Volume 5, Issue 9
September 2025
Safety and Efficacy of Regional Blocks in Pediatric Day Surgery Procedures
Talal Sulaiman Alrumaihi, Abdullah Ahmed Ghunaim, Jameel Hosni Amoudi, Mohammed Sameer Alqabli
DOI: http://dx.doi.org/10.52533/JOHS.2025.50901
Keywords: safety, efficacy, regional blocks, pediatric, children, day surgery, procedures
Pediatric day surgery is increasingly recognized worldwide, attributed to its lower costs, reduced disturbance, and abbreviated hospital stays. Addressing surgical pain is crucial in encouraging immediate recovery, achieving discharge criteria, and ensuring parental satisfaction. Perioperative analgesia in pediatrics is based on the use of regional anesthesia to target pain and reduce the dose of opioids that are used systemically as well as the side effects of those opioids. This narrative review summarizes the recent regional block safety and efficacy evidence for pediatric day surgery. Caudal, peripheral nerve, and fascial plane blocks are prioritized. Recently, conducted research has demonstrated that regional anesthesia is more effective than systemic anesthesia in managing pain. Regional anesthesia effectively manages pain, reduces reliance on opioid pain medications, and offers a longer duration of pain relief. The reduction of nausea, vomiting, sedation, and other opioid-related side effects is an advantage of regional anesthesia that speeds up the milestones associated with discharge. Regional blocks for children are safe and effective in reducing the risk of complications when performed by clinicians who have received professional training, especially with ultrasound assistance, which improves anatomical visualization. In pediatric day surgical procedures, regional anesthetic improves patient comfort, recovery quality, and parental satisfaction in outpatient care. Selection of the right block depends on surgical site, patient age, and expertise. To maintain high standards of care, institutions must support training, pediatric-specific equipment, and safety protocols. This review aims to provide an updated synthesis of regional block safety and efficacy in pediatric day surgery to enable anesthesiologists to make evidence-based decisions. Future research should include pediatric-specific trials of emerging fascial plane blocks, long-acting local anesthetics, and regional anesthesia in enhanced recovery after surgery (ERAS) pathways. These advances may improve outcomes, reduce opioid exposure, and expand regional techniques in pediatric ambulatory anesthesia.
Introduction
Outpatient surgeries for children have advanced due to minimally invasive techniques, enhanced monitoring, and optimized recovery programs. Day surgery reduces the expenses of healthcare, increases patient satisfaction, and decreases the number of hospital-acquired infections and family conflicts (1). Reduced hospital stays correlate with less perioperative anxiety and enhanced surgical recovery trajectories in pediatric patients (2). Perioperative planning and discharge criteria must be strict due to limited observation time and to avoid complications that lead to unplanned hospitalizations and delayed discharge (3).
Anatomical, physiological, pharmacokinetic, and psychological factors restrict pain management in pediatric patients. Premature myelination of nerve pathways has an impact on both the pharmacodynamics of local anesthetics and the perception of pain (4). Immature enzyme systems may prolong drug half-lives in neonates and infants due to increased hepatic metabolism that may impair medication efficacy in older children (5). Psychological factors, such as preoperative anxiety and previous healthcare experiences, substantially impact pediatric pain perception (6). For pediatric day surgery, multimodal analgesia includes regional anesthetic, acetaminophen, NSAIDs, parental presence, distraction, and age-appropriate communication (7).
Caudal epidural blocks are the most common regional technique used for pediatric patients. Their popularity arises from their ease of administration, high success rate, and applicability to interventions concerning the lower limbs, perineum, and lower abdomen (7). Ultrasound guidance is becoming more popular; however, the utilization of this technology is limited by equipment and operator proficiency, practically in low-resource settings (8). Abdominal surgery typically uses Transversus Abdominis Plane (TAP) and ilioinguinal/iliohypogastric (II/IH) nerve blocks (9). Regional anesthesia is used independently for short operations or with general anesthesia to reduce intraoperative anesthetic demands and improve recovery (10).
In pediatric day surgery, regional blocks must be evaluated for safety and efficacy. Quality and duration of postoperative analgesia, opioid-sparing effects, enhanced recovery profiles, and same-day discharge are indicators of efficacy (11). Day surgery requires rapid recovery without motor blockade or sedation. Postoperative motor weakness may delay ambulation, prolong discharge readiness, and elevate fall risk, particularly in younger pediatric populations (12).
