Volume 5, Issue 9
September 2025
Moyamoya Syndrome in A 65-Year-Old With COVID-19: A Case Report
Juwain Y. Assahafi, Haneen A. Alzahrani, Wajd Y. Assahafi, Asmaa Y. Bohkari, Ali M. Alelyani, Aseel A. Aljunied, Abdulmoeen M. Alqarni
DOI: http://dx.doi.org/10.52533/JOHS.2025.50902
Keywords: Moyamoya disease, MMD, COVID-19, cerebrovascular disorder, Angiogenesis, stroke
Background: Moyamoya disease (MMD) is an unusual vasculopathy in which the blood vessels of the brain become occluded, resulting in the formation of collateral vessels, and leading to seizures or strokes. Moyamoya Syndrome (MMS) is a result of MMD caused by an underlying pathology. While it is uncommon for MMS to be associated with severe acute respiratory syndrome coronavirus 2 (COVID-19) infections, Moyamoya angiopathy (MMA) can be caused or exacerbated by inflammatory mediators.
Case presentation: Our case reports MMS in a 65-year-old male patient with COVID-19 and a medical background of diabetes, hypertension, and Parkinson’s disease. A magnetic resonance angiograph revealed changes in the microvasculature that fit the criteria of MMD. The patient was unresponsive to treatment and was declared dead due to acute respiratory distress syndrome, acute respiratory failure, post-arrest brain anoxia, and multi-organ failure.
Conclusion: It is difficult to conclude that COVID-19 can cause MMD with certainty; However, as MMD occurs secondary to immune dysregulation, there is enough evidence to emphasize the importance of considering the development of MMS secondary to COVID-19.
Introduction
Moyamoya disease is a rare, progressive cerebrovascular disorder characterized by stenosis and occlusion of the circle of Willis, especially at the internal carotid arteries, resulting in the compensatory development of tiny collateral “Moyamoya” vessels. These vessels were named “Moyamoya”, meaning ‘puff of smoke’ in Japanese, due to their smoky cloud appearance on angiography. Moyamoya vessels are frail and small, making them susceptible to thrombosis, bleeding, and aneurysms. As such, MMD manifests as transient ischemic attacks, hemorrhagic stroke, or seizures (1).
The etiology of MMD is unresolved, but some associations have been made. MMD was first reported in Japan, and it is more frequent in Asian populations. This is likely due to the prevalence of the Ring Finger Protein 213 (RNF-213) gene in East Asian populations, which is also found in 95% of familial MMD cases (2). The term MMD is used for genetic or idiopathic conditions; However, if the condition is associated with an underlying pathology, it is termed Moyamoya syndrome (1).
Moyamoya angiopathy is a type of immune reactive vasculitis that occurs due to injury to the cerebral vasculature caused by inflammatory mediators. Many cytokines as well as cytokine polymorphisms have been linked to collateral vessel formation in MMD. (3). Studies have elaborated that severe COVID-19 infection prompts immune dysregulation and cytokine storm, which can precipitate and aggravate MMA (4). However, the exact pathogenesis and neurological consequences of COVID-19 remain unclear.
In this report, we present the first case, to our knowledge, of Moyamoya disease in an adult patient with COVID-19 infection in Saudi Arabia to highlight how immune dysregulation and cytokine storm can precipitate or exacerbate MMD, as well as strengthen the hypothesis that inflammatory diseases can trigger or worsen MMA, necessitating vigilance in patients with severe systemic inflammation.
Case description
A bedridden 65-year-old Saudi male patient with a medical background of diabetes, hypertension, and Parkinson’s disease was brought to the emergency department (ED). He had a one-day history of a productive cough associated with subjective low-grade fever and small amounts of inoffensive yellowish sputum. There was no history of chest pain, dyspnea, palpitations, altered mental status, or constitutional symptoms, and other systemic review was unremarkable. His son denied any history of recent hospitalizations or contact with sick individuals. The patient did not smoke and did not receive any COVID-19 vaccination.
