Volume 5, Issue 9
September 2025
A Case Report of Acute Myocardial Infarction in a Patient with History of Herpes Zoster Infection
Mohammed A. Alshehri, Abdullah M. Alshehri
DOI: http://dx.doi.org/10.52533/JOHS.2025.50903
Keywords: Herpes zoster, Herpes zoster vaccination, Myocardial infarction, Acute coronary syndrome
Background: Patients with history of herpes zoster (HZ) infection were found to have an increased long-term risk of major cardiovascular events. The association between myocardial infarction (MI) and HZ infection is an area of rising research interest. While HZ infection primarily has both dermatological and neurological manifestations, studies have increasingly shown that it may also be linked to increased cardiovascular risk, particularly acute MI and stroke.
Case presentation: Here we report a case of acute MI in a 68-year-old male patient who has a history of HZ infection and received the booster dose of HZ vaccine (Shingrix) 24 hours prior to his presentation with acute MI. Moreover, this case report of acute myocardial injury secondary to acute None-ST segment elevation MI following Shingrix vaccine in a patient with history of HZ infection helps in establishing the relationship between HZ infection and its cardiovascular effects.
Conclusion: To conclude, health care providers should be aware of the increased risk of cardiovascular events in patients with history of HZ infection and the rare side effect of vaccines to properly evaluate patient who presented with suspicious symptoms following vaccine administration.
Introduction
Herpes zoster, typically presents with pain described as burning or stabbing, followed by a vesicular rash in the affected dermatome; location of symptoms depends on the affected nerve. It’s a viral syndrome caused by reactivation of the varicella-zoster virus. After an episode of varicella (chickenpox), the varicella-zoster virus remains latent in the nervous system. HZ infection could affect adults or elderly (1). In individuals aged ≥50 years, the cumulative incidence of HZ infection has been reported to range from 2.9–19.5 cases per 1,000 population, with an incidence rate between 5.23–10.9 cases per 1,000 person-years. A trend of increasing incidence of HZ with increasing age was observed (2). HZ infection could occur in patients due to different risk factors or triggers that include emotional stress, usage of immunosuppressant medications, acute or chronic illnesses, exposure to the virus and presence of malignancy (1). HZ infection is clinically diagnosed with burning pain, characteristic morphology, and typical distribution. But for some cases tests that include Tzanck smear, Varicella-zoster virus (VZV) specific IgM antibody, Direct fluorescent antibody testing when there is eye involvement and PCR testing could be done to help in the diagnosis (1). As for the treatment of HZ infections antiviral therapy regimens of acyclovir, valacyclovir and famciclovir are prescribed for patients to accelerate the resolution of lesions, decreases acute pain and help to prevent post-herpetic neuralgia especially in elderly patients (1).
Patients with a history of HZ infection were found to have an increased long-term risk of major cardiovascular events (3). These findings suggest that there are long-term implications of HZ infection and indicate the importance of public health efforts for prevention. For this reason, vaccination against HZ has emerged as a crucial public health intervention. In the Kingdom of Saudi Arabia, the prophylactic HZ vaccine which has been licensed is the recombinant subunit glycoprotein E vaccine which is called Shingrix.
Here we report a case of acute myocardial infarction (MI) in elderly male patient who has a history of HZ infection and received the poster dose of Shingrix vaccine 24 hours prior to his presentation with acute MI.
Case Presentation
A 68-year-old male presented to the emergency department complaining of compressing chest pain, dizziness, and feeling of generalized fatigue. The patient is a known case of hypertension, with no history of cardiac disease, diabetes, hyperlipidemia, or smoking. He had a history of herpes zoster infection one year ago. One day prior to presentation, he received the second dose of the recombinant Shingrix vaccine. ECG was done in the emergency department which showed normal sinus rhythm with nonspecific ST-T changes, but troponin-T was elevated (700 ng). Patient was diagnosed as acute non-ST-elevation myocardial infarction (NSTEMI) and received Aspirin 300 mg, loaded with Clopidogrel 300 mg and started on Therapeutic LMWH (Enoxaparin sodium) 80 Subcutaneously every 12 hours and admitted to the coronary care unit.
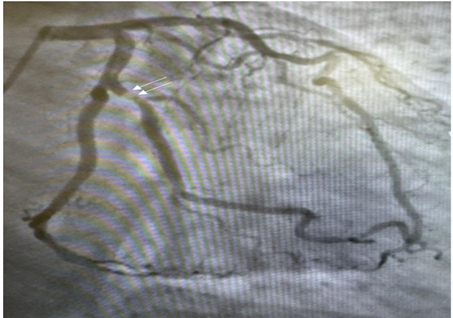
Then next day, the patient underwent selective coronary angiography via the right Radial Artery, using 6F XB 3.0, JR4 Diagnostic catheters in multiple projections. It showed dominant right coronary artery (RCA) which was normal, normal Left main (LM) and Left Anterior Descending (LAD). The Left circumflex artery had no significant lesion, but the First obtuse marginal branch (OM1) had a severe 90% hazy proximal Lesion (Figure 1).
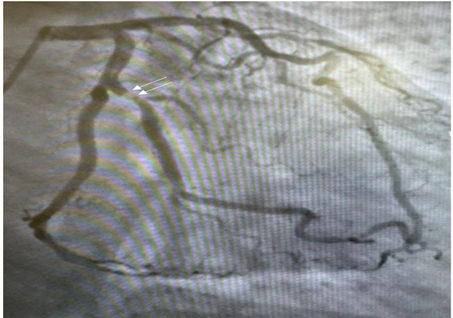
Figure 1: Coronary angiogram, RAO view showing First obtuse marginal branch (OM1) with severe 90% hazy.
Percutaneous coronary intervention (PCI) was done to OM1 using the 6F XB 3.0 guide catheter to engage the LM and then 0.014-inch Sion Blue wire was advanced across the lesion to distal OM1 following which the lesion was pre-dilated using 2.5mm x 10mm Sapphire ballon and stented using a 3.5 x 23mm Xience stent and post dilated using 3.75mm x 15mm NC Sapphire. Repeat angiography revealed good deployment of the stent, no significant residual stenosis, no complications and TIMI III flow distally (Figure 2).

Figure 2: Coronary angiogram, RAO view showing the same vessel First obtuse marginal branch (OM1) Post proximal Lesion.
The patient was transferred to the CCU, where he remained for 48 hours. During his stay, he was stable and asymptomatic, and he was discharged with a follow-up appointment in the cardiology clinic after 2 weeks. There were no complications in this patient on follow up.
Discussion
The risk of cardiovascular events among patients with past history of HZ infection was shown in multiple studies (3, 4). A study that was conducted by Curhan et al, that covered 3 large cohort studies showed that history of HZ infection was significantly and independently associated with higher long-term risk of coronary heart disease (CHD) compared to those without a history of HZ infection. CHD was defined as nonfatal or fatal MI, fatal CHD, or coronary revascularization procedure. The multivariable-adjusted hazard ratios for CHD were 1.13 for 1–4 years, 1.16 for 5–8 years, and 1.25 for 9–12 years following an HZ infection episode. (3). A cohort study done by Horev et al., showed that the risk of major adverse cardiac and cerebrovascular events was 19% higher among HZ infection sufferers in the first year of follow up, and this risk was sustained for at least 4.4 years following episode (4). Another cohort study conducted by Wang et al, showed that even after adjusting multiple potential confounding factors like hypertension, diabetes mellitus, hyperlipidemia, HZ infection remained independently associated with the development of acute coronary syndrome (ACS) (5). Another retrospective cohort study done by Parameswaran et al, showed that HZ infection was linked with 1.35-fold increased risk of developing MI within the first 30 days postinfection. History of MI, male sex, history of heart failure, age ≥50 years, human immunodeficiency virus, peripheral vascular disease, renal disease and prior cerebrovascular accident increased odds of MI 30 days postinfection with herpes zoster (6). Furthermore, an analysis of administrative data collected between 2002 and 2013 in Korea done by Kim et al, showed that patients with HZ infection (N=23,213) had a raised risk of a composite cardiovascular endpoint, stroke and acute MI by 41%, 35%, and 59%, respectively compared to the group that did not have HZ infection (7). Another population-based study by Wu et al was performed in Taiwan from 1998 to 2008 which identified 19,483 patients with HZ infection and 77,932 without HZ infection. Both cohorts were followed until the end of 2010 to measure the incidence of coronary artery disease and arrhythmia. The coronary artery disease incidence in the HZ cohort was 1.16-fold higher than that in the non-herpes zoster cohort. On the other hand, the incidence of arrhythmia was 1.17-fold greater in the herpes zoster cohort than in the non-herpes zoster cohort (8). A study done by Nagel et al showed that the pathogenesis of VZV infection effect on arteries presented as: disrupted internal elastic lamina; a thickened intima composed of myofibroblasts expressing alpha-smooth muscle actin, potentially contributing to luminal narrowing/occlusion and ischemic stroke; and a paucity of medial smooth muscle cells leading to loss of vessel wall integrity. Our Patient had a history of HZ infection one year prior to his acute coronary event which might be a predisposing factor for his presentation (9). According to US Centers for Disease Control and Prevention and a systemic review done by Parmar et al. Serious adverse diseases were related to herpes vaccinations including cardiac effects such as pericarditis, myocarditis and noncardiac diseases such as febrile seizures, anaphylaxis, Immune thrombocytopenia, meningitis, encephalitis, and Guillain-Barré syndrome (10, 11). Furthermore, a unique case report done by Puram et al. of a 60-year-old man who presented with Hypersensitivity vasculitis after receiving the Shingrix vaccine could raise suspicion of the effect of vaccination on our patient’s presentation (12). Our patient had the second booster dose of Shingrix vaccine one day prior to his acute myocardial injury which could be a contributing factor to his cardiovascular event.
Conclusion
This case report of acute myocardial injury secondary to acute None-ST segment elevation MI in a patient with history of HZ infection following Shingrix vaccine helps in establishing the relationship between HZ infection and its cardiovascular effects. Healthcare providers should be aware of the increased risk of cardiovascular events in patients with history of HZ infection and the rare side effect of vaccines to properly evaluate patient who presented with suspicious symptoms following Shingrix vaccine administration.
Abbreviations
HZ: Herpes zoster
NSTEMI: Non-ST elevation myocardial infarction
TIMI: Thrombolysis In Myocardial Infarction
CCU: Coronary care unit
MI: Myocardial Infarction
CHD: Coronary Heart Disease
ACS: Acute coronary syndrome
VZV: Varicella zoster virus
Acknowledgements
There are no acknowledgements.
Disclosure
Statement
The authors declare that they have no conflict of interests.
Funding
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical Consideration
Consent to the anonymous use and publication of their medical information and video materials was obtained from the patient.
Data Availability
The contributions presented in the study are included in the article further inquiries can be directed to the corresponding author.
Author Contribution
MA drafted the article and contributed to editing, revision of the study and literature searches.
AA contributed to revision of the article and took the responsibility of communicating with the patient.
Both authors approved submission of the manuscript.