Regional anesthetic is increasingly used in pediatric day surgery; the utilization of this technology is limited by equipment and operator proficiency. The analgesic efficacy of regional blocks has been studied in several randomized controlled trials and observational studies; however, its dose, block duration, and complication rates across various age demographics remain inconsistent (13). Multiple regional anesthesia exposures in early childhood may affect neurodevelopment, raising long-term safety concerns. In pediatric patients, especially day-case patients, the evidence base for emerging blocks like erector spinae plane (ESP) or quadratus lumborum (QL) blocks is limited (14). This review aims to synthesize the safety and efficacy of regional blocks in pediatric day surgery and focus on commonly used techniques, clinical outcomes, and risk profiles. The main objectives of our article review are to describe the methods and indications of regional anesthesia for pediatric day surgery. We should consider recovery time, opioid sparing, and analgesic efficacy. It is important to consider complications and monitoring. Locate knowledge gaps and suggest research priorities. This review will provide anesthesia providers with an evidence-based framework for integrating regional anesthesia into pediatric day surgery pathways to enhance patient outcomes and safety by consolidating current literature and clinical experience.
Methodology
A comprehensive literature search in PubMed, Web of Science, Science Direct, and Cochrane databases utilizing the medical topic headings (MeSH) and relevant keywords such as ‘safety’, ‘efficacy’, ‘regional blocks’, ‘pediatric’, ‘children’, ‘day surgery’, ‘procedures’, and a combination of all available related terms was performed on August 10, 2025. All relevant peer-reviewed articles involving human subjects and those available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, or participant age.
Discussion
Overview of Regional Blocks in Pediatric Anesthesia
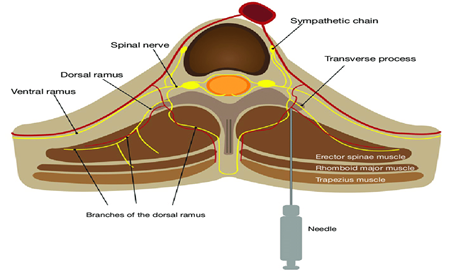
Regional anesthesia provides targeted pain control and high safety in pediatric day surgery. Caudal, peripheral nerve, and fascial plane blocks are the most common types (15). Caudal blocks dominate pediatric lower abdominal, pelvic, and lower limb surgery. Through the sacral hiatus, this neuraxial block dermatome pain signals by injecting local anesthetic into the caudal epidural area. It provides numerous advantages because of its predictable anatomical features, uncomplicated execution, and established reduction in postoperative analgesic requirements however, side effects, such as motor blockade, urinary retention, and single-shot duration influence its selection in ambulatory settings (16). Femoral, sciatic, brachial plexus, and popliteal nerve blocks are possible peripheral nerve blocks (17). Depositing local anesthetic near nerves or plexuses inhibits nociceptive signal transmission, providing targeted analgesia to the surgical field. (18). Peripheral nerve blocks can provide prolonged pain relief for pediatric day surgery patients without the need for opioids or systemic sedation. Fascial plane blocks, including TAP, ESP (Figure 1), and QL blocks, are increasingly popular techniques that involve depositing local anesthetic within fascial planes to anesthetize multiple segmental nerves, offering an indirect method of nerve block that reduces nerve stress (19). This indirect method reduces nerve stress and encompasses stomach, thoracic, and spine surgeries. These blocks are appealing pediatric ambulatory practice due to their simplicity, adaptability, and ultrasound compatibility. Consequently, pediatric regional anesthesia blocks are associated with particular anatomical targets, therapeutic applications, and processes (20). Caudal, peripheral nerve, and fascial plane analgesia are safe, effective, and procedure-specific due to surgical, patient, and institutional knowledge (21).
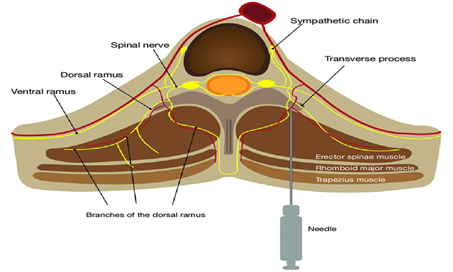
Figure 1: Schematic diagram of erector spinae plane block (22).