Upon general examination in the ED, the patient was conscious yet disoriented, with a Glasgow Coma Scale (GCS) of 9 (eye opening 3, motor response 4, and verbal response 2). He was afebrile with a body temperature of 36.8°C, tachycardiac with a pulse of rate of 118 BPM, hypotensive with a blood pressure of 66/46 mmHg, and tachypneic with a respiratory rate of 27 BPM and an oxygen saturation of 82% on room air.
Upon auscultation, the patient had bilateral crepitations with equal breath sounds. Cardiovascular examination showed normal heart sounds with no murmurs. His abdomen was neither distended nor tender, and his bowel sounds were normal. No other findings were apparent.
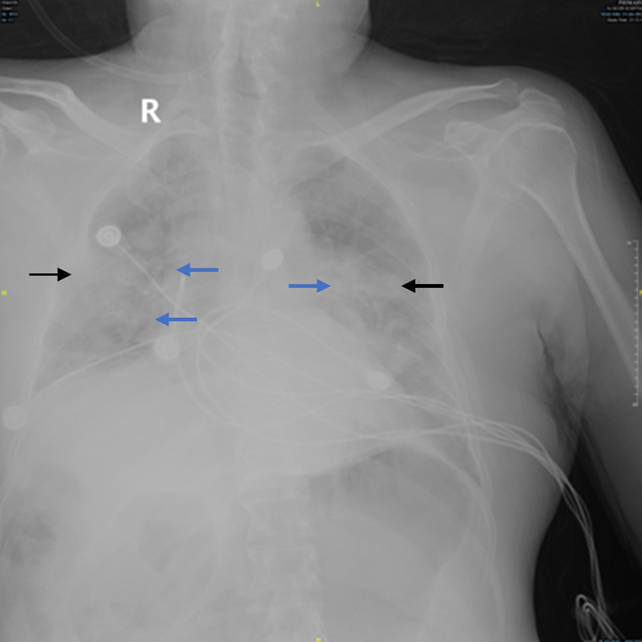
A septic workup and a COVID-19 nasopharyngeal swab were obtained. An anterior-posterior (AP) view of the chest X-ray showed bilateral opacities with peripheral infiltration (Figure 1). His Electrocardiogram showed a sinus rhythm with ST depression of the chest leads.
|
Table 1. Summary of laboratory findings upon presentation |
||
|
Patient’s Results |
Laboratory Reference Range |
|
|
Hemoglobin (g/L) |
14.8 |
120-150 |
|
Leukocytes: WBC count (109/L) |
8.58 |
4-11 |
|
Platelet count (109/L) |
604 |
150-400 |
|
Arterial blood gas |
||
|
pH |
7.29 |
7.35-7.45 |
|
PCO2 (MmHg) |
53.8 |
35-48 |
|
PO2 (MmHg) |
55 |
83-108 |
|
HCO3 (mmol/L) |
25.4 |
21-28 |
|
Alanine transaminase (U/L) |
63 |
14-60 |
|
Aspartate transaminase (U/L) |
43 |
15-37 |
|
Total bilirubin (µmol/L) |
8 |
0-18.7 |
|
Lactate dehydrogenase (U/L) |
300 |
|
|
Direct bilirubin (µmol/L) |
3 |
0-3 |
|
Albumin (g/L) |
33 |
34-50 |
|
Creatinine (µmol/L) |
53 |
44-90 |
|
Blood urea nitrogen (mmol/L) |
3.10 |
2.6-6.4 |
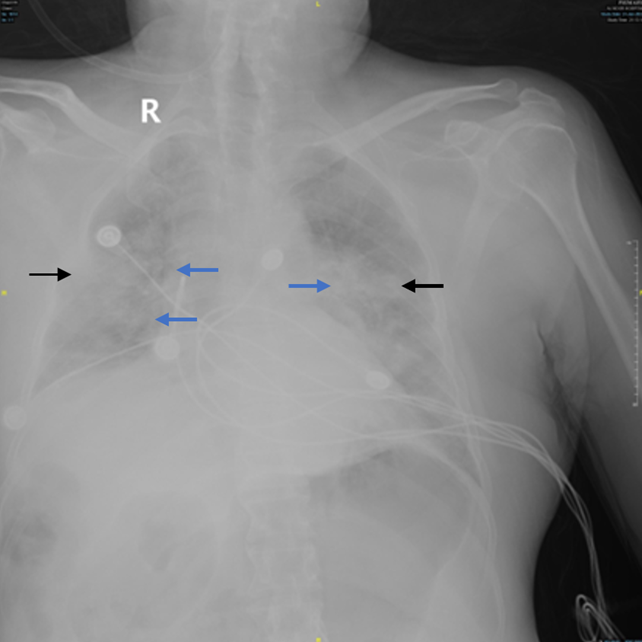
Figure 1: AP view chest X-ray taken upon admission. Bilateral opacities (black arrows) and peripheral infiltration (blue arrows) are noted.
