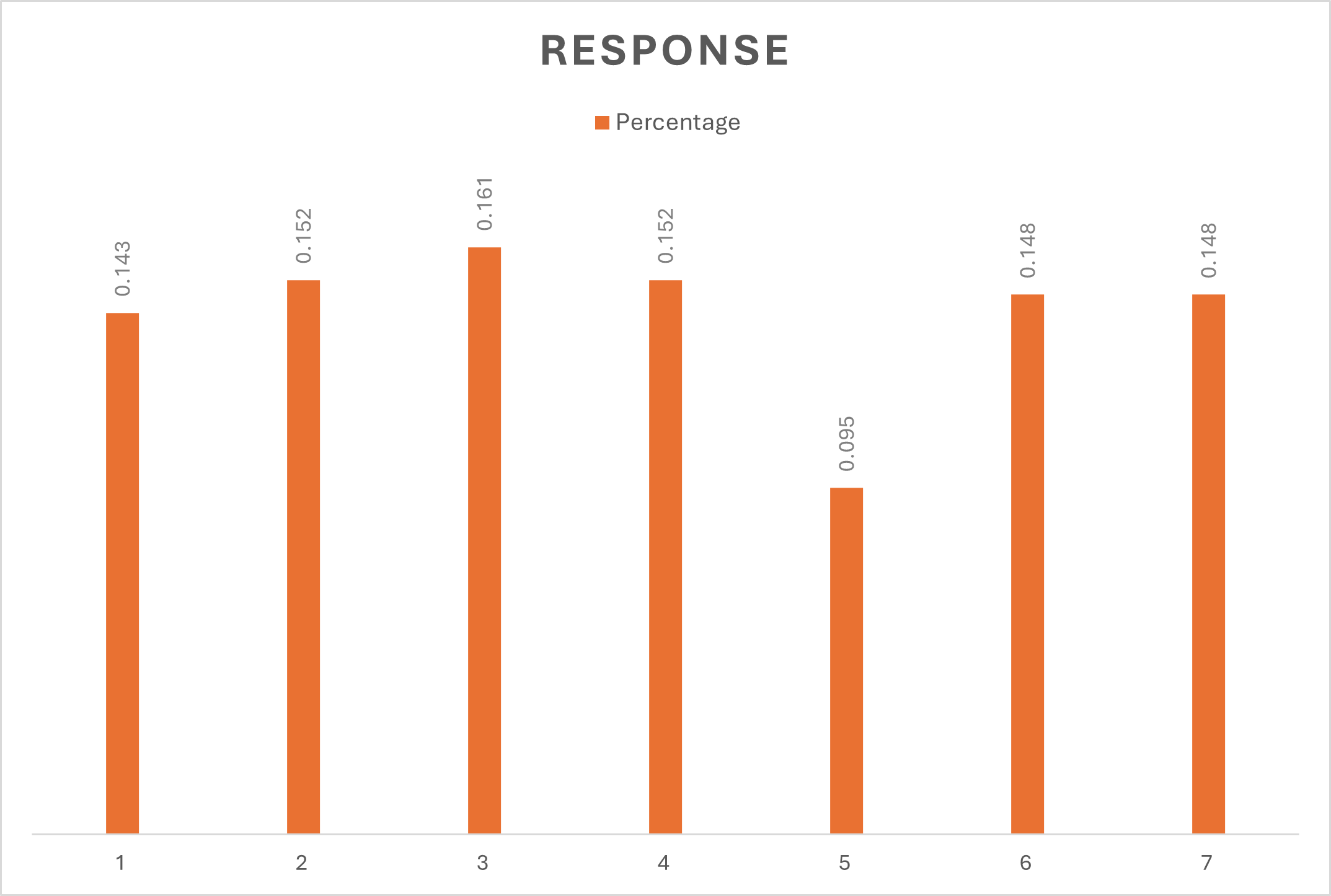
Figure 1: Multiple Responses Questions (Dipstick Test Measured Components)
|
Table 2: Knowledge and Attitude Assessment |
|||
|
Questions |
Yes |
Sometime |
No |
|
I know when urine dipstick test results are considered. |
56 (74.67%) |
19 (25.33%) |
0 (0%) |
|
I know that a urine dipstick test is mandatory for antenatal visits. |
60 (80%) |
8 (10.67%) |
7 (9.33%) |
|
There is a protocol regarding positive urine dipstick tests. |
39 (52%) |
28 (37.33%) |
8 (10.67%) |
|
I am familiar with further investigations of positive results. |
57 (76%) |
16 (21.33%) |
2 (2.67%) |
|
I feel confident about interpreting the urine dipstick test results. |
49 (65.33%) |
24 (32%) |
2 (2.76%) |
|
I know what each positive result indicates. |
50 (66.67%) |
21 (28%) |
4 (5.33%) |
|
I know when the results are considered dangerous. |
58 (77.33%) |
15 (20%) |
2 (2.67%) |
|
I am aware of both false negative and false positive results. |
26 (34.67%) |
35 (46.67%) |
14 (18.76%) |
|
I know when I should interfere according to the test results. |
49 (65.33%) |
24 (32%) |
2 (2.67%) |
|
I personally checked the results of urine dipstick test. |
47 (62.67%) |
13 (17.33%) |
15 (20%) |
|
I follow the protocol regarding positive urine dipstick test. |
54 (72%) |
17 (22.67%) |
4 (5.33%) |
|
I know when I should refer the patient to other departments. |
57 (76%) |
15 (20%) |
3 (4%) |
|
Based on positive results, I do further investigations on whether the patient is symptomatic or asymptomatic |
60 (80%) |
12 (16%) |
3 (4%) |
|
I take proper history according to the urine dipstick test results. |
69 (92%) |
6 (8%) |
0 (0%) |
|
I give enough time to read the urine dipstick test results. |
57 (76%) |
16 (21.33%) |
2 (2.67%) |
|
I refer patients after specific positive test results. |
30 (40%) |
37 (49.33%) |
8 (10.67%) |
(N=29, 38.70%) of participants will take action when positive +++ hematuria is observed. Family physicians will take action when they notice positive + in proteinuria, ketonuria, glycosuria, and leukocyte esterase. However, leukocyte esterase was accounted to have the highest number and percentage (N=36, 48%). Positive + and positive ++ were equally chosen by physicians at the rate of (N = 24, 32%) to act on albuminuria (Table 3).
|
Table 3: Attitude Assessment |
||
|
Results |
Response |
Percentage |
|
Hematuria |
||
|
Positive 1 |
21 |
28% |
|
Positive 2 |
15 |
20% |
|
Positive 3 |
29 |
38.70% |
|
Positive 4 |
6 |
8% |
|
No action will be taken |
4 |
5.30% |
|
Proteinuria |
||
|
Positive 1 |
26 |
34.70% |
|
Positive 2 |
20 |
26.70% |
|
Positive 3 |