Analgesic Efficacy and Opioid-Sparing Benefits
Pain management is essential for pediatric day surgery recovery, discharge, and patient satisfaction. These blocks are crucial to multimodal analgesic techniques for intraoperative and postoperative pain management, according to growing studies (2). Caudal blocks are the standard for postoperative analgesia in lower abdominal, pelvic, and lower leg surgeries, as they have been thoroughly investigated (23). Analgesia can be extended safely with adjuvants like clonidine or dexmedetomidine. Their efficacy is restricted in procedures above the umbilicus, and motor block may impede ambulation (24). For orthopedic and upper or lower limb procedures, peripheral nerve blocks provide regional analgesia with long-term pain control. Day surgery rarely uses continuous catheter procedures, but they can extend analgesia. Fascial plane blocks are helpful for pain management for abdominal, thoracic, and spine procedures (Figure 2) (19). In pediatric hernia repair, appendectomy, and other abdominal surgeries, the TAP block reduces discomfort and narcotic use (25). ESP and QL blocks achieve broad dermatomal coverage with lower postoperative pain scores than typical infiltration procedures. They are useful in ambulatory settings due to their ease of administration and low complication rates (26). Finally, localized blocks provide predictable, procedure-specific analgesia for pediatric day surgery, surpassing systemic therapies. In this population, they are first-line multimodal pain management components because they speed recovery, maintain low pain levels, and restrict opioid consumption (27). In lower abdominal and urogenital procedures, caudal blocks sustain reduced pain levels for several hours post-surgery, facilitating the prompt initiation of oral intake in infants and ensuring hydration prior to discharge (28). Orthopedic day surgery requires peripheral nerve blocks for long-term site-specific analgesia and early limb mobility and rehabilitation. Reduced intravenous analgesics reduce recovery room interventions, streamlining perioperative procedures (29). Studies indicate that parents who receive clear surgical instructions and observe minimal child distress have enhanced discharge acceptance and satisfaction rates (30). Early release with stable vital signs, pain control, oral intake tolerance, and safe ambulation minimizes hospital stays without compromising patient safety. Regional blocks improve patient outcomes and healthcare systems in modern pediatric ambulatory anesthesia. Pediatric discharge coordinators can start feeding promptly since opioid-sparing maintains gastrointestinal motility and decreases surgical nausea and vomiting (31). Pediatric opioid adverse effects include drowsiness, coughing, nausea, vomiting, itching, urine retention, and respiratory depression. Parents are concerned that the side effects of opioids may delay discharge, create complications, and hinder healing (32). Regional blocks minimize perioperative opioids, improving safety, recovery, and ambulatory surgery goals. Clonidine and dexmedetomidine adjuncts prolong analgesia, diminishing postoperative opioid consumption. Avoiding opioid use at home is important in the ambulatory situation; therefore, this extended pain control is beneficial (33). Systemic analgesics can be eliminated for a period of 12–24 hours following surgery through the use of brachial plexus blocks in the upper limb and femoral nerve blocks in the lower leg (34). Maintaining cognitive awareness and reducing sedation helps children resume routines and satisfy discharge readiness standards faster. Patients have fewer opioid-related adverse effects, including gastrointestinal disturbances, which sometimes delay oral intake in children (34). Reducing perioperative opioid exposure is beneficial to global efforts to reduce opioid usage because of the long-term hazards associated with opioid use. The attempt encompasses efforts to prevent opioid utilization in pediatric populations. In pediatric day surgery, localized blocks reduce systemic opioid use (35). This enhances postoperative safety, recovery, and pediatric opioid exposure compliance.