While in the ED, the patient suffered a cardiac arrest. Cardiopulmonary resuscitation (CPR) was performed according to the American Heart Association Advanced Cardiac Life Support guidelines and return of spontaneous circulation (ROSC) was achieved 10 minutes after resuscitation. The patient was stabilized and shifted to the radiology department shortly afterwards, where a computed tomography (CT) scan of the brain was done without contrast. The CT scan did not show any features of acute brain injury. A pulmonary embolism (PE) was also suspected, and a CT scan of the chest showed bilateral ground glass appearance without acute PE (Figure 2).
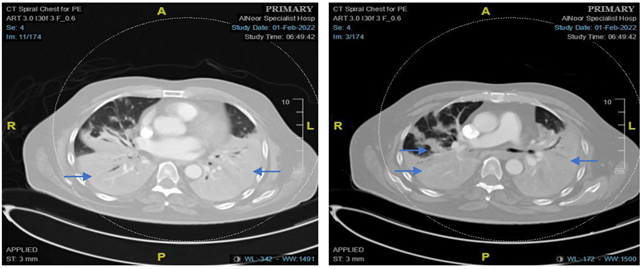
Figure 2: Axial spiral computed tomography scan of the chest with contrast showing bilateral consolidation with air bronchogram.
He was admitted to an isolation room in the intensive care unit (ICU) as a case of bilateral pneumonia suspected to be secondary to a COVID-19 infection complicated by septic and/or cardiogenic shock. In the ICU, he was started on empirical antibiotics and ionotropic support. Given the ECG changes and cardiac arrest, the possibility of acute coronary syndromes couldn’t be ruled out. A bedside echocardiography reported an ejection fraction of 50% with mild tricuspid and mitral regurgitation, and no other significant findings.
A reverse transcriptase-polymerase chain reaction (RT-PCR) was positive for COVID-19 with no growth reported on blood and urine cultures. The patient’s laboratory workup exhibited persistent leukocytosis with declining renal functions (Figure 3).