24 |
32% |
|
Positive 4 |
4 |
5.30% |
|
No action will be taken |
1 |
1.30% |
|
Ketonuria |
||
|
Positive 1 |
29 |
38.70% |
|
Positive 2 |
23 |
30.70% |
|
Positive 3 |
15 |
20% |
|
Positive 4 |
6 |
8% |
|
No action will be taken |
2 |
2.70% |
|
Albuminuria |
||
|
Positive 1 |
24 |
32% |
|
Positive 2 |
24 |
32% |
|
Positive 3 |
16 |
21.30% |
|
Positive 4 |
4 |
5.30% |
|
No action will be taken |
7 |
9.30% |
|
Glycosuria |
||
|
Positive 1 |
28 |
37.30% |
|
Positive 2 |
13 |
17.30% |
|
Positive 3 |
24 |
32% |
|
Positive 4 |
4 |
5.30% |
|
No action will be taken |
6 |
8% |
|
Leukocyte Esterase |
||
|
Positive 1 |
36 |
48% |
|
Positive 2 |
13 |
17.30% |
|
Positive 3 |
17 |
22.70% |
|
Positive 4 |
6 |
8% |
|
No action will be taken |
3 |
4% |
Age and knowledge were associated, as the p-value was less than 0.05 using the Fisher's exact test. However, it was found that there was a non-significant relationship between age and attitude (p-value ≥ 0.05). A significant relationship was noticed between the position of family physicians and their knowledge of the urine dipstick test(p-value=0.032). However, they showed no association between their position and attitude toward the urine dipstick test results. Furthermore, it was shown that there was a significant association between experience in NGHA and knowledge(p-value=0.019). On the other hand, there was no relationship between experience and attitude taken by physicians toward the urine dipstick test results. Neither the knowledge nor the attitude of family physicians was affected in those who had experience outside NGHA (p-value ≥ 0.05) (Table 4).
|
Table 4: Demographic Variables Association with Knowledge and Attitude |
|
|
Knowledge association |
p-value |
|
Age |
0.005 |
|
Position |
0.032 |
|
Experience in NGHA |
0.019 |
|
Experience outside NGHA |
0.349 |
|
Attitude association |
p-value |
|
Age |
0.471 |
|
Position |
0.204 |
|
Experience in NGHA |
0.587 |
|
Experience outside NGHA |
0.183 |
Discussion
Urine dipstick testing is a widely used, rapid, and non-invasive screening method for detecting urinary abnormalities, and it remains a routine component of antenatal care protocols. However, family physicians' knowledge and attitudes toward interpreting dipstick test results can vary considerably. This study found that the doctors who participated in our study had achieved relatively good results, depending on their answers in the survey. Significant associations were observed between knowledge and factors such as age, professional position, and years of experience; however, no such associations were identified for attitude.