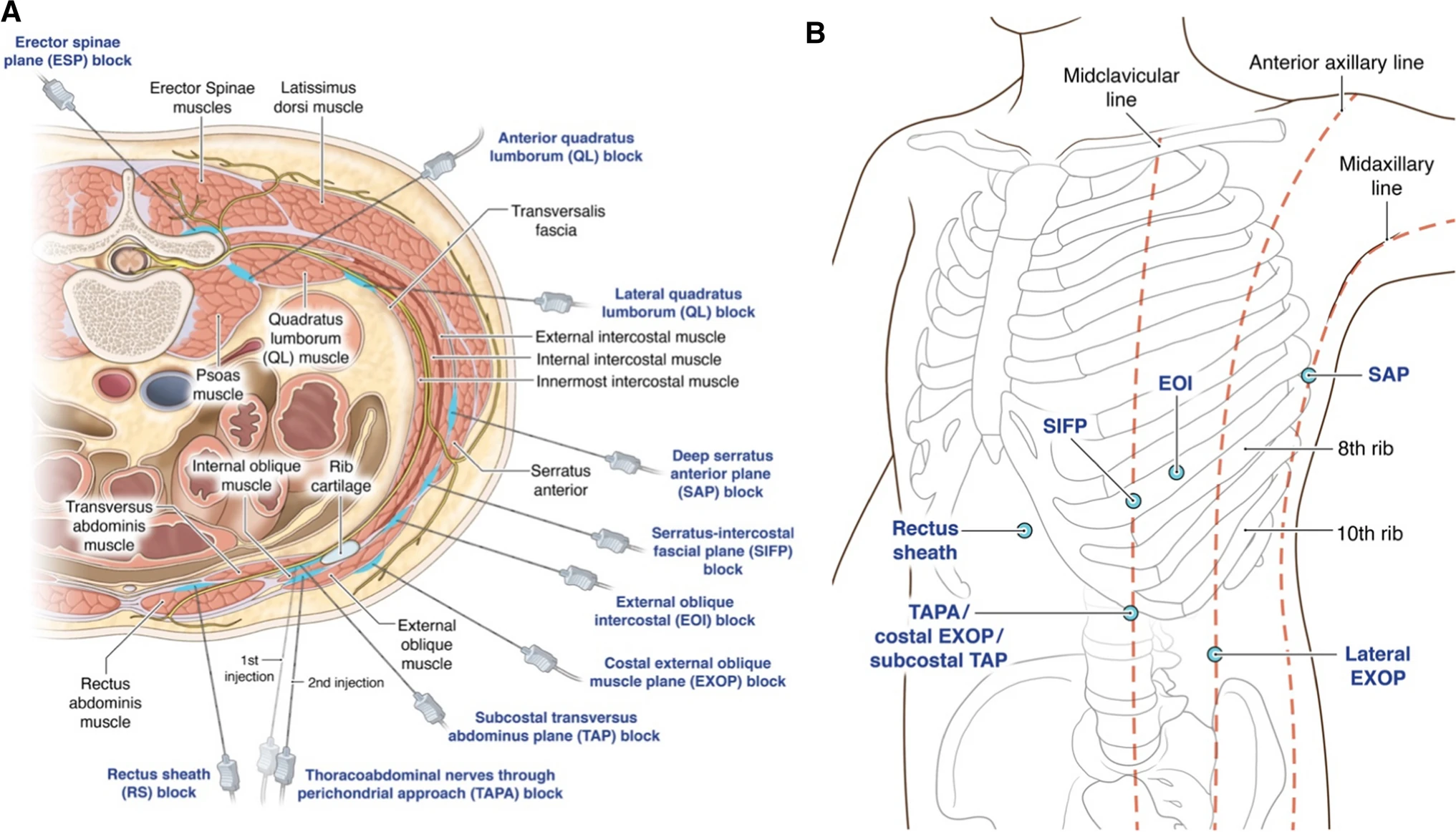
Figure 2: Injection points of fascial plane blocks for the abdominal wall (36).
Safety Profile and Complication Rates
Clinical use of regional anesthesia in pediatric day surgery depends on safety. Although major problems are rare, children's anatomical and physiological differences require a careful approach, medicine administration, and monitoring (37). Caudal blocks are generally safe; nonetheless, they may result in dural puncture, intravascular injection, infection, and urinary retention. Most minor complications, such as transitory motor blockage or delayed micturition, disappear without treatment. LAST can be avoided by following weight-based dosing (38). Similar adverse effects are rare with ultrasound-guided peripheral nerve blocks. In contrast to landmark-based approaches, real-time imaging directly visualizes nerves, arteries, and needle trajectory, decreasing nerve injury and vascular puncture (39). Ultrasound guidance significantly enhances the safety and effectiveness of nerve blocks by providing real-time visualization of needle placement and local anesthetic distribution (40). Moreover, ultrasound guidance increases the accuracy and safety of various peripheral nerve blocks, such as femoral, sciatic, brachial plexus, and popliteal nerve (17), enabling precise visualization of anatomical structures, reducing local anesthetic volumes, and reducing the risk of vascular puncture or nerve injury (18). Additionally, it enhances block precision and reduces vascular puncture and nerve injury and is specifically required for appendectomy, hernia, and other abdominal surgeries. Recently, high-resolution portable ultrasound equipment has become more common, allowing precise imaging of little patients. 3D ultrasonography and real-time needle monitoring are being researched to improve accuracy and reduce complications (41). Sensory or motor impairments after surgery normally resolve, however, in rare situations, neurological effects persist, emphasizing the significance of proper technique and avoiding high-pressure injections (42). This indirect approach renders face plane blocks among the safest regional methods for children, as nerve damage and intravascular injection are rare since the needle is away from important nerves and blood arteries (43). Local hematoma and insufficient analgesia due to incomplete diffusion of local anesthetic are rare and minor consequences; this risk is mitigated by precise determination of maximum safe doses, gradual injections with aspiration, and the quick accessibility of lipid emulsion therapy (44). Overall, regional blocks in pediatric day surgery are safe when delivered by experienced clinicians using contemporary imaging. These perioperative pain treatment methods are considered successful because complications are rare, typically minor, and can be prevented by adhering to established safety measures (45). Safety evaluation reduces Local anesthetic systemic toxicity (LAST), nerve injury, bleeding, and infection risk factors. Children are prone to LAST due to decreased protein binding, increased cardiac output, and different body composition. Thus, careful intraoperative monitoring, age-appropriate dosing, and gradual injection are necessities (46). These variables make them susceptible to LAST and necessitate weight-based dose calculation.