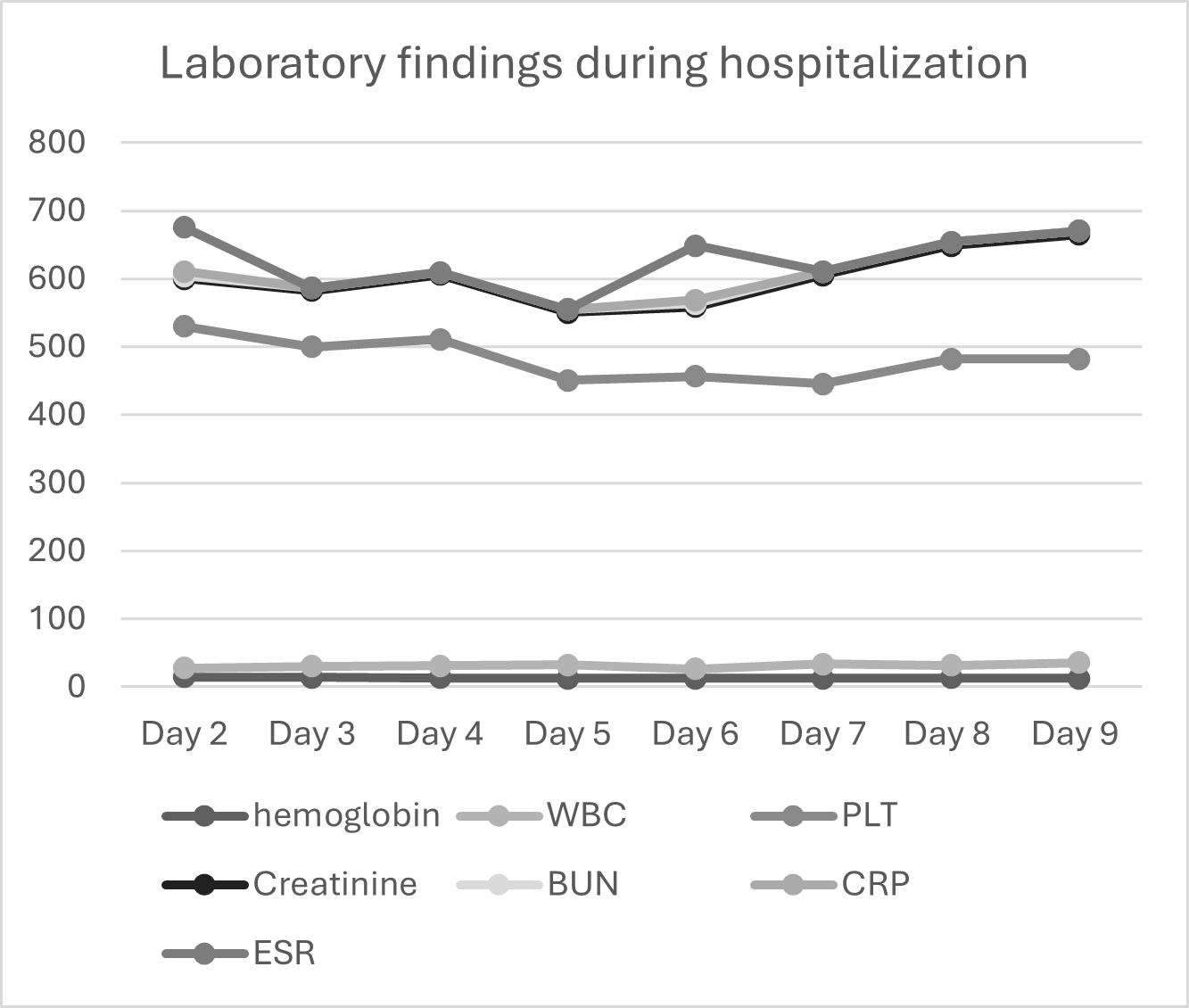
Figure 3: Summary of laboratory findings during hospitalization.
His condition worsened with increased requirements of inotropic and ventilatory support. Follow up chest radiography showed subtle improvement of lung aeration followed by progressive worsening infiltration in keeping with acute respiratory distress syndrome (ARDS) (Figure 4).
