Volume 2, Issue 9
September 2022
Classification of Post-Mortem Changes and Factors Affecting It
Abdulaziz Emam, Hani Mujalid, Noora Altamimi, Weaam Faraj, Meshari Almutairi, Zayed Alresheedi, Rinad Ergsous, Abdulrahman Qadah, Nourah Al Modahka, Abdulaziz Alzahrani, Haya Alkhamis, Abdullah Alassiri
DOI: http://dx.doi.org/10.52533/JOHS.2022.2901
Keywords: post-mortem, change, death, factor, forensic medicine
An autopsy is not simply the patient's last medical intervention but in addition to determining the cause of death, it also provides information about the deceased patient's underlying health. The natural process of the body's breakdown following death, starting at the cellular level, is known as post-mortem change. Complex cellular and biochemical phenomena are involved in the process. The changes that begin right away after death continue for a considerable amount of time at various rates for various organs. Numerous intrinsic and extrinsic factors have an impact on the beginning and severity of these changes. The purpose of this research is to review the available information about classification of post-mortem changes and factors affecting it. Post-mortem changes are further divided into three classes, Immediate changes, early changes and late changes. After cardiac and respiratory failure, early post-mortem changes including rigor mortis and post-mortem lividity occur. However, tissue metabolism continues for a few hours after death. Supravital reactions, time-dependent post-mortem lividity, and rigor mortis criteria are used to estimate the time since death. Estimating the post-mortem interval or time since death, is one of the main aims of the forensic autopsy, requires an understanding of post-mortem changes. Many exogenous and endogenous factors can lead to degradation. Animal predation, the environment, and mechanical injury are extrinsic causes, whereas autolysis, putrefaction, and decay are endogenous factors. However, despite the importance of post-mortem findings the literature available is very limited more research in future can be a significant contributor.
Introduction
Autopsies are essential in medicine and are critical in confirmation of the clinical diagnosis, medical education, and quality control. For the benefit of the patient, a proper diagnosis is vital, as are statistics on morbidity and death. In order to match the clinical diagnosis with the post-mortem results, hospital autopsies which are regarded as the gold standard for establishing a conclusive diagnosis are frequently used. Although diagnostic techniques have advanced significantly, ante- and post-mortem diagnoses are different. Autopsy is not only the patient's final medical treatment; in addition to identifying the reasons of death, but it also sheds light on the underlying condition of the patient who has passed away. Clinical autopsies require either the deceased's antemortem consent or the family' post-mortem consent which is in contrast to forensic autopsies (1). The majority of clinicians and pathologists continue to view autopsies as necessary, with discrepancy rates between premortem and post-mortem diagnoses remaining constant over the years at around 10%. The autopsy rate can be raised by upholding standards for conducting and documenting autopsies. On the legislative front, adjustments are being made so that autopsy is acknowledged as a tool for quality control and guidelines are established for better monetary recompense. Numerous post-mortem examination procedures are currently available; however they cannot replace traditional autopsies (2).
Various bodily changes that take place after death are referred to as post-mortem changes. These changes may be crucial in determining or confirming the time of death, hinting at the manner or cause of death, or indicating that a body may have been transferred after passing away. The degree of rigor mortis, the degree, location, colour, and nature blanching vs. fixed of livor mortis, as well as the presence or absence of decompositional changes, should all be noted at each external inspection (3). Artifacts are introduced to the body by post-mortem changes that a forensic pathologist must discern from trauma. Additionally, these post-mortem changes may conceal real trauma. Although it may seem contradictory, the skeleton, and more specifically the timing of fractures, is one region of the body where post-mortem changes impact the precise assessment of injury (4). The purpose of this research is to review the available information about classification of post-mortem changes and factors affecting it.
Methodology
This study is based on a comprehensive literature search conducted on August 1, 2022, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the information about the classification of post-mortem changes and factors affecting it. There were no restrictions on date, language, participant age, or type of publication.
Discussion
The biological processes of dying and death are ongoing. The majority of the time, the irreversible loss of respiratory and circulatory functions is the cause of a person's death. Early post-mortem changes such post-mortem lividity and rigor mortis come after cardiac and respiratory failure. Tissue metabolism, however, continues for a number of hours after death. Tissue responses to excitation during this supravital phase resemble those of living things. The time since death is determined using supravital reactions as well as the time-dependent post-mortem lividity and rigor mortis criteria. Devastation and decay are caused by a variety of external and endogenous sources. Autolysis, putrefaction, and decay are endogenous factors, whereas animal predation, the elements, and mechanical injury are extrinsic causes. While these organic processes cause the cadaver to dissolve and disintegrate down to its bones and tendons, some environmental factors may help preserve a body. Mummification and adipocere production are examples of preservation techniques. Wet and frozen bodies can also contain it (5).
Classification of post-mortem changes
The post-mortem modifications can be categorized as immediate changes, early changes, and late changes depending on when they first appeared.
Immediate Changes
The term somatic death or systemic death refers to alterations that occur right after death. The permanent loss of the heart, lungs, and brain functioning is known as somatic death. The immediate post-mortem changes are referred as the signs or symptoms of death. Insensibility, the loss of voluntary movements, the cessation of respiration and circulation, and the cessation of nervous system operations are among the immediate changes. Primary muscular relaxation takes place at this period. Although insensibility and loss of voluntary movement are among the first signs of death, these symptoms can also be present in cases of electrocution, hypnosis, fainting episodes, narcosis, and catalepsy, among other causes (6).
Early Changes
Rigor mortis, livor mortis, algor mortis, and corneal dryness are early post-mortem changes. The term rigor mortis refers to the post-mortem contraction of muscles caused by the locking of actin-myosin filaments as a result of lowered adenosine triphosphate production (7). Both voluntary and involuntary muscles are affected by rigor mortis, which causes hardening of the joints. First there is a flaccidity, which then starts in the jaws, moves to the upper extremities, and then to the lower extremities. As actin-myosin connections get denaturized during the early stages of decomposition, rigor mortis persists for a varied amount of time before waning and finally disappearing. The pattern of the beginning and the disappearance will be similar. Livor mortis begins when the blood stops flowing through the capillary bed and the related smaller afferent and efferent vessels because arterial propulsion and venous return are unable to maintain blood flow. The now-stagnant blood is subsequently affected by gravity, which drags it to the lowest accessible places. Lividity is first noticeable 20 minutes to 4 hours after death, with discolouration peaking between 3 and 16 hours later. With a change in body position at fixation, lividity does not change. Algor mortis or bodily heat loss can occur by four mechanisms: Evaporation, radiation, conduction and convection. The environment will cause a decrease in body temperature. The tache noir, which is frequently seen in cadavers with the eyes open and the exposed portion of the cornea drying out, is another early post-mortem alteration.

Figure 1: Livor mortis or lividity on the posterior aspect of the body (3).
The post-mortem alterations from various processes that are relevant for calculating the time since death are: Physical, metabolic, physiological, physical-chemical, bacterial, putrefaction, autolysis which is loss of selective membrane permeability, diffusion, and insect activity are examples of physical phenomena (8-10). Livor mortis or lividity on the posterior aspect of the body is shown in (Figure 1) (3). Tache noir of the eyes from post-mortem drying is depicted in (Figure 2).

Figure 2: Tache noir of the eyes from post-mortem drying (3).
Late Changes
Putrefaction and autolysis are the two mechanisms that contribute to decomposition. Autolysis marks the beginning of decomposition shortly after death, whereas putrefaction marks the beginning of the macroscopic changes brought on by decomposition. The process of autolysis is brought on by the hydrolytic cellular enzymes that leak out of dead cells. The majority of the changes that take place throughout this process are microscopic rather than macroscopic. Internally, the pancreas and other organs with a high concentration of cellular enzymes are where autolytic alterations are most noticeable. The prostate and the non-gravid uterus degrade more slowly than other organs. The putrefaction process, which is the breakdown of surrounding tissues by microbes such bacteria, fungus, and protozoa that are typically found in the human microbiota, is facilitated by the release of cellular contents. In contrast to autolytic alterations, putrefactive changes manifest macroscopically as skin discoloration or swelling in areas of the body such the face, abdomen, breasts, and scrotum. It can manifest itself in a variety of ways, including putrifiable fluids and putrifiable gases (11-14). Figure 3 shows body in fresh stage of decomposition (15).

Figure 3: Body in fresh stage of decomposition (15).
Kemp stated that post-mortem changes can both conceal and mimic trauma, making it more difficult to assess the injuries. Bones are not immune to these effects, despite being able to survive the post-mortem period relatively unharmed. It might be challenging to pinpoint the time when a fracture occurred if there is no associated soft tissue to provide an examination with guidance. Both organic and inorganic components that make up bones each add to the biomechanical characteristics of the bones. The biomechanical response of bones to trauma alters when biological material is lost, but organic material can stay in the bone for a long time after death. Wet bone is defined as having intact biological content, whereas dry bone does not. As a result of this distinction, fractures in wet bone may not look exactly like those in dry bone. Differential colouring, the fracture's individual characteristics such as its angle, surface, and contour, the cortex's surrounding flakes, and the inadequate separation of bone fragments from the fracture are all essential in separating the two. The two types of fractures can be hard to distinguish since the changes are not absolute (16).
Sauvageau A stated in his study findings that post-mortem changes are notable for their potential to be mistaken for traumatic lesions, which can falsely raise suspicions of a violent demise and, as a result, lead to a request for a forensic autopsy. Post-mortem artifacts misinterpreted for traumatic lesions were discovered in 18 of the 230 cases that were analysed. These erroneous conclusions were drawn from five categories of post-mortem changes: purge fluid drainage in 12 cases (66.7%), bluish discoloration from lividity in 5 cases (27.8%), parchment-like skin drying in 4 cases (22.2%), bloating from gas formation in 4 cases (22.2%), and skin slippage in 1 case (5.56%). Therefore, of all requested forensic autopsies, post-mortem artifact misinterpretation happened in 7.83 % (95% confidence interval 0.05–0.12) and in 35.29 % (95% confidence interval 0.23-0.50) of decomposed autopsy cases (17).
Levy described that in order to enhance forensic autopsies, multidetector computed tomography (MDCT) has proven to be a successful imaging technology. Post-mortem change and decomposition are always visible at autopsies and on post-mortem MDCT since they appear right away. Therefore, it is important to distinguish post-mortem change and decomposition on post-mortem MDCT and to avoid mistaking them for a pathogenic process or trauma. Livor mortis causes the vasculature and dependent tissues' MDCT attenuation to rise. The fluid levels in the large caliber blood arteries and heart chambers caused by dependent stacking erythrocytes may also have an impact on haematocrit levels. Algor mortis and rigor mortis lack any distinctive MDCT characteristics. Contrarily, decomposition brought on by autolysis, putrefaction, and animal and insect predation results in pronounced changes in the body's appearance on MDCT. The attenuation of organs is altered by autolysis. The brain exhibits the most pronounced autolytic alterations on MDCT, where gray-white matter distinction is lost practically quickly after death and cerebral sulci and ventricles are effaced. Intravascular gas is produced by putrefaction, followed by gaseous distension of all anatomical spaces, organs, and soft tissues. The interpretation of post-mortem MDCT requires an understanding of the range of post-mortem alteration and decomposition (18). Post-mortem computed tomography scan of the deceased shows intracranial gas fluid and skin slippage (19) (Figure 4).
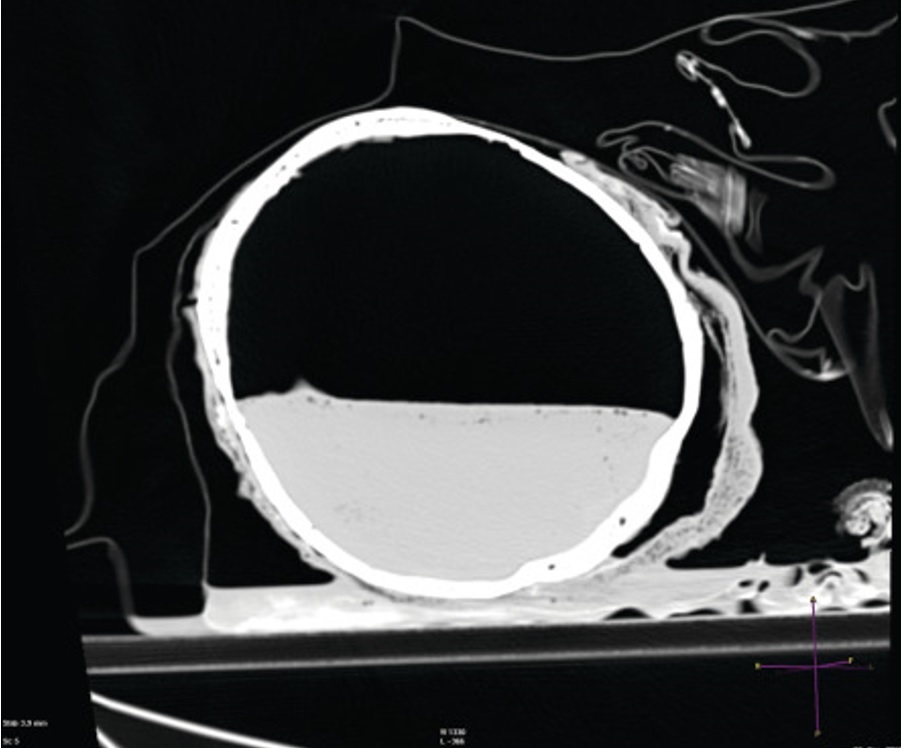
Figure 4: Post-mortem computed tomography scan of the deceased shows intracranial gas fluid and skin slippage (19).
Factors affecting post-mortem changes
In general, post-mortem changes happen in a predictable order of increasing stages of degeneration. However, there are significant variances because of a wide range of influencing factors originating from both the environment and the human body itself. Changes caused by the human body itself are referred as intrinsic factors while changes due to environment are extrinsic factors. Body mass and surface area are intrinsic determinants, but there are also others like age, sex, antemortem disease, the presence of wounds or trauma, the amount of bacterial activity, and the reason for death. Extrinsic features include the kind and amount of clothing and other body insulation, as well as the environment surrounding the death scene, including temperature, wetness, air flow intensity, depth of burial, and insect and microbial activity (20). Although post-mortem findings have a pivotal role especially in predicting the cause of death and time of death in unknown cases still the literature is quite scarce and limited more research in future will not only aid in contributing to literature but also help in developing strategies to control factors affecting these changes so more accurate and reliable post-mortem findings are reported.
Conclusion
Post-mortem findings are helpful in revealing the reason and manner of death. The post-mortem changes are influenced by a variety of internal and external causes. Further research by forensic researchers is need of time for better knowledge and understanding of post-mortem changes and factors responsible for it.
Disclosure
Statement
The authors declare no conflict of interest.
Funding
No funding.
Ethical consideration
Non-applicable.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Authors’ contribution
All authors contributed equally to the drafting, writing, sourcing, article screening and final proofreading of the manuscript.