Age-Specific Considerations
Age influences the selection, administration, and effectiveness of regional anesthesia in pediatric outpatient surgery. Pediatric patients have unique anatomical proportions, physiological sensitivities, and developmental phases that affect block selection and local anesthetic dosage (47). (48). The distribution and duration of drugs are influenced by the compliance of the epidural space and the elevated amount of cerebrospinal fluid (49). This age group benefits from ultrasound assistance for visualizing anatomical structures and decreasing problems. Infant organ systems are immature; however, they exhibit greater stability than those of newborns. However, their modest anatomical dimensions require careful needle placement and conservative drug doses (49). Infraumbilical surgeries in this age group often involve caudal blocks for predictable dissemination and adequate analgesia. Balancing analgesia with functional recovery is important since newborns are sensitive to motor blockage and could delay mobilization (50). Children of school age exhibit a high tolerance for localized anesthetics and demonstrate consistent pharmacokinetic profiles (50). The surgical site, anticipated pain trajectory, and patient-specific factors dictate the method that optimizes analgesia while minimizing systemic side effects (51). Anesthesiologists must tailor analgesia to age, weight, cognition, and development. Since peripheral nerve blocks provide extended site-specific analgesia with minimal systemic influence, they are becoming beneficial for orthopedic day surgery (52). Communicating block placement and expected sensations with the child can enhance participation and procedure success. Pediatric and adult anesthetic factors overlap in adolescents. Maximum safe limits apply to adult doses, even if larger bodies require more local anesthetic. Anatomical and physiological characteristics unique to age influence regional anesthesia in pediatric day surgery (53). For safety and efficacy, age-specific methods are essential, due to incomplete hepatic metabolism, plasma protein binding, and nerve myelination, neonates present unique problems.
Emerging Techniques and Future Directions
Technological advances, pain physiology knowledge, and the search for safer, more effective analgesics are advancing pediatric regional anesthesia. In pediatric outpatient surgery, many innovative methods and technologies can improve regional block safety, efficacy, and accessibility (10). Novel fascial plane blocks are becoming more popular due to their versatility and low risk. ESP, QL, and PECS blocks are being developed for pediatric applications, thereby expanding the scope of regional anesthetics. Instead of direct nerve contact, their indirect approach utilizes fascial compartments to distribute anesthetic for multi-dermatomal analgesia, ensuring safety (54). Early studies suggest equivalent or enhanced pain control compared to standard approaches in certain procedures; however, pediatric-specific trials are needed to determine optimal dose and indications (55). Imaging technologies are altering pediatric regional anesthesia. These advancements may enable a higher number of practitioners to perform complex nerve blocks. Prolonged-acting local anesthetics and novel delivery mechanisms signify a new frontier. Liposomal formulations and sustained-release delivery systems can prolong analgesia beyond single-shot methods, encompassing the entire postoperative duration in day surgery without the need for catheters (56). This would reduce opioid use and simplify home postoperative care. Pediatric regional anesthetic abilities are improving with digital and simulation-based training. Virtual reality simulators and interactive anatomical models accelerate learning by letting trainees practice needle guidance, probe manipulation, and anatomical recognition without patient danger (57). In ambulatory surgery, developing block techniques and evidence-based perioperative care regimens can improve outcomes and efficiency (58). Finally, block techniques, imaging, drug distribution, and training will change pediatric day surgery regional anesthesia. Further studies are required, especially including pediatrics, to guarantee the safety, efficacy, and broad implementation of these findings.
Conclusion
According to the existing evidence, regional anesthesia is indeed a safe and beneficial part of multimodal pain management in pediatric day surgery, providing better pain relief, minimizing opioid use, and promoting faster recovery compared to relying solely on systemic pain medications. Caudal, peripheral nerve, and fascial plane blocks offer distinct advantages for pain management, with ultrasound guidance enhancing their precision and safety. Optimizing dosage regimens, standardizing novel methods, and assessing long-term outcomes are essential goals for future research. Careful intraoperative monitoring, age-appropriate dosing, and gradual injection are necessities. Expanding high-quality pediatric studies will strengthen the evidence base and support broader integration of regional anesthesia in ambulatory pediatric practice.
Disclosures
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical considerations
This study is a literature review of previously published literature and does not involve any original data collection involving human or animal subjects. Therefore, ethical approval was not required.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.