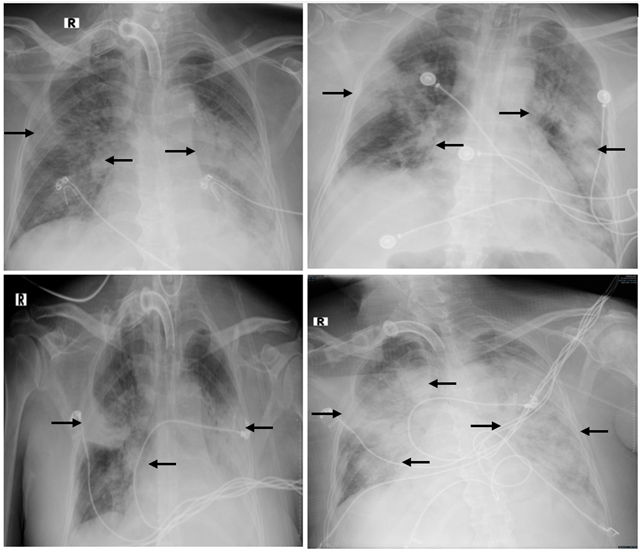
Figure 4: A) Repeated chest x-ray AP view showing bilateral infiltration more on the left side. B) Follow up chest x-ray AP view showing worsening bilateral infiltration. C) AP view showing slight resolution of the right side. D) AP view of the chest showing worsening bilateral infiltration in keeping with ARDS.
He also failed to gain consciousnesses despite being off of sedative agents, magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the brain performed to assess for anoxic brain injury, both of which reported deep watershed infarctions at bilateral anterior cerebral artery (ACA)/middle cerebral artery (MCA) and MCA, posterior cerebral artery territories (PCA)with hemorrhagic transformation, all which fit the criteria of MMD (Figure 5).
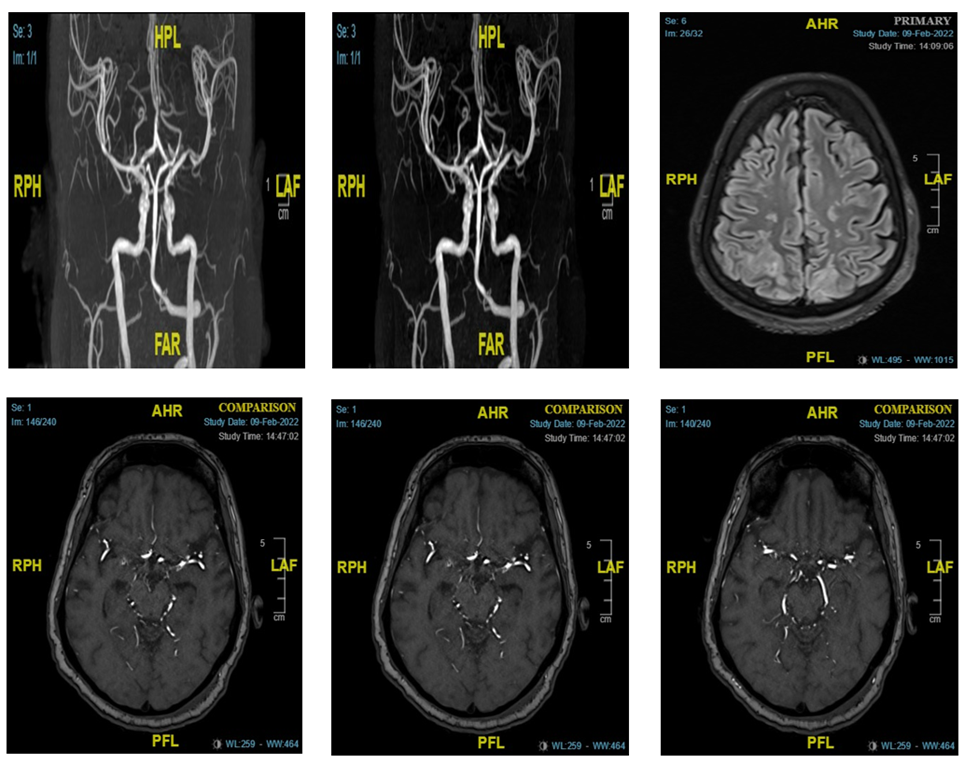
Figure 5: MRI with displayed findings of watershed infarctions at bilateral ACA/MCA and MCA, PCA territories with hemorrhagic transformation fulfilling the criteria of MMD.
After a period in the ICU, the patient’s condition kept deteriorating. He was unresponsive to treatment offered and was declared dead as a result of ARDS, acute respiratory failure, post-arrest brain anoxia, and multi-organ failure.
Discussion
This case reports the first case of MMD in an adult patient with COVID-19 infection in Saudi Arabia to the best of our knowledge.
Although the etiology of MMD is unknown, there is increasing evidence highlighting the RNF-213 gene on chromosome 17q25.3 as a susceptibility factor (2, 4). Okhubo et. al reported that RNF-213 is a target for inflammatory cytokines (5). While the specific pathogenesis and neurological consequences concomitant to COVID-19 infection are not fully understood, studies on the effect of severe COVID-19 infections have shown that COVID-19 triggers immune dysregulation as well as heightened levels of inflammatory cytokines, which could interact with RNF-213, leading to subsequent MMD (3, 6). Furthermore, COVID-19 has been linked to localized intravascular coagulopathy, inflammatory cytokine release, and endothelial dysfunction, which may also precipitate MMD by increasing angiogenesis-related factors (7). These angiogenesis-related factors have been demonstrated in other cases in which patients developed coagulopathies secondary to COVID-19 (8). Additionally, COVID-19 is associated with hypercoagulability and thrombosis, which may increase the likelihood of developing transient ischemic attacks or hemorrhagic strokes in cases with existing MMD.
Moyamoya vasculopathy has been observed following other inflammatory diseases and infections (9, 10). Most cases of post-infective MMS were secondary to bacterial meningitis (11, 12). Despite the etiological difference, these studies also considered autoimmune processes and inflammation as the basis of angiogenesis and coagulopathy. During inflammatory processes, excessive cytokine release can alter vascular function and structure through autoimmune activation and endothelial damage. Cytokines also influence apoptosis-related signaling pathways, which may initiate the apoptosis of endothelial cells and subsequently weaken the walls of blood vessels, leading to vascular remodeling (13). “Cytokine storm”, a hyperinflammatory state characterized by excessive cytokine release, has been elucidated as a key feature of COVID-19 (6). This suggests a link between the inflammatory response to COVID-19 and MMD. Cases reporting MMD concomitant to COVID-19 have also suggested this link (10,14-16).
Other cases reports discussing MMD and COVID-19 infection have emphasized the role of the vaccine or vaccine boosters as a heralding factor; However, in this report, the patient had not received a vaccination (10, 15).
The strength of this paper lies in it reporting an early occurrence of MMD in an adult patient with COVID-19 infection in Saudi Arabia, thus enabling the understanding of the concomitant presentation of the two. This paper highlights the significance of considering consequent MMD in COVID-19 patients. While it is difficult to definitively claim that COVID-19 can cause MMD, we believe that the association is valid in the reported case due to the initial absence of MMD signs, in addition to the timing between the COVID-19 infection and the presentation of MMD.
This study has some limitations. Firstly, it is difficult to establish a causal relationship by reporting the case of only one patient. Secondly, it is impossible to retrospectively eliminate the probability of pre-existing MMD unmasked by COVID-19. Finally, we cannot eliminate the potential influence of the patient’s existing diabetes, hypertension, and Parkinson’s disease on the development of MMD.
Conclusion
This report highlights the potential link between COVID-19 and MMS. It is difficult to conclude that COVID-19 can cause MMS with certainty; However, there is enough evidence to emphasize the importance of considering the development of MMD secondary to COVID-19. Patients with severe COVID-19 should be closely monitored to detect early signs of MMD, which, without rapid management, could be life-threatening.
Disclosure
Conflict of interest
The authors declare no conflict of interest.
Funding
The authors declare no funding.
Data availability
All patient data has been presented within the paper. Any additional queries can be assisted by contacting the corresponding author.
Patient consent
Written informed consent was obtained from the patient’s next of kin for publication of this case. The ethics committee’s approval was not required for publication, as this is a case report.