Increasing age was positively correlated with higher knowledge scores, likely reflecting cumulative clinical experience. This means that as age increases, the doctors will have better results. This might be attributed to the years of experience, as it is found clearly in the results. Conversely, younger physicians demonstrated relatively lower knowledge levels, potentially due to limited practical exposure. Similarly, the position of the doctors showed relatively the same relationship as being at an older age, implying that they have more experience and are in a higher position. Furthermore, years of experience within NGHA were significantly associated with greater knowledge, suggesting a positive influence of institutional familiarity. However, the experience of doctors outside NGHA did not show any association with knowledge and attitude, which implies that all doctors of interest have the same level of expertise regarding the knowledge and attitude toward urine dipstick test results. Also, different primary health centers (other than NGHA) provide resembling efficacy.
Regarding doctors' attitudes toward the urine dipstick test results, it was shown that there was no association with the other variables. Many doctors interpret the test results differently according to their experience and expectations, which may raise questions about how they react to the urine dipstick test results. A questionnaire-based study conducted by Braeckman et al. (24) sought to assess the utilization of routine urine dipstick urinalysis in the daily practice of Belgian occupational physicians. The study yielded comparable findings to our research, illustrating that occupational physicians often rely on established routines that may not consistently align with evidence-based guidelines. Notably, the study conducted by Braeckman et al. involved a larger cohort of 120 participants, as compared to our study with 75 participants. However, it is important to note that the Braeckman et al. study did not investigate the validity and reliability of the questionnaire employed, which may limit the comparability of findings (24). The lack of guidelines to be followed, rather than behaving according to the experience, might explain their behavior. In the present study, 32% of the participants reported uncertainty regarding the false positive and false negative rates of dipstick testing, while 2.67% admitted complete unawareness. A study showed that asymptomatic pregnant women who underwent screening for UTI were correlated with false positives and false negatives stated by Demilie et al (18). The accuracy of the dipstick urinalysis with a 1+ threshold in prediction of significant proteinuria is poor, so it is considered of limited usefulness to physicians (25). Therefore, their level of knowledge influenced their attitude toward urine dipstick test results. Furthermore, leukocyte esterase is one component that significantly helps detect UTI.
Similarly, the present study revealed that physicians frequently initiate clinical actions upon observing positive dipstick results, particularly in cases with leukocyte esterase positivity, indicative of urinary tract infection. Additionally, most doctors claim they know when the urine dipstick test is dangerous. Preeclampsia remains one of the major hazardous complications in pregnancy, characterized by high blood pressure and multiple severe conditions like neurological complications, liver dysfunction, and thrombocytopenia. Proteinuria detected via dipstick testing serves as a key diagnostic criterion (26). The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) suggest only screening for preeclampsia in high-risk pregnant women (27, 28). Interestingly, most family physicians in NGHA choose to take further investigations on whether the patient is symptomatic or not, demonstrating a cautious and proactive clinical approach. A prospective observational study indicates that the diagnostic threshold for proteinuria in preeclampsia may need to be set higher, and highlights the necessity for a standardized gold-standard assay to ensure accurate measurement and comparability across different testing methods (29).
Despite ACOG and USPSTF guideline recommendations, some clinicians advocate for universal screening—even among low-risk populations—given the test's simplicity and potential to detect early pathology. There is variation in the decision of taking further investigations regarding the level of the positivity, for example, +, ++, +++, +++++ or not taking any actions. Physicians should keep up to date with changes in the medical field using evidence-based medicine, as it displays its effectiveness in improving the quality of care in the medical field (30, 31). In addition, it supports the more efficient establishment of clinical guidelines aimed at reducing avoidable complications.
Limitations and strengths
Despite the good response rate of the participants, a higher percentage of them were residents, which might have affected the representativeness of the population. Also, the number of 75 participants may not represent the population in Saudi Arabia, so selection bias may be introduced. Additionally, as a self-developed questionnaire was used, the possibility of report bias may be introduced. Furthermore, the lack of similar previous studies to compare was a significant challenge. On the other hand, great effort was made to ensure the validity of our self-developed questionnaire. Also, it is considered one of the few studies on this topic, and it is believed that this research will provide opportunities to establish more research in this regard.
Conclusion
It is found that family physicians usually behave according to their experience and expectations, which may not be aligned with evidence-based medicine today. Workshops can be held to clarify the effectiveness of using evidence-based medicine in the medical field. Furthermore, medical colleges should make greater efforts to reinforce the importance of implementing evidence-based medicine in future doctors. Again, additional research in this field is necessary to better understand doctors' behavior in medicine. This could help develop specific guidelines that will considerably benefit the medical field.
Acknowledgments
The authors would like to thank everyone who contributed to this research, especially Dr. Mohammad Aldgair, for his contribution to data analysis. Also, prof. Dr. Lutgart Braeckman who had provided helpful suggestions regarding the questionnaire development.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical consideration
Ethical approval for this research was received from the Institutional Review Board of King Abdullah International Medical Research Center (KAIMRC), IRB number: IRB/0729/22, on Apr 5, 2022